In addition to following standards of care, nurses must also follow related federal and state laws. Criminal law is a system of laws that punishes individuals who commit crimes. Crimes are classified as felonies, misdemeanors, and infractions. Conviction for a crime requires evidence to show the defendant is guilty beyond a shadow of doubt. This means the prosecution must convince a jury there is no reasonable explanation other than guilty that can come from the evidence presented at trial. See Figure 5.1[1] for an illustration of a criminal case being tried in front of a jury. Civil law focuses on the rights, responsibilities, and legal relationships between private citizens, and involves compensation to the injured party. A person bringing the lawsuit is called the plaintiff, and the parties named in the lawsuit are called defendants.[2]

Civil law includes torts. A tort is an act of commission or omission that gives rise to injury or harm to another and amounts to a civil wrong for which courts impose liability. Tort law exists to compensate clients injured by negligent practice, provide corrective judgment, and deter negligence with consequences of action or inaction.[3]
Two categories of torts affecting nursing practice are intentional torts and unintentional torts. Intentional torts are wrongs that the defendant knew (or should have known) would be caused by their actions. Examples of intentional torts include assault, battery, false imprisonment, slander, libel, and breach of privacy or client confidentiality. Unintentional torts occur when the defendant’s actions or inactions were unreasonably unsafe. Unintentional torts can result from acts of commission (i.e., doing something a reasonable nurse would not have done) or omission (i.e., failing to do something a reasonable nurse would do). Examples of torts affecting nursing practice are discussed in further detail in the following subsections.[4]
Assault and Battery
Assault and battery are intentional torts. Assault is defined as intentionally putting another person in reasonable apprehension of an imminent harmful or offensive contact. Battery is defined as intentional causation of harmful or offensive contact with another person without that person’s consent. Physical harm does not need to occur in order to be charged with assault or battery. Battery convictions are typically misdemeanors but can be felonies if serious bodily harm occurs.[5]
An example related to assault and battery in health care is the patient’s right to refuse treatment. For example, a hospitalized patient can refuse to take prescribed medication. If a nurse forcibly administers medication without a patient’s consent, it could be ruled assault or battery in a court of law. However, forcible administration of a medication based on a provider’s order may be justified in an emergency situation to prevent imminent harm to oneself or others.[6]
False Imprisonment
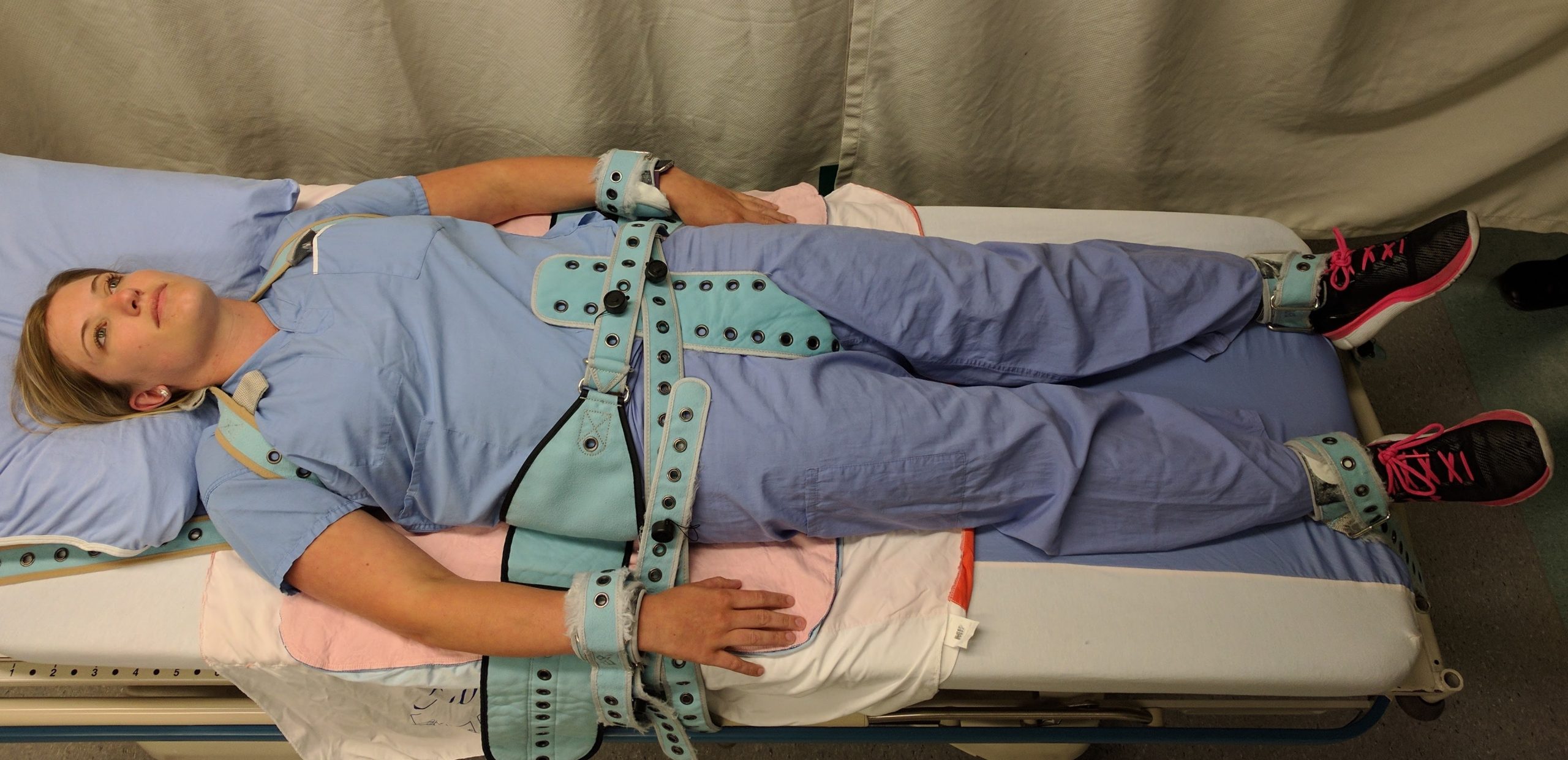
False imprisonment is an intentional tort. False imprisonment is defined as an act of restraining another person and causing that person to be confined in a bounded area. An example of possible false imprisonment in health care is the use of restraints. See Figure 5.2[7] for an image of a simulated client in full physical medical restraints. Restraints can be physical, chemical, or verbal. Nurses must vigilantly follow agency policies related to the use of physical restraints and monitor clients who are restrained. Chemical restraints include administration of PRN medications such as benzodiazepines and require clear documentation supporting their use. Verbal threats to keep an individual in an inpatient environment can also qualify as false imprisonment and should be avoided. Additional information regarding the use of restraints is discussed in the “Patient Rights” section.
Privacy and Confidentiality
Breaching privacy and confidentiality are intentional torts. Confidentiality is the right of an individual to have personal, identifiable medical information, referred to as protected health information, kept private. Protected Health Information (PHI) is defined as individually identifiable health information, including demographic data, that relates to the individual’s past, present, or future physical or mental health or condition; the provision of health care to the individual; and the past, present, or future payment for the provision of health care to the individual.[8]
Confidentiality is a right protected by the Health Insurance Portability and Accountability Act (HIPAA). HIPAA was enacted in 1996 and was prompted by the need to ensure privacy and protection of personal health records in an environment of electronic medical records and third-party insurance payers. There are two main sections of HIPAA law: the Privacy Rule and the Security Rule. The Privacy Rule addresses the use and disclosure of individuals’ health information. The Security Rule sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. HIPAA regulations extend beyond medical records and apply to client information shared with others. Therefore, all types of client information and data should be shared only with health care team members who are actively providing care to them. For example, when applying HIPAA to mental health inpatient settings, nurses may not answer in the affirmative if someone calls and asks if an individual has been admitted to the unit.[9] See Figure 5.3[10] for a depiction of confidentiality.

There are specific circumstances in which HIPAA does not apply. For example, nurses have a duty to warn and protect, are mandated reporters of suspected abuse or neglect, and are required to share specific information reported by minors with authorities or their parents.
Duty to Warn and Protect
Most states have laws regarding the duty to protect third parties from potential life threats. Nurses and other mental health professionals have a duty to warn and protect third parties when they may be in danger from a patient. This duty falls outside of HIPAA regulations. This includes assessing and predicting the patient’s threat of violence towards another person or groups of people and taking action to protect the identified victims.[11]
Mandatory Reporting of Suspected Abuse or Neglect
HIPAA does not apply to reporting the suspected neglect or abuse of children, adults at risk, or older adults. Many states require health professionals to report suspected neglect or abuse. State laws vary, but they generally include a definition of abuse, a list of people required to report abuse, and the government agency designated to receive and investigate the reports. Nurses and other health professionals are referred to as mandated reporters because they are required by state law to report suspected neglect or abuse of children, adults at risk, and the elderly. Adults at risk are adults who have a physical or mental condition that impairs their ability to care for their own needs.
For example, in Wisconsin, suspected neglect or abuse is reported to Child Protective Services (CPS), Adult Protective Services, or law enforcement. Nurses should be aware of the country or state agencies to whom they should report suspected abuse. See the following box for additional information.
Read additional information about signs of child and elder abuse in the “Trauma, Abuse, and Violence” chapter.
Read more about protective services in your state. Here are links to Wisconsin’s Child Protective Services and Adult Protective Services.
Find resources in your area for reporting suspected child abuse at ChildHelp National Child Abuse Hotline or elder abuse at the National Adult Protective Services Association website.
Conditional Confidentiality for Minors
“Conditional confidentiality” applies to minors under the age of 18. State laws determine what information is considered confidential and what requires reporting to law enforcement or Child Protective Services, such as child abuse, gunshot or stabbing wounds, sexually transmitted infections, abortions, suicidal ideation, and homicidal ideation. Some state laws make it optional for clinicians to inform parents/guardians if their child is seeking services related to sexual health care, substance use, or mental health care. Nurses should be aware of the state laws affecting the confidentiality of child and adolescent care in the state in which they are practicing.[12]
Slander and Libel
Slander and libel are intentional torts. Defamation of character occurs when an individual makes negative, malicious, and false remarks about another person to damage their reputation. Slander is spoken defamation and libel is written defamation. Nurses must take care in their oral communication and documentation to avoid defaming clients or coworkers.[13]
Fraud
Fraud is an intentional tort that occurs when an individual is deceived for personal gain. A nurse may be charged with fraud for documenting interventions not performed or for altering documentation to cover up an error. Fraud can result in civil and criminal charges, as well as suspension or revocation of a nurse’s license.[14]
Negligence and Malpractice
Negligence and malpractice are unintentional torts. Negligence is the failure to exercise the ordinary care a reasonable person would use in similar circumstances. Wisconsin civil jury instruction states, “A person is not using ordinary care and is negligent, if the person, without intending to do harm, does something (or fails to do something) that a reasonable person would recognize as creating an unreasonable risk of injury or damage to a person or property.” Malpractice is a specific term used for negligence committed by a health professional with a license.
Elements of Malpractice
Clients bringing a malpractice lawsuit must be able to demonstrate to the court that their interests were harmed. Most malpractice lawsuits name physicians or hospitals as defendants, although nurses can be individually named. Employers can be held liable for the actions of their employees.
Malpractice lawsuits are concerned with the legal obligations nurses have to their patients to adhere to current standards of practice. These legal obligations are referred to as the duty of reasonable care. Nurses are required to adhere to standards of practice when providing care to patients they have been assigned. This includes following organizational policies and procedures, maintaining clinical competency, and confining their activities to the authorized scope of practice as defined by their state’s Nurse Practice Act. Nurses also have a legal duty to be physically, mentally, and morally fit for practice. When nurses do not meet these professional obligations, they are said to have breached their duties to patients.[15]
All of the following elements must be established in a court of law to prove malpractice[16]:
- Duty: A nurse-client relationship exists.
- Breach: The standard of care was not met and harm was a foreseeable consequence of the action or inaction.
- Cause: Injury was caused by the nurse’s breach.
- Harm: Injury resulted in damages.
Duty
In the work environment, a duty is created when the nurse accepts responsibility for a patient and establishes a nurse-patient relationship. This generally occurs during inpatient care upon acceptance of a handoff report from another nurse. Outside the work environment, a nurse-patient relationship is created when the nurse volunteers services. Mandatory reporting and duty to warn and protect are additional examples of a nurse’s duty.[17]
Breach of Duty
The second element of malpractice is breach of duty. After a plaintiff has established the first element in a malpractice suit (i.e., the nurse owed a duty to the plaintiff), the plaintiff must demonstrate that the nurse breached that duty by failing to comply with the duty of reasonable care. To demonstrate that a nurse breached their duty to a patient, the plaintiff must prove the nurse deviated from acceptable standards of practice. The plaintiff must establish how a reasonably prudent nurse in the same or similar circumstances would act and then show how the defendant nurse departed from that standard of practice. The plaintiff must claim the nurse did something a reasonably prudent nurse would not have done (an act of commission) or failed to do something a reasonable nurse would have done (an act of omission).[18]
Experts are needed during court hearings to explain things outside the knowledge of non-nurse jurors. In reaching their opinions, experts review many materials, including the state’s Nurse Practice Act and organizational policies, to determine whether the nurse adhered to them. To qualify as a nurse expert, the person testifying must have relevant experience, education, skill, and knowledge. Medical malpractice trials take place primarily in state courts, so experts are deemed qualified based on state requirements.[19]
Cause
The third element of malpractice is cause. After the plaintiff has established that the nurse owed a duty to a patient and then breached that duty, they must then demonstrate that damages or harm were caused by that breach. Plaintiffs cannot prevail by only demonstrating the nurse departed from acceptable standards of practice, but also must prove that such departures were the cause of any injuries. Additionally, nurses are held accountable for foreseeability, meaning a nurse of ordinary skill, care, and diligence could anticipate the risk of harm of departing from standards of practice in similar circumstances.[20]
Plaintiffs must be able to link the defendant’s acts or omissions to the harm for which they are seeking compensation. This requires expert testimony from a physician because it requires a medical diagnosis. Unlike criminal cases, where the standard of proof is “beyond reasonable doubt,” the elements of a malpractice lawsuit must be proven by a “preponderance of evidence.” Expert testimony is required to demonstrate “medical certainty” that the nurse’s breach was the cause of an actual injury.[21]
Harm
The fourth element of malpractice is harm. In a civil lawsuit, after a plaintiff has established the nurse owed a duty to the patient, breached that duty, and injury was caused by the nurse’s breach, they must prove the injury resulted in damages. They request compensation for what they have lost.[22]
There are several types of injuries for which patients or their representatives seek compensation. Injuries can be physical, emotional, financial, professional, marital, or any combination of these. Physical injuries include loss of function, disfigurement, physical or mental impairment, exacerbation of prior medical problems, the need for additional medical care, and death. Economic injuries can include lost wages, additional medical expenses, rehabilitation, durable medical expenses, the need for architectural changes to one’s home, the loss of earning capacity, the need to hire people to perform tasks the plaintiff can no longer do, and the loss of financial support. Emotional injuries can include psychological damage, emotional distress, or other forms of mental suffering.[23]
Determining the specific amount a plaintiff needs can require expert witness testimony from a person known as a life care planner who is trained in analyzing and evaluating medical costs, as well as the subjective determination of a jury. Damages fall into several categories, including compensatory (economic) damages, noneconomic damages, and punitive damages.[24]
Implications for Nurses
Nurses defending themselves against allegations of professional malpractice must demonstrate that their actions conformed with accepted standards of practice. They must convince a jury they acted as a reasonably prudent nurse would have in the same or similar circumstances. Nurses should follow these practices to avoid allegations of malpractice[25]:
- Practice according to current standards of practice.
- Adhere to organizational policies and procedures. The standard of practice is to adhere to agency policy. Failing to do so creates an assumption of departure from standards.
- Document in a manner that permits accurate reconstruction of patient assessments and the sequence of events, especially when notifying providers regarding clinical concerns.
- Maintain competence through continuing education, participation in professional conferences, membership in professional organizations, and subscriptions to professional journals.
- When using an interpreter, ensure that properly trained interpreters are used and document the name of the interpreter. The use of family, friends, or other untrained interpreters is unsafe practice and is not consistent with acceptable standards of practice.
- Maintain professional boundaries. Personal relationships with patients or their families can be red flags for juries and can be viewed as evidence of departure from professional standards.
- Engage the chain of command with patient concerns and pursuing concerns to resolution.
Read more about actual nursing malpractice cases in the “Frequent Allegations and SBON Investigations” section of the “Legal Implications” chapter in Open RN Nursing Management and Professional Concepts.
Disciplinary Action by the Board of Nursing
In addition to being held liable in a court of law, nurses can have their licenses suspended or revoked by the State Board of Nursing (SBON) for unsafe nursing practice. The SBON governs nursing practice according to that state’s Nurse Practice Act to protect the public through licensure, education, legislation, and discipline. A nursing license is a contract between the state and the nurse in which the licensee agrees to provide nursing care according to that state’s Nurse Practice Act. Deviation from the Nurse Practice Act is a breach of contract that can lead to limited or revoked licensure. Nurses must practice according to the Nurse Practice Act of the state in which they are providing client care.[26]
A nurse may be named in a board licensing complaint called an allegation. Allegations can be directly related to a nurse’s clinical responsibilities, or they can be nonclinical (such as operating a vehicle under the influence of a substance, exhibiting unprofessional behavior, or committing billing fraud). A complaint can be filed against a nurse by anyone, such as a patient, a patient’s family member, a colleague, or an employer. It can also be filed anonymously. After a complaint is filed, the SBON follows a disciplinary process that includes investigation, proceedings, board actions, and enforcement. The process can take months or years to resolve, and it can be costly to hire legal representation.[27]
Disciplinary actions by the SBON may include the following[28]:
- Reprimand: The licensee receives a public warning for a violation.
- Limitation of License: The licensee has conditions or requirements imposed upon their license, their scope of practice, or both.
- Suspension: The license is completely and absolutely withdrawn and withheld for a period of time, including all rights, privileges, and authority previously conferred by the credential.
- Revocation: The license is completely and absolutely terminated, as well as all rights, privileges, and authority previously conferred by the credential.
- Administrative Warning: A warning is issued if the violation is of a minor nature, or a first occurrence and the warning will adequately protect the public. The issuance of an administrative warning is public information but the reason for issuance is not.
- Remedial Education Order: A remedial education order is issued when there is reason to believe that the deficiency can be corrected with remedial education, while sufficiently protecting the public.
Find and review your state’s Nurse Practice Act.
- “Courtroom Trial with Judge, Jury - Vector Image” designed by WannaPik is licensed under CC0 ↵
- Brous, E. (2019). The elements of a nursing malpractice case, part 1: Duty. American Journal of Nursing, 119(7), 64–67. https://doi.org/10.1097/01.NAJ.0000569476.17357.f5 ↵
- Wis. JI—Civil 1005. (2016). https://wilawlibrary.gov/jury/civil/instruction.php?n=1005 ↵
- Brous, E. (2019). The elements of a nursing malpractice case, part 1: Duty. American Journal of Nursing, 119(7), 64–67. https://doi.org/10.1097/01.NAJ.0000569476.17357.f5 ↵
- Brous, E. (2019). The elements of a nursing malpractice case, part 1: Duty. American Journal of Nursing, 119(7), 64–67. https://doi.org/10.1097/01.NAJ.0000569476.17357.f5 ↵
- Fry, S. T. (1989). The role of caring in a theory of nursing ethics. Hypatia, 4(2), 87-103. https://doi.org/10.1111/j.1527-2001.1989.tb00575.x ↵
- “PinelRestaint.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- Wis. JI—Civil 1005. (2016). https://wilawlibrary.gov/jury/civil/instruction.php?n=1005 ↵
- Wis. JI—Civil 1005. (2016). https://wilawlibrary.gov/jury/civil/instruction.php?n=1005 ↵
- “Concept of Data Privacy And Policy Illustration” by Delesign Graphics at Iconscout is licensed under CC BY 4.0 ↵
- Fry, S. T. (1989). The role of caring in a theory of nursing ethics. Hypatia, 4(2), 87-103. https://doi.org/10.1111/j.1527-2001.1989.tb00575.x ↵
- Nurses Service Organization and CNA Financial. (2020, June). Nurse professional liability exposure claim report (4th ed.). https://www.nso.com/Learning/Artifacts/Claim-Reports/Minimizing-Risk-Achieving-Excellence ↵
- Wis. JI—Civil 1005. (2016). https://wilawlibrary.gov/jury/civil/instruction.php?n=1005 ↵
- Wis. JI—Civil 1005. (2016). https://wilawlibrary.gov/jury/civil/instruction.php?n=1005 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Teoli and Ghassemzadeh and is licensed under CC BY 4.0 ↵
- American Nurses Association. (2012). Position statement: Reduction of patient restraint and seclusion in health care settings. https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/reduction-of-patient-restraint-and-seclusion-in-health-care-settings/ ↵
- American Nurses Association. (2012). Position statement: Reduction of patient restraint and seclusion in health care settings. https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/reduction-of-patient-restraint-and-seclusion-in-health-care-settings/ ↵
- American Nurses Association. (2012). Position statement: Reduction of patient restraint and seclusion in health care settings. https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/reduction-of-patient-restraint-and-seclusion-in-health-care-settings/ ↵
A system of laws that punishes individuals who commit crimes.
Rights, responsibilities, and legal relationships between private citizens and involves compensation to the injured party.
A person bringing the lawsuit.
The parties named in the lawsuit.
An act of commission or omission that gives rise to injury or harm to another and amounts to a civil wrong for which courts impose liability.
Wrongs that the defendant knew (or should have known) would be caused by their actions.
Occur when the defendant’s actions or inactions were unreasonably unsafe.
Intentionally putting another person in reasonable apprehension of an imminent harmful or offensive contact.
Intentional causation of harmful or offensive contact with another person without that person’s consent.
An act of restraining another person and causing that person to be confined in a bounded area.
The right of an individual to have personal, identifiable medical information, referred to as protected health information, kept private.
Individually identifiable health information, including demographic data, that relates to the individual’s past, present, or future physical or mental health or condition; the provision of health care to the individual; and the past, present, or future payment for the provision of health care to the individual.
Federal regulations to ensure the privacy and protection of personal records and information.
Individuals required by state law to report suspected neglect or abuse of children, adults at risk, and the elderly.
Adults who have a physical or mental condition that impairs their ability to care for their own needs.
When an individual makes negative, malicious, and false remarks about another person to damage their reputation.
An intentional tort that occurs when an individual is deceived for personal gain.
The failure to exercise the ordinary care a reasonable person would use in similar circumstances.
A specific term used for negligence committed by a health professional with a license.

