The Assessment Standard of Practice established by the American Nurses Association (ANA) states, “The registered nurse collects pertinent data to the health care and information relative to the health care consumer’s health or the situation.”[1] Review the competencies for the Assessment Standard of Practice for registered nurses in the following box.
ANA’s Assessment Competencies[2]
The registered nurse:
- Creates the safest environment possible for conducting assessments.
- Collects pertinent data related to health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, the inherent dignity, worth, and unique attributes of every person, including, but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.
- Utilizes a health and wellness model of assessment that incorporates integrative approaches to data collection and honors the whole person.
- Recognizes the health care consumer or designated person as the decision-maker regarding their own health.
- Explores the health care consumer’s culture, values, preferences, expressed and unexpressed needs, and knowledge of the heath care situation.
- Assesses the impact of family dynamics on the health care consumer’s health and wellness.
- Identifies enhancements and barriers to effective communication based on personal, cognitive, physiological, psychosocial, literacy, financial, and cultural considerations.
- Engages the health care consumer, family, significant others, and interprofessional team members in holistic, culturally sensitive data collection.
- Integrates knowledge from current local, regional, national, and global health initiatives and environmental factors into the assessment process.
- State and local departments of health
- World Health Organization
- World Health Organization health topics
- Healthy People
- Centers for Disease Control and Prevention
- Prioritizes data collection based on the health care consumer’s immediate condition, the anticipated needs of the health care consumer or situation, or both.
- Uses evidence-based assessment techniques and available data and information to identify patterns and variances in the consumer’s health.
- Remains knowledgeable about constantly changing technologies that impact the assessment process (e.g., telehealth, artificial intelligence).
- Analyzes assessment data to identify patterns, trends, and situations that impact the person’s health and wellness.
- Validates the analysis with the health care consumer.
- Documents data accurately and makes accessible to the interprofessional team in a timely manner.
- Communicates changes in a person’s condition to the interprofessional team.
- Applies the provisions of the ANA Code of Ethics, legal guidelines, and policies to the collection, maintenance, use, and dissemination of data and information.
- Recognizes the impact of one’s own personal attitudes, values, beliefs, and biases on the assessment process.
Review the components of a nursing assessment in the “Nursing Process” chapter of Open RN Nursing Fundamentals.
Nursing assessments related to mental health disorders differ from physiological assessments with a greater focus on collecting subjective data. For example, prior to administering a cardiac medication to a client with a heart condition, a nurse will assess objective data such as blood pressure and an apical heart rate to determine the effectiveness of the medication treatment. However, prior to administering an antidepressant, a nurse uses therapeutic communication to ask questions and gather subjective data about how the patient is feeling to determine the effectiveness of the medication. The nurse will also observe client behaviors, speech, mood, and thought processes as part of the assessment.
As a nurse, you cannot directly measure a neurotransmitter to determine the effects of the medication, but you can ask questions to determine how your patient is feeling emotionally and perceiving the world, which are influenced by neurotransmitter levels. An example of a nurse using therapeutic communication to perform subjective assessment is, “Tell me more about how you are feeling today.” The nurse may also use general survey techniques such as simply observing the patient to assess for cues of behavior. Examples of objective data collected by a general survey could be assessing the patient’s mood, hygiene, appearance, or movement.
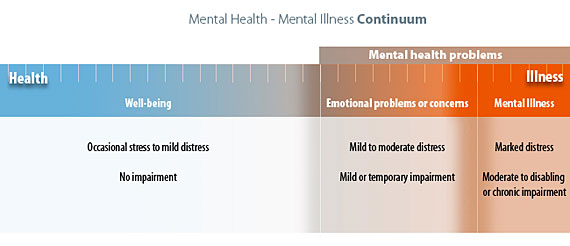
Recall the mental health continuum introduced in the “Foundational Mental Health Concepts” chapter (see Figure 4.2[3]). Nurses in any setting holistically assess their clients’ physical, emotional, and mental health, as well as any impairments impacting their functioning. They must recognize subtle cues of undiagnosed or poorly managed physical and mental disorders and follow up appropriately with other members of the interprofessional health care team.
When assessing a client’s mental health, the nurse incorporates a variety of assessments, in addition to the traditional physical examination. Assessments may include the following:
- Performing a mental status examination
- Completing a psychosocial assessment
- Reviewing the client’s use of psychotropic medications (drugs that treat psychiatric symptoms) and/or other medications that can cause psychiatric symptoms as side effects
- Screening for suicidal ideation, exposure to trauma or violence, and substance misuse
- Incorporating a spiritual assessment while assessing the client’s coping status
- Incorporating life span, developmental, and cultural considerations
- Reviewing specific laboratory results related to the client’s use of psychotropic and other medications
Mental Status Examination
Registered nurses must use effective clinical interviewing skills while performing a mental status assessment and developing a therapeutic nurse-client relationship.[4] Read more about establishing a therapeutic nurse-client relationship in the “Therapeutic Communication and the Nurse-Client Relationship” chapter. Assessing a client with a suspected or previously diagnosed mental health disorder focuses on both verbal and nonverbal assessments. New assessment findings are compared to the baseline admission findings to determine if the client’s condition is improving, worsening, or remaining the same.
When conducting a focused assessment on a client’s mental health, the mental status examination is a priority component of the overall assessment. A successful nurse develops a style in which the bulk of the mental status examination is performed through unstructured observations made during the routine physical examination, also referred to as the “general survey.” When the nurse recognizes cues of possible mental health disorders, such as aberrant behavior or difficulties in day-to-day functioning, then a focused mental status examination should be completed.
A mental status examination assesses a client’s level of consciousness and orientation, appearance and general behavior, speech, motor activity, affect and mood, thought and perception, attitude and insight, and cognitive abilities. The examiner should also monitor their personal reaction to a client when performing a mental status examination. The structured components of a mental status examination are outlined in Table 4.3 and further described in the following subsections.
Read about the components of a general survey in the “General Survey” chapter of Open RN Nursing Skills.
Table 4.3 Mental Status Examination[5]
| Assessment | Expected Findings/Optimal Level of Functioning | Unexpected Findings/Impaired Functioning |
|---|---|---|
| Signs of Distress |
|
|
| Level of Consciousness and Orientation |
|
|
| Appearance and General Behavior |
|
|
| Speech |
|
|
| Motor Activity |
|
|
| Affect and Mood |
|
|
| Thought and Perception |
|
|
| Attitude and Insight |
|
|
| Cognitive Abilities |
|
|
| Examiner’s Reaction to Client |
|
|
Signs of Distress
If a client is exhibiting signs of distress during an examination, the nurse must quickly obtain focused assessment data and obtain additional assistance based on the level of emergency care required and agency policy. For example, if a client is found unresponsive, a “code” is typically called during inpatient care, or 911 is called in an outpatient setting as the nurse begins cardiopulmonary resuscitation (CPR). If a client is demonstrating difficulty breathing, new onset confusion, or other signs of a deteriorating condition, the rapid response team may be called, or other emergency assistance may be obtained per agency policy. Keep in mind that the emergency administration of naloxone may be required in cases of a suspected opioid overdose.
Level of Consciousness and Orientation
A normal level of consciousness is when the client is alert (i.e., the ability to respond to stimuli at the same level as most people) and oriented to person, place, and time. Clouded consciousness refers to a state of reduced awareness to stimuli. Delirium is an acute onset of an abnormal mental state, often with fluctuating levels of consciousness, disorientation, irritability, and hallucinations. Delirium is often associated with infection, metabolic disorders, or toxins in the central nervous system. Obtundation refers to a moderate reduction in the client’s level of awareness so that mild to moderate stimuli do not awaken the client. When arousal does occur, the patient is slow to respond. Stupor refers to unresponsiveness unless a vigorous stimulus is applied, such as a sternal rub. The client quickly drifts back into a deep sleep-like state on cessation of the stimulation. Coma refers to unarousable unresponsiveness, where vigorous noxious stimuli may not elicit reflex motor responses. For example, a client in a coma may not pull their foot away from a painful prick of their toe with a needle. When documenting reduced levels of consciousness, note the type of stimulus required to arouse the patient and the degree to which the patient can respond when aroused.[6]
Appearance and General Behavior
This component refers to an overall impression of the client, including their physical appearance regarding their age, grooming, dressing, posture, eye contact, ability to socialize with others, and general behaviors. There are several terms used to describe a client’s appearance and behavior. For example, the appearance of one’s age can be altered due to chronic illness and pain. Providers may document that a client “appears their stated age” or “appears older than their stated age.” Clients may be described as well-groomed (i.e., exhibit good hygiene) or disheveled (i.e., their hair, clothes, or hygiene appears untidy, disordered, unkempt, or messy). Their dress may be described as “appropriate” or “inappropriate” according to the weather and situation. A client’s posture may be described as “erect” or “slumped.” Clients may be described as having “good eye contact” (i.e., they maintain a direct gaze into the examiner’s eyes) or “poor eye contact” (i.e., they avoid direct eye contact).[7] Life span and cultural considerations must always be kept in mind when assessing a client’s appearance and general behavior. For example, some cultures consider direct eye contact disrespectful.
Speech
Evaluating speech as the client answers open-ended questions provides useful information. A client demonstrates normal speech when responding to verbal questions appropriately with an even rate, rhythm, and tone. Their speech is clear and understandable, and the client follows instructions appropriately.
Characteristics of speech can be described as normal, rapid, slow (i.e., delayed rhythm of conversation), loud, or soft. Stuttering and aphasia may occur. Examples of speech difficulties include lack of appropriate responses to verbal questions, rapid and/or pressured speech of a client experiencing mania or amphetamine intoxication, or halting speech of a client experiencing word-finding difficulties due to a previous stroke.[8]
Other terms used to describe speech include circumstantial (i.e., speaking with many unnecessary or tedious details without getting to the point of the conversation) and poverty of content (i.e., a conversation in which the client talks without stating anything related to the question, or their speech in general is vague and meaningless).
Motor Activity
Overall motor activity should be noted, including any tics or unusual mannerisms. Normal motor activity refers to the client having good balance, moving all extremities equally bilaterally, and walking with a smooth gait. Slow movements or lack of spontaneity in movement can occur due to depression or dementia. Dyskinesia (uncontrolled, involuntary movement) and akathisia (i.e., motor restlessness) may occur if the client is experiencing extrapyramidal syndrome related to psychotropic medication use.[9]
Terminology used to describe motor activity includes psychomotor agitation (i.e., a condition of purposeless, non goal-directed activity) and psychomotor retardation (i.e., a condition of extremely slow physical movements, slumped posture, or slow speech patterns).
Affect and Mood
Affect refers to the client’s expression of emotion, and mood refers to the predominant emotion expressed by an individual.[10] Sustained emotions influence a person’s behavior, personality, and perceptions. Mood can be described using various terms such as neutral, elevated, or labile (i.e., a rapid change in emotional responses, mood, or affect that are inappropriate for the moment or the situation). It can also be described as anxious, angry, sad, irritable, dysphoric (i.e., exhibiting depression), or euphoric (i.e., a pathologically elevated sense of well-being). People may express feelings of emptiness, impaired self-esteem, indecisiveness, or crying spells. [11]
Normal affect and mood are described as euthymic (i.e., displays a wide range of emotion that is appropriate for the situation). Abnormal findings related to affect include inappropriateness for the situation (e.g., laughing at the recent death of a loved one) or incongruent. Congruence refers to the consistency of verbal and nonverbal communication. Affect may also be described as subdued, tearful, labile, blunted (i.e., diminished range and intensity), or flat (no emotional expression).
Other terminology related to documenting a client’s mood includes alexithymia (i.e., the inability to describe emotions with how one is feeling), anhedonia (i.e, the lack of experiencing pleasure in activities normally found enjoyable), and apathy (i.e., a lack of feelings, emotions, interests, or concerns).
Thoughts and Perceptions
The manner in which a client perceives and responds to stimuli is a critical psychiatric assessment. The inability to process information accurately is a component of the definition of psychotic thinking. For example, does the client harbor realistic concerns or are their concerns elevated to the level of irrational fear? Is the client responding in an exaggerated fashion to actual events? Is there no discernible basis in reality for the patient’s beliefs or behavior?[12]
Clients with mental health disorders may experience intrusive thoughts, delusions, and/or obsessions. Delusions are a fixed, false belief not held by cultural peers and persisting in the face of objective contradictory evidence. For example, a client may have the delusion that the CIA is listening to their conversations via satellites. Grandiose delusions refer to a state of false attribution to the self of great ability, knowledge, importance or worth, identity, prestige, power, or accomplishment.[13] Clients may withdraw into an inner fantasy world that’s not equivalent to reality, where they have inflated importance, powers, or a specialness that is opposite of what their actual life is like.[14]Paranoia is a condition characterized by delusions of persecution.[15] Clients often experience extreme suspiciousness or mistrust or express fear. For example, a resident of a long-term care facility may have delusions that the staff is trying to poison them.
Obsessions are persistent thoughts, ideas, images, or impulses that are experienced as intrusive or inappropriate and result in anxiety, distress, or discomfort. Common obsessions include repeated thoughts about contamination, a need to have things in a particular order or sequence, repeated doubts, aggressive impulses, and sexual imagery. Obsessions are distinguished from excessive worries about everyday occurrences because they are not concerned with real-life problems.[16] Rumination is obsessional thinking involving excessive, repetitive thoughts that interfere with other forms of mental activity.[17]
Clients may also experience altered perceptions such as hallucinations and illusions. Hallucinations are false sensory perceptions not associated with real external stimuli and can include any of the five senses (auditory, visual, gustatory, olfactory, and tactile). For example, a client may see spiders climbing on the wall or hear voices telling them to do things. These are referred to as “visual hallucinations” or “auditory hallucinations.”
Illusions are misperceptions of real stimuli. For example, a client may misperceive tree branches blowing in the wind at night to be the arms of monsters trying to grab them.
It is important for nurses to remember that delusions, hallucinations, and illusions feel very real to clients and cause internal emotional reactions, even when a caregiver reassures them they are not based in reality. Because clients often conceal these experiences, it is helpful to ask leading questions, such as, “Have you ever seen or heard things that other people could not see or hear? Have you ever seen or heard things that later turned out not to be there?”[18]
Other terms used to document clients’ thought processes include racing thoughts, flight of ideas, loose associations, and clang associations. Racing thoughts are fast moving and often repetitive thought patterns that can be overwhelming. They may focus on a single topic, or they may represent multiple different lines of thought. For example, a client may have racing thoughts about a financial issue or an embarrassing moment.
Flight of ideas indicates the client frequently shifts from one topic to another with rapid speech, making it seem fragmented. The examiner may feel the client is rambling and changing topics faster than they can keep track, and they probably can’t get a word in edgewise.[19] An example of client exhibiting a flight of ideas is, “My father sent me here. He drove me in a car. The car is yellow in color. Yellow color looks good on me.”[20]
Loose associations refers to jumping from one idea to an unrelated idea in the same sentence. For example, the client might state, “I like to dance, and my feet are wet.”[21] The term word salad refers to severely disorganized and virtually incomprehensible speech or writing, marked by severe loosening of associations.[22]
Clang associations refers to stringing words together that rhyme without logical association and do not convey rational meaning. For example, a client exhibiting clang associations may state, “Here she comes with a cat catch a rat match.”
Clients with altered perceptions, especially when experiencing hallucinations and delusions, may have violent thoughts regarding themselves or others. If a client is having auditory hallucinations, it is vital for the nurse to determine if the voices are encouraging the client to hurt themselves or others. Homicidal ideation refers to threats or acts of life-threatening harm toward another person. Suicidal ideation is used to describe an individual who has been thinking about suicide but does not necessarily have an intention to act on that idea. Suicide attempt is a term used to describe an individual who harms themselves with intent to end their life but does not die as a result of their actions. Suicide plan refers to an individual who has a plan for suicide, has the means to injure oneself, and has the intent to die.
Of all portions of the mental status examination, the evaluation of thought disorders is the most difficult and requires a thorough assessment.[23] Psychiatric-mental health nurse specialists receive additional training in assessing thought disorders. These types of thought disorders are associated with mental illnesses like bipolar disorder and schizophrenia and may precede an episode of psychosis, so it is important to obtain further assistance if you notice a client is newly exhibiting these types of behaviors.[24]
Attitude and Insight
The client’s attitude is the emotional tone displayed toward the examiner, other individuals, or their illness. It may convey a sense of hostility, anger, helplessness, pessimism, overdramatization, self-centeredness, or passivity. It is important to determine the client’s attitude toward emotional problems or diagnosed mental health disorders. Does the client look forward to improvement and recovery or are they resigned to suffer?[25]
Insight is the client’s ability to identify the existence of a problem and to have an understanding of its nature.
Nurses must also be aware of transference. Transference occurs when the client projects (i.e., transfers) their feelings onto the nurse. For example, a client is feeling angry at a family member related to a previous disagreement and displaces the anger onto the nurse during the interview.
Cognitive Abilities
Cognition is the mental action or process of acquiring knowledge and understanding through thought, experience, and the senses. It includes thinking, knowing, remembering, judging, and problem-solving. When performing focused assessments on cognition, the examiner assesses attention and memory.[26] A term related to assessing attention is distractibility, referring to the client’s attention being easily drawn to unimportant or irrelevant external stimuli.
Memory disturbance is a common complaint and is often a presenting symptom in the elderly. Memory can be grouped into three categories: immediate recall, short-term memory, and long-term storage. Short-term memory is the most clinically pertinent, and the most important to be tested. Short-term retention requires that the patient process and store information so that they can move on to a second intellectual task and then call up the remembrance after completion of the second task. For example, short-term memory may be tested by having the patient repeat the names of four unrelated objects and then asking the patient to recall the information in 3 to 5 minutes after performing a second, unrelated mental task.[27]
Examiner’s Reaction to the Client
Assessing a client sometimes results in the nurse developing subtle and easily overlooked feelings toward the client. For example, it can be difficult to repeatedly address a client’s negative state. Examiners may experience feelings of frustration, which can be taken by patients to mean there’s something wrong with them. In such cases, nurses should examine their reactions to the client and be alert to feelings of distraction, boredom, or frustration. They should also be aware that clients perceive a nurse’s feelings through their nonverbal communication, such as facial expressions, posture, tone of voice, and lack of eye contact.[28]
Nurses should also be aware of countertransference. Countertransference refers to a tendency for the examiner to displace (transfer) their own feelings onto the client and then these feelings may influence the client. For example, a nurse finds themself providing advice about how to raise children to a client. Upon self-reflection, they realize it is a countertransference reaction related to their previous parenting experience.[29]
Review a brief mental status examination PDF form from TherapistAid.
Psychosocial Assessment
A psychosocial assessment (also referred to as a health history) is a component of the nursing assessment process that obtains additional subjective data to detect risks and identify treatment opportunities and resources. Agencies have specific forms used for psychosocial assessments/health histories that typically consist of several components[30],[31]:
- Cultural assessment
- Reason for seeking health care (i.e., “chief complaint”)
- Thoughts of self-harm or suicide
- Current and past medical history
- Current medications
- History of previously diagnosed mental health disorders
- Previous hospitalizations
- Educational background
- Occupational background
- Family dynamics
- History of exposure to psychological trauma, violence, and domestic abuse
- Substance use (tobacco, alcohol, recreational drugs, misused prescription drugs)
- Family history of mental illness
- Coping mechanisms
- Functional ability/Activities of daily living
- Spiritual assessment
Review specific questions used during a psychosocial assessment/health history in the “Health History” chapter in Open RN Nursing Skills.
Cultural Formulation Interview Questions
While performing a psychosocial assessment, it is important to begin by performing a cultural assessment. We all bring our own cultural beliefs, values, and expectations to the clinical encounter, which influences how we approach specific aspects of care. The American Psychiatric Association developed evidence-based Cultural Formulation Interview (CFI) questions as a way to incorporate cultural assessment into the care of all clients that enhances clinical understanding and decision-making.[32] The CFI questions are used to clarify key aspects of the presenting clinical problem from the point of view of the individual and other members of the individual’s social network (e.g., family, friends, or others involved in the current problem). This includes the problem’s meaning, potential sources of help, and expectations for health care services.
CFI questions used with all clients include the following[33]:
- What brings you here today?
- What troubles you most about this problem?
- Why do you think this is happening to you? What do you think is the cause of this problem?
- Are there any kinds of support that make this problem better, such as support from family, friends, or others?
- Are there any kinds of stresses that make this problem worse, such as difficulties with money or family problems?
- Sometimes aspects of people’s background or identity can make their problem better or worse, such as the communities they belong to, the languages they speak, where they or their family are from, their race or ethnic background, their gender or sexual orientation, or their faith or religion. Are there any aspects of your background or identity that make a difference to this problem?
- Sometimes people have various ways of dealing with problems. What have you done on your own to cope with this problem?
- Often, people look for help from many different sources, including different kinds of doctors, helpers, or healers. In the past, what kinds of treatment, help, advice, or healing have you sought for this problem?
- Has anything prevented you from getting the help you need?
- What kinds of help do you think would be most useful to you at this time for this problem?
- Are there other kinds of help that your family, friends, or other people have suggested that would be helpful for you now?
- Sometimes health care professionals and patients misunderstand each other because they come from different backgrounds or have different expectations. Have you been concerned about misaligned care expectations and is there anything that we can do to provide you with the care you need?
Findings from the cultural formulation interview are used to individualize a client’s plan of care to their preferences, values, beliefs, and goals.
Reason for Seeking Health Care
It is helpful to begin the psychosocial assessment by obtaining the reason why the patient is seeking health care in their own words. During a visit to a clinic or emergency department or on admission to a health care agency, the patient’s primary reasons for seeking care are referred to as the chief complaint. Assessing a client’s chief complaint recognizes that clients are complex beings, with potentially multiple coexisting health needs, but there is often a pressing issue that requires most immediate care. Questions used to evaluate a client’s chief complaint are as follows:
- What brought you in today?
- How long has this been going on?
- How is this affecting you?
After identifying the reason the patient is seeking health care, additional focused questions are used to obtain detailed information about priority concerns, such as pain or other symptoms causing discomfort. The mnemonic PQRSTU is used to ask the patient questions in an organized fashion. See Table 4.3b for examples of questions used to assess a client’s report of pain.
Table 4.3b Sample PQRSTU Questions
| PQRSTU | Sample Questions |
|---|---|
| Provocation/Palliation
|
What makes your pain worse?
What makes your pain feel better? |
| Quality | What does the pain feel like?
Note: You can provide suggestions for pain characteristics such as “aching,” “stabbing,” or “burning.” |
| Region | Where exactly do you feel the pain? Does it move around or radiate elsewhere? |
| Severity | How would you rate your pain on a scale of 0 to 10, with “0” being no pain and “10” being the worst pain you’ve ever experienced? |
| Timing/Treatment
|
When did the pain start?
What were you doing when the pain started? Is the pain constant or does it come and go? If the pain is intermittent, when does it occur? How long does the pain last? Have you taken anything to help relieve the pain? |
| Understanding | What do you think is causing the pain? |
Thoughts of Suicide
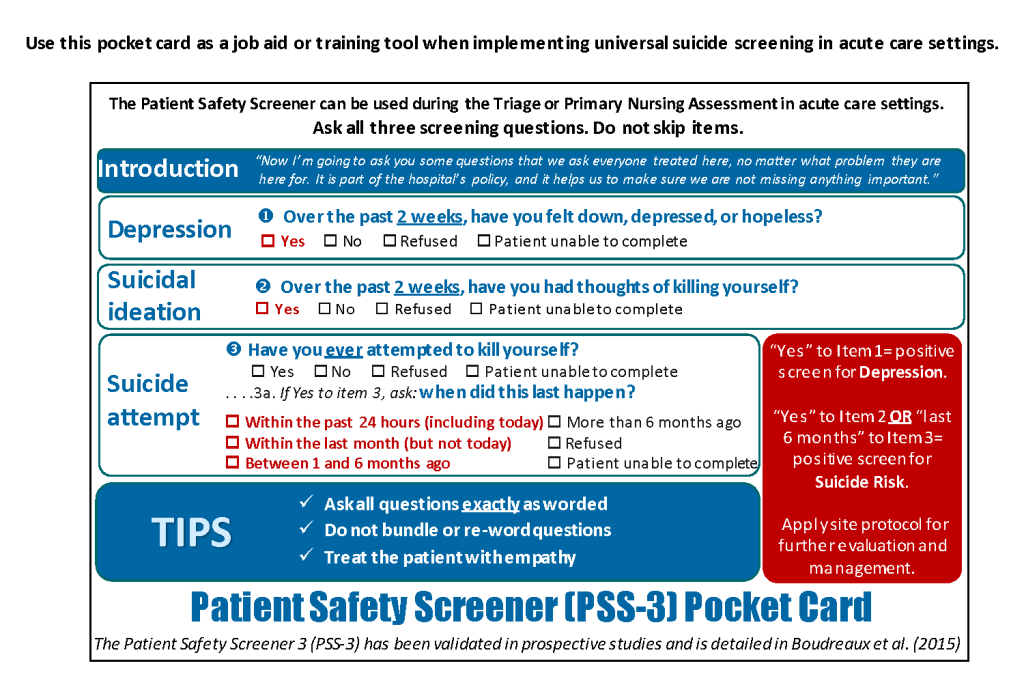
As discussed in Chapter 1, all clients aged 12 and older presenting for acute care should be screened for suicidal ideation. Clients being evaluated or treated for mental health conditions often have suicidal ideation, and up to 10 percent of emergency department clients presenting with medical issues have a hidden risk for suicide, such as recent suicidal ideation or previous suicide attempts.[34] Universal screening allows for the detection of suicide risk and implementation of early interventions before a person attempts suicide.
It is important to introduce suicide screening in a way that helps the patient understand its purpose and normalize questions that might otherwise seem intrusive. A nurse might introduce the topic in the following way: “Now I’m going to ask you some questions that we ask everyone treated here, no matter what problem they are here for. It is part of the hospital’s policy, and it helps us to make sure we are not missing anything important.”[35]
The Patient Safety Screener (PSS-3) is an example of a brief screening tool to detect suicide risk in all patients presenting to acute care settings.[36] See Figure 4.3[37] for an image of the PSS-3.
The PSS-3 consists of assessing for three items: depression, active suicidal ideation, and lifetime suicide attempt. Each of these items taps a different aspect of suicide risk[38]:
- Depression is a common precipitant of suicidal ideation and behavior and is the most common diagnosis among those who die by suicide.
- Suicidal ideation (i.e., thoughts about killing oneself) is a precondition for suicidal behavior.
- A previous suicide attempt is one of the most consistent risk factors for suicide.
Self-Injury
Non-suicidal self-injury (NSSI) refers to intentional self-inflicted destruction of body tissue without suicidal intention and for purposes not socially sanctioned. Common forms of NSSI include behaviors such as cutting, burning, scratching, and self-hitting. It is considered a maladaptive coping strategy without the desire to die. NSSI is a common finding among adolescents and young adults in psychiatric inpatient settings.[39]
Family Dynamics
Family dynamics are included in a psychosocial assessment, especially for children, adolescents, and older adults. Family dynamics refers to the patterns of interactions among relatives, their roles and relationships, and the various factors that shape their interactions. Because family members rely on each other for emotional, physical, and economic support, they are primary sources of relationship security or stress. Family dynamics and the quality of family relationships can have either a positive or negative impact on an individual’s health. For example, secure and supportive family relationships can provide love, advice, and care, whereas stressful family relationships can be burdened with arguments and constant critical feedback.[40]
Unhealthy family dynamics can cause children to experience trauma and stress as they grow up. This type of exposure, known as adverse childhood experiences (ACEs), is linked to an increased risk of developing physical and mental health problems such as heart, lung, and liver disease; depression; and anxiety. Unhealthy family dynamics also correlate with an increased risk of substance use and addiction among adolescents.[41]
Effectively assessing and addressing a client’s family dynamic and its role in health and disease require an interprofessional team of health professionals, including nurses, physicians, social workers, and therapists. Nurses are in a unique position to observe and document interaction patterns, assess family relationships, and tend to family concerns in the clinical setting because they are in frequent contact with family members.[42]
Spiritual Assessment
Spiritual assessment is included in a psychosocial assessment. It is common for people in the process of recovery from mental health disorders and substance use to search for spiritual support.[43] Spirituality includes a sense of connection to something larger than oneself and typically involves a search for meaning and purpose in life. Basic questions used to assess spirituality include the following:
- Who or what provides you with strength or hope?
- How do you express your spirituality?
- What spiritual needs can we advocate for you during this health care experience?
Over the past decade, research has demonstrated the importance of spirituality in health care.[44],[45] Spiritual distress is very common for clients experiencing serious illness, injury, or the dying process, and nurses are on the front lines as they assist these individuals to cope with these life events. Addressing a patient’s spirituality and advocating spiritual care have been shown to improve patients’ health and quality of life, including how they experience pain, cope with stress and suffering associated with serious illness, and approach end of life.[46],[47]
The FICA Spiritual History Tool© is a common tool used to gather information about a patient’s spiritual history and preferences.[48] FICA© is a mnemonic for Faith, Importance, Community, and Address in Care. Read more about the FICA© tool in the following box.
The FICA© Spiritual History Tool[49]
F – Faith and Belief: Determine if the patient identifies with a particular belief system or spirituality.
I – Importance: Ask, “Is this belief important to you? Does it influence how you think about health and illness? Does it influence your health care decisions?”
C – Community: Determine if the client belongs to a spiritual community (e.g., a church, temple, mosque, or other group). If not, ask, “Would it be helpful to you to find a spiritual community?”
A – Address in Care: Evaluate what should be addressed during the client’s care. Ask, “What should be included in your treatment plan? Are there spiritual practices you want to develop? Would you like to see a chaplain, spiritual director, or pastoral counselor while you are here?”
Based on the assessment findings, nurses may refer clients to agency chaplains or to the client’s religious leaders for spiritual support to enhance coping.
Read more about spiritual assessment and providing spiritual care in the “Spirituality” chapter of Open RN Nursing Fundamentals.
Screening Tools
Screening tools are evidence-based methods to assess specific information related to mental health disorders. These tools may be used on admission to the hospital or treatment facility, as well as at different times throughout the client’s stay. Findings may be used to compare client progress during the hospital stay or from a previous admission. The registered nurse often conducts these screening tools as part of the interprofessional health care treatment team. Read more about specific screening tools in each “disorder” chapter.
Laboratory and Diagnostic Testing
Nurses review laboratory and diagnostic testing results as part of the assessment process.
Nurses monitor electrolytes and medication levels as they evaluate the need for medication adjustment. For example, serum sodium levels may be out of range due to conditions such as polydipsia, and poor nutritional or hydration status related to mental health disorders may require additional interventions by the nurse. Specific laboratory and diagnostic tests will be discussed in each “disorder” chapter, as well as in the “Psychotropic Medications” chapter.
Life Span Considerations
Life span considerations influence nursing assessments, care planning, and interventions. Mental health disorders occur across the life span, from the very young to the very old, and developmental stages must be considered when identifying impairments. Assessments and interventions must be individualized to the age and developmental level of the client. Development encompasses physical, social, and cognitive changes that occur continuously throughout one’s life. See Figure 4.4[50] for an image of the human life cycle.

There are multiple factors that affect human development with expected milestones along the way. Cognitive development encompasses several different skills that develop at different rates. Each human has their own individual experience that influences development of intelligence and reasoning as they interact with one another. With these unique experiences, everyone has a memory of feelings and events that is exclusive to them.[51]
There are many theories regarding how infants and children grow and develop into happy, healthy adults. Three major theories that have historically impacted nursing care are Freud’s Psychosexual Theory of Development, Erikson’s Psychosocial Stages of Development, and Piaget’s Cognitive Theory of Development.
Freud’s Psychosexual Theory of Development
Sigmund Freud (1856–1939) believed that personality develops during early childhood, and childhood experiences shape our personalities and behavior as adults. Freud believed that each individual must pass through a series of stages during childhood, and if we lack proper nurturance and parenting during a stage, we may become stuck, or fixated, in that stage. According to Freud, children’s pleasure-seeking urges are focused on different areas of the body, called erogenous zones, at each of the five stages of development: oral, anal, phallic, latency, and genital.[52]
While most of Freud’s ideas are not supported by research and modern psychologists dispute Freud’s psychosexual stages as a legitimate explanation for how one’s personality develops, Freud’s original theory supported that one’s personality is shaped, in some part, by childhood experiences.[53]
Erikson’s Psychosocial Stages of Development
Erik Erikson (1902–1994) took Freud’s theory and modified it as psychosocial theory. Erikson’s psychosocial development theory emphasizes the social nature of our development rather than its sexual nature. It describes eight sequential stages of individual human development influenced by biological, psychological, and social factors throughout the life span that contribute to an individual’s personality. Erikson’s stages of development are trust versus mistrust, autonomy versus shame, initiative versus guilt, industry versus inferiority, identity versus identity confusion, intimacy versus isolation, generativity versus stagnation, and integrity versus despair.[54],[55]
- Trust vs. Mistrust
The first stage that develops is trust (or mistrust) that basic needs, such as nourishment and affection, will be met. Trust is the basis of our development during infancy (birth to 12 months). Infants are dependent upon their caregivers for their needs. Caregivers who are responsive and sensitive to their infant’s needs help their baby to develop a sense of trust, and the infant will perceive the world as a safe, predictable place. Unresponsive caregivers who do not meet their baby’s needs can engender feelings of anxiety, fear, and mistrust, and the infant will perceive the world as unpredictable.[56]
- Autonomy vs. Shame
Toddlers begin to explore their world and learn that they can control their actions and act on the environment to get results. They begin to show clear preferences for certain elements of the environment, such as food, toys, and clothing. A toddler’s main task is to resolve the issue of autonomy versus shame and doubt by working to establish independence. For example, we might observe a budding sense of autonomy in a two-year-old child who wishes to choose their own clothes and dress themselves. Although the outfits might not be appropriate for the situation, the input in basic decisions has an effect on the toddler’s sense of independence. If denied the opportunity to act on their environment, they may begin to doubt their abilities, which could lead to low self-esteem and feelings of shame.[57]
- Initiative vs. Guilt
After children reach the preschool stage (ages 3–6 years), they are capable of initiating activities and asserting control over their world through social interactions and play. By learning to plan and achieve goals while interacting with others, preschool children can master a feeling of initiative and develop self-confidence and a sense of purpose. Those who are unsuccessful at this stage may develop feelings of guilt.[58]
- Industry vs. Inferiority
During the elementary school stage (ages 7–11), children begin to compare themselves to their peers to see how they measure up. They either develop a sense of pride and accomplishment in their schoolwork, sports, social activities, and family life, or they may feel inferior and inadequate if they feel they don’t measure up to their peers.[59]
- Identity vs. Identity Confusion
In adolescence (ages 12–18), children develop a sense of self. Adolescents struggle with questions such as, “Who am I?” and “What do I want to do with my life?” Along the way, adolescents try on many different selves to see which ones fit. Adolescents who are successful at this stage have a strong sense of identity and are able to remain true to their beliefs and values in the face of problems and other people’s perspectives. Teens who do not make a conscious search for identity, or those who are pressured to conform to their parents’ ideas for the future, may have a weak sense of self and experience role confusion as they are unsure of their identity and confused about the future.[60]
- Intimacy vs. Isolation
People in early adulthood (i.e., 20s through early 40s) are ready to share their lives and become intimate with others after they have developed a sense of self. Adults who do not develop a positive self-concept in adolescence may experience feelings of loneliness and emotional isolation.[61]
- Generativity vs. Stagnation
When people reach their 40s, they enter a time period known as middle adulthood that extends to the mid-60s. The developmental task of middle adulthood is generativity versus stagnation. Generativity involves finding your life’s work and contributing to the development of others through activities such as volunteering, mentoring, and raising children. Adults who do not master this developmental task may experience stagnation with little connection to others and little interest in productivity and self-improvement.[62]
- Integrity vs. Despair
The mid-60s to the end of life is a period of development known as late adulthood. People in late adulthood reflect on their lives and feel either a sense of satisfaction or a sense of failure. People who feel proud of their accomplishments feel a sense of integrity and often look back on their lives with few regrets. However, people who are not successful at this stage may feel as if their life has been wasted. They focus on what “would have,” “should have,” or “could have” been. They face the end of their lives with feelings of bitterness, depression, and despair.[63]
Piaget’s Cognitive Theory of Development
Jean Piaget (1896–1980) studied childhood development by focusing on children’s cognitive growth. He believed that thinking is a central aspect of development and that children are naturally inquisitive but do not think and reason like adults. Children explore the world as they attempt to make sense of their experiences. His theory explains that humans move from one stage to another as they seek cognitive equilibrium and mental balance. There are four stages in Piaget’s theory of development that occur in children from all cultures[64],[65]:
- Sensorimotor period. The first stage extends from birth to approximately two years and is a period of rapid cognitive growth. During this period, infants develop an understanding of the world by coordinating sensory experiences (seeing, hearing) with motor actions (reaching, touching). The main development during the sensorimotor stage is the understanding that objects exist, and events occur in the world independently of one’s own actions. Infants develop an understanding of what they want and what they must do to have their needs met. They begin to understand language used by those around them to make needs met.
- Preoperational period. The second stage begins in the toddler years. This continues through early school-age years. This is the time frame when children learn to think in images and symbols. Play is an important part of cognitive development during this period.
- Concrete Operations period. Older school-age children (age 7 years to 11 years) learn to think in terms of processes and can understand that there is more than one perspective when discussing a concept. This stage is considered a major turning point in the child’s cognitive development because it marks the beginning of logical or operational thought.
- Formal Operations period. Children enter this stage around age 12 as they become self-conscious and egocentric. Adolescents gain the ability to think in an abstract manner by manipulating ideas in their head. Moving toward adulthood, this further develops into the ability to critically reason.
Cognitive Impairment
Cognitive impairment is a term used to describe impairment in mental processes that drive how an individual understands and acts in the world, affecting the acquisition of information and knowledge. Cognitive impairments can range from mild impairments, such as impairments in cognitive operations, to profound intellectual impairments causing minimal independent functioning. Components of cognitive functioning include attention, decision-making, general knowledge, judgment, language, memory, perception, planning, and reasoning.[66]
Review information about cognitive impairments associated with dementia and Alzheimer’s disease in the “Cognitive Impairments” chapter of Open RN Nursing Fundamentals.
Intellectual disability (formerly referred to as mental retardation) is a diagnostic term that describes intellectual and adaptive functioning deficits identified during the developmental period. In the United States, the developmental period refers to the span of time prior to the age of 18 years. Children with intellectual disabilities may demonstrate a delay in developmental milestones (e.g., sitting, speaking, walking) or demonstrate mild cognitive impairments that may not be identified until school-age. Intellectual disability is typically nonprogressive and lifelong. It is diagnosed by multidisciplinary clinical assessments and standardized testing and is treated with a multidisciplinary treatment plan that maximizes quality of life.[67]
Resilience
When assessing an individual’s developmental level, it is important to consider possible effects of adverse childhood events (ACEs) on their development. Science tells us that some children develop resilience, the ability to overcome serious hardship or traumatic experiences, while others do not. One way to understand the development of resilience is to visualize a seesaw. Protective experiences and coping skills on one side counterbalance significant adversity on the other. Resilience is evident when a child’s health and development tip toward positive outcomes – even when a heavy load of factors is stacked on the negative outcome side.[68]
The most common factor for children who develop resilience is at least one stable and committed relationship with a supportive parent, caregiver, or other adult. These relationships provide the personalized responsiveness and protection that buffer children from developmental disruption. They also build their ability to plan, monitor, and regulate behavior that enables children to respond adaptively to adversity and thrive. This combination of supportive relationships, adaptive skill-building, and positive experiences is the foundation of resilience.[69]
The capabilities that underlie resilience can be strengthened at any age. It is never too late to build resilience. Age-appropriate, health-promoting activities can significantly improve the chances that an individual will recover from stress-inducing experiences. For example, regular physical exercise, stress management activities, and programs that actively promote self-regulation skills can improve the abilities of children and adults to cope with adversity in their lives.[70]
Read more about promoting resilience across the life span at Harvard’s Center on the Developing Child Resilience webpage.
Cultural Considerations
Cultures and communities exhibit and explain symptoms of mental illness and manifest stress in various ways. Nurses should be aware of relevant contextual information stemming from a patient’s culture, race, ethnicity, religion, or geographical origin. For example, uncontrollable crying and headaches are symptoms of panic attacks in some cultures, whereas difficulty breathing may be the primary symptom in another culture. Understanding such distinctions will help nurses effectively treat them.[71]
At the center of patient-centered care is practicing with cultural humility and inclusiveness. In the 2021 edition of Nursing: Scope and Standards of Practice, the American Nurses Association (ANA) established a Standard of Professional Performance called Respectful and Equitable Practice. This standard is defined as, “The registered nurse practices with cultural humility and inclusiveness.” Cultural humility is “a humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot know everything about other cultures, and approach learning about other cultures as a life-long goal and process.”[72] Inclusiveness is defined as “the practice of providing equal access to opportunities and resources for people who might otherwise be excluded or marginalized, such as those having physical or mental disabilities or belonging to other minority groups.”[73] Read the ANA competencies for the Respectful and Equitable Practice standard in the following box.
ANA’s Respectful and Equitable Practice Competencies[74]
The registered nurse:
- Demonstrates respect, equity, and empathy in actions and interactions with all health care consumers.
- Respects consumer decisions without bias.
- Participates in life-long learning to understand cultural preferences, worldviews, choices, and decision-making processes of diverse consumers.
- Reflects upon personal and cultural values, beliefs, biases, and heritage.
- Applies knowledge of differences in health beliefs, practices, and communication patterns without assigning values to the differences.
- Addresses the effects and impact of discrimination and oppression on practice within and among diverse groups.
- Uses appropriate skills and tools for the culture, literacy, and language of the individuals and population served.
- Communicates with appropriate language and behaviors, including the use of qualified health care interpreters and translators in accordance with consumer needs and preferences.
- Serves as a role model and educator for the cultural humility and the recognition and appreciation of diversity and inclusivity.
- Identifies the cultural-specific meaning of interactions, terms, and content.
- Advocates for policies that promote health and prevent harm among diverse health care consumers and groups.
- Promotes equity in all aspects of health and heatlh care.
- Advances organizational policies, programs, services, and practices that reflect respect, equity, and values for diversity and inclusion.
Read more about cultural humility and advocating for the values, beliefs, and preferences of diverse clients in the “Diverse Clients” chapter of Open RN Nursing Fundamentals.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “continuum.jpg” by University of Michigan is used with permission. Access the original at https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse. ↵
- American Nurses Association, American Psychiatric Nurses Association, and International Society of Psychiatric-Mental Health Nurses. (2014). Psychiatric-Mental Health Nursing: Scope and Standards of Practice (2nd ed.). Nursebooks.org ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- American Psychological Association. (n.d.). APA Dictionary of Psychology. https://dictionary.apa.org/ ↵
- Raypole, C. (2019, November 20). 10 signs of covert narcissism. Healthline. https://www.healthline.com/health/covert-narcissist#fantasies ↵
- American Psychological Association. (n.d.). APA Dictionary of Psychology. https://dictionary.apa.org/ ↵
- American Psychological Association. (n.d.). APA Dictionary of Psychology. https://dictionary.apa.org/ ↵
- American Psychological Association. (n.d.). APA Dictionary of Psychology. https://dictionary.apa.org/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- PsychologGenie. (n.d.). The true meaning of flight of ideas explained with examples. https://psychologenie.com/flight-of-ideas-meaning-examples ↵
- American Psychological Association. (n.d.). APA Dictionary of Psychology. https://dictionary.apa.org/ ↵
- American Psychological Association. (n.d.). APA Dictionary of Psychology. https://dictionary.apa.org/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Joy, R. (2020, January 20). Clang association: When a mental health condition disrupts speech. Healthline. https://www.healthline.com/health/clang-association#whats-it-sound-like ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- Martin, D. C. (1990). The mental status examination. In Walker, H. K., Hall, W. D., Hurst, J. W., (Eds.), Clinical methods: The history, physical, and laboratory examinations. (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK320/ ↵
- DeAngelis, T. (2019). Better relationships with patients lead to better outcomes. Monitor on Psychology, 50(10), 38. https://www.apa.org/monitor/2019/11/ce-corner-relationships ↵
- DeAngelis, T. (2019). Better relationships with patients lead to better outcomes. Monitor on Psychology, 50(10), 38. https://www.apa.org/monitor/2019/11/ce-corner-relationships ↵
- GW School of Medicine & Health Sciences. (n.d.). Clinical FICA tool. https://smhs.gwu.edu/spirituality-health/program/transforming-practice-health-settings/clinical-fica-tool ↵
- Glasner, J., Baltag, V., & Ambresin, A. E. (2021). Previsit multidomain psychosocial screening tools for adolescents and young adults: A system review. Journal of Adolescent Health, 68, 449-459. https://www.jahonline.org/article/S1054-139X(20)30600-5/pdf ↵
- DeSilva, R., Aggarwall, N. K., & Lewis-Fernandez, R. (2015). The DSM-5 cultural formulation interview and the evolution of cultural assessment in psychiatry. Psychiatric Times, 32(6). https://www.psychiatrictimes.com/view/dsm-5-cultural-formulation-interview-and-evolution-cultural-assessment-psychiatry ↵
- American Psychiatric Association. (2013). Cultural formulation. In Diagnostic and Statistical Manual of Mental Disorders (5th ed.). American Psychiatric Association. pp. 749-759. ↵
- Suicide Prevention Resource Center. (n.d.). The patient safety screener: A brief tool to detect suicide risk. https://sprc.org/micro-learning/patientsafetyscreener ↵
- Suicide Prevention Resource Center. (n.d.). The patient safety screener: A brief tool to detect suicide risk. https://sprc.org/micro-learning/patientsafetyscreener ↵
- Suicide Prevention Resource Center. (n.d.). The patient safety screener: A brief tool to detect suicide risk. https://sprc.org/micro-learning/patientsafetyscreener ↵
- “Patient Safety Screener (PSS-3) Pocket Card” by University of Massachusetts Medical School (UMass Medical) is used on the basis of Fair Use. ↵
- Suicide Prevention Resource Center. (n.d.). The patient safety screener: A brief tool to detect suicide risk. https://sprc.org/micro-learning/patientsafetyscreener ↵
- Cipriano, A., Cella, S., & Cotrufo, P. (2017). Nonsuicidal self-injury: A systematic review. Frontiers in Psychology, 8. https://www.frontiersin.org/articles/10.3389/fpsyg.2017.01946/full ↵
- This work is a derivative of StatPearls by Jabbari & Rouster and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Jabbari & Rouster and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Jabbari & Rouster and is licensed under CC BY 4.0 ↵
- Neto, G. L., Rodrigues, L., Rozendo da Silva, D. A., Turato, E. R., & Campos, C. J. G. (2018). Spirituality review on mental health and psychiatric nursing. Revista Brasileira de Enfermagem, 71 (Suppl 5), 2323-2333. https://doi.org/10.1590/0034-7167-2016-0429 ↵
- Pilger, C., Molzahn, A. E., de Oliveira, M. P., & Kusumota, L. (2016). The relationship of the spiritual and religious dimensions with quality of life and health of patients with chronic kidney disease: An integrative literature review. Nephrology Nursing Journal: Journal of the American Nephrology Nurses’ Association, 43(5), 411–426. https://pubmed.ncbi.nlm.nih.gov/30550069/ ↵
- Puchalski, C., Jafari, N., Buller, H., Haythorn, T., Jacobs, C., & Ferrell, B. (2020). Interprofessional spiritual care education curriculum: A milestone toward the provision of spiritual care. Journal of Palliative Medicine, 23(6), 777–784. https://doi.org/10.1089/jpm.2019.0375 ↵
- Pilger, C., Molzahn, A. E., de Oliveira, M. P., & Kusumota, L. (2016). The relationship of the spiritual and religious dimensions with quality of life and health of patients with chronic kidney disease: An integrative literature review. Nephrology Nursing Journal: Journal of the American Nephrology Nurses’ Association, 43(5), 411–426. https://pubmed.ncbi.nlm.nih.gov/30550069/ ↵
- Puchalski, C., Jafari, N., Buller, H., Haythorn, T., Jacobs, C., & Ferrell, B. (2020). Interprofessional spiritual care education curriculum: A milestone toward the provision of spiritual care. Journal of Palliative Medicine, 23(6), 777–784. https://doi.org/10.1089/jpm.2019.0375 ↵
- GW School of Medicine & Health Sciences. (n.d.). Clinical FICA tool. https://smhs.gwu.edu/spirituality-health/program/transforming-practice-health-settings/clinical-fica-tool ↵
- GW School of Medicine & Health Sciences. (n.d.). Clinical FICA tool. https://smhs.gwu.edu/spirituality-health/program/transforming-practice-health-settings/clinical-fica-tool ↵
- “shutterstock_149010437.jpg” by Robert Adrian Hillman is used under license from Shutterstock.com ↵
- Vallotton, C. D., & Fischer, K. W. (2008). Cognitive development. Encyclopedia of Infant and Early Childhood Development. Academic Press. pp. 286-298. https://doi.org/10.1016/B978-012370877-9.00038-4 ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of StatPearls by Orenstein & Lewis and is licensed under CC BY 4.0 ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- This work is a derivative of Psychology 2e by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction ↵
- Vallotton, C. D., & Fischer, K. W. (2008). Cognitive development. Encyclopedia of Infant and Early Childhood Development. Academic Press. pp. 286-298. https://doi.org/10.1016/B978-012370877-9.00038-4 ↵
- McLeod, S. (2020, December 7). Piaget’s theory and stages of development. SimplyPsychology. https://www.simplypsychology.org/piaget.html ↵
- Schofield, D. W. (2018, December 26). Cognitive deficits. Medscape. https://emedicine.medscape.com/article/917629-overview ↵
- Schofield, D. W. (2018, December 26). Cognitive deficits. Medscape. https://emedicine.medscape.com/article/917629-overview ↵
- Center on the Developing Child. (n.d.). Resilience. Harvard University. https://developingchild.harvard.edu/science/key-concepts/resilience/ ↵
- Center on the Developing Child. (n.d.). Resilience. Harvard University. https://developingchild.harvard.edu/science/key-concepts/resilience/ ↵
- Center on the Developing Child. (n.d.). Resilience. Harvard University. https://developingchild.harvard.edu/science/key-concepts/resilience/ ↵
- American Psychiatric Association. (n.d.). DSM-5 fact sheets. https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/dsm-5-fact-sheets ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
- Oxford Learner’s Dictionaries. (n.d.). Inclusion. Oxford University Press. https://www.oxfordlearnersdictionaries.com/us/definition/english/inclusion ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵
An assessment of a client’s level of consciousness and orientation, appearance and general behavior, speech, motor activity, affect and mood, thought and perception, attitude and insight, and cognitive abilities.
Motor restlessness.
Uncontrolled, involuntary movement.
A state of reduced awareness to stimuli.
An onset of an abnormal mental state, often with fluctuating levels of consciousness, disorientation, irritability, and hallucinations.
A moderate reduction in the client's level of awareness so that mild to moderate stimuli do not awaken the client. When arousal does occur, the patient is slow to respond.
A state of unresponsiveness unless a vigorous stimulus is applied, such as a sternal rub.
A state of unarousable unresponsiveness, where vigorous noxious stimuli may not elicit reflex motor responses.
Hair, clothes, or hygiene appears untidy, disordered, unkempt, or messy.
Speaking with many unnecessary or tedious details without getting to the point of the conversation.
A conversation in which the client talks without stating anything related to the question or their speech in general is vague and meaningless.
A condition of purposeless, non goal-directed activity.
A condition of extremely slow physical movements, slumped posture, or slow speech patterns.
A client’s expression of emotion.
The predominant emotion expressed by an individual.
A rapid change in emotional responses, mood, or affect that are inappropriate for the moment or the situation.
Exhibiting depression.
A pathologically elevated sense of well-being.
Normal affect and mood with a wide range of emotion appropriate for the situation.
Consistency of verbal and nonverbal communication.
Diminished range and intensity.
No emotional expression.
The inability to describe emotions with how one is feeling.
The inability to experience or even imagine any pleasant emotion.
A lack of feelings, emotions, interests or concerns.
Fixed, false belief not held by cultural peers and persisting in the face of objective contradictory evidence.
A state of false attribution to the self of great ability, knowledge, importance or worth, identity, prestige, power, accomplishment.
A condition characterized by delusions of persecution.
Persistent thoughts, ideas, images, or impulses that are experienced as intrusive or inappropriate and result in anxiety, distress, or discomfort.
Obsessional thinking involving excessive, repetitive thoughts that interfere with other forms of mental activity.
False sensory perceptions not associated with real external stimuli that can include any of the five senses (auditory, visual, gustatory, olfactory and tactile).
Misperceptions of real stimuli.
Fast moving and often repetitive thought patterns that can be overwhelming.
A state where the client frequently shifts from one topic to another with rapid speech, making it seem fragmented.
Jumping from one idea to an unrelated idea in the same sentence. For example, the client might state, “I like to dance, my feet are wet.
Severely disorganized and virtually incomprehensible speech or writing, marked by severe loosening of associations.
Stringing words together that rhyme without logical association and do not convey rational meaning.
Threats or acts of life-threatening harm towards another person.
Thoughts of killing oneself.
A term used to describe an individual who harms themselves with intent to end their life but does not die as a result of their actions.
An individual who has a plan for suicide, has the means to injury oneself, and has the intent to die.
The client's ability to identify the existence of a problem and to have an understanding of its nature.
When the client projects (i.e., transfers) their feelings to the nurse.
The mental action or process of acquiring knowledge and understanding through thought, experience, and the senses.
Referring to the client’s attention being easily drawn to unimportant or irrelevant external stimuli.
A tendency for the examiner to displace (transfer) their own feelings onto the client and then these feelings may influence the client.
A component of the nursing assessment process that obtains additional subjective data to detect risks and identify treatment opportunities and resources.
The patient’s primary reasons for seeking care.
Intentional self-inflicted destruction of body tissue without suicidal intention and for purposes not socially sanctioned.
Refers to the patterns of interactions among relatives, their roles and relationships, and the various factors that shape their interactions.
A sense of connection to something larger than oneself and typically involves a search for meaning and purpose in life.
Physical, social, and cognitive changes that occur continuously throughout one’s life.
A term used to describe impairment in mental processes that drive how an individual understands and acts in the world, affecting the acquisition of information and knowledge.
A diagnostic term that describes intellectual and adaptive functioning deficits identified during the developmental period.
The ability to rise above circumstances or meet challenges with fortitude.
A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot know everything about other cultures, and approach learning about other cultures as a life-long goal and process.
The practice of providing equal access to opportunities and resources for people who might otherwise be excluded or marginalized, such as those having physical or mental disabilities or belonging to other minority groups.

