The Diagnosis Standard of Practice by the American Nurses Association states, “The registered nurse analyzes assessment data to determine actual or potential diagnoses, problems, and issues.”[1] Review the competencies for the Diagnosis Standard of Practice for registered nurses in the following box.
ANA’s Diagnosis Competencies[2]
The registered nurse:
- Identifies actual or potential risks to the health care consumer’s health and safety or barriers to health, which may include, but are not limited to, interpersonal, systematic, cultural, socioeconomic, or environmental circumstances.
- Uses assessment data, standardized classification systems, technology, and clinical decision support tools to articulate actual or potential diagnoses, problems, and issues.
- Identifies the health care consumer’s strengths and abilities, including, but not limited to, support systems, health literacy, and engagement in self-care.
- Verifies the diagnoses, problems, and issues with the health care consumer and interprofessional colleagues.
- Prioritizes diagnoses, problems, and issues based on mutually established goals to meet the needs of the health care consumer across the health-illness continuum and the care continuum.
- Documents diagnoses, problems, strengths, and issues in a manner that facilitates the development of the expected outcomes and collaborative plan.
Review how to analyze assessment data, make hypotheses, and create nursing diagnoses statements in the “Diagnosis” section of the “Nursing Process” chapter in Open RN Nursing Fundamentals.
Nursing Diagnoses
A nursing diagnosis is “a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability to that response, by an individual, family, group, or community.”[3] Nursing diagnoses are customized to each patient and drive the development of the nursing care plan. The nurse should refer to an evidence-based care planning resource and review the definitions and defining characteristics of the hypothesized nursing diagnoses.
Recall that nursing diagnoses are different from medical diagnoses and mental health diagnoses. Medical diagnoses focus on medical problems that have been identified by the physician, physician’s assistant, or advanced nurse practitioner. Mental health diagnoses are established by mental health experts, such as psychiatrists, psychologists, and advanced practice psychiatric-mental health nurses, using the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). See Figure 4.5[4] for an illustration of several mental health diagnoses.
Nursing diagnoses focus on the human response to health conditions and life processes and are established by registered nurses. Patients with the same mental health diagnosis will often respond differently and thus have different nursing diagnoses. For example, two clients may have the same diagnosis of Major Depressive Disorder. However, one client may demonstrate a high risk for suicide whereas another patient may experience impaired nutrition due to lack of appetite. The nurse must consider these different responses when creating an individualized nursing care plan.
Prioritization
After identifying nursing diagnoses, the next step is prioritizing specific needs of the patient. Prioritization is the process of identifying the most significant problems and the most important interventions to implement based on a client’s current status.
It is essential that life-threatening concerns and crises are quickly identified and addressed immediately. Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns. Nurses must recognize cues signaling a change in patient condition, apply evidence-based practices in a crisis, and communicate effectively with interprofessional team members. Most client care situations fall somewhere between a crisis and routine care.
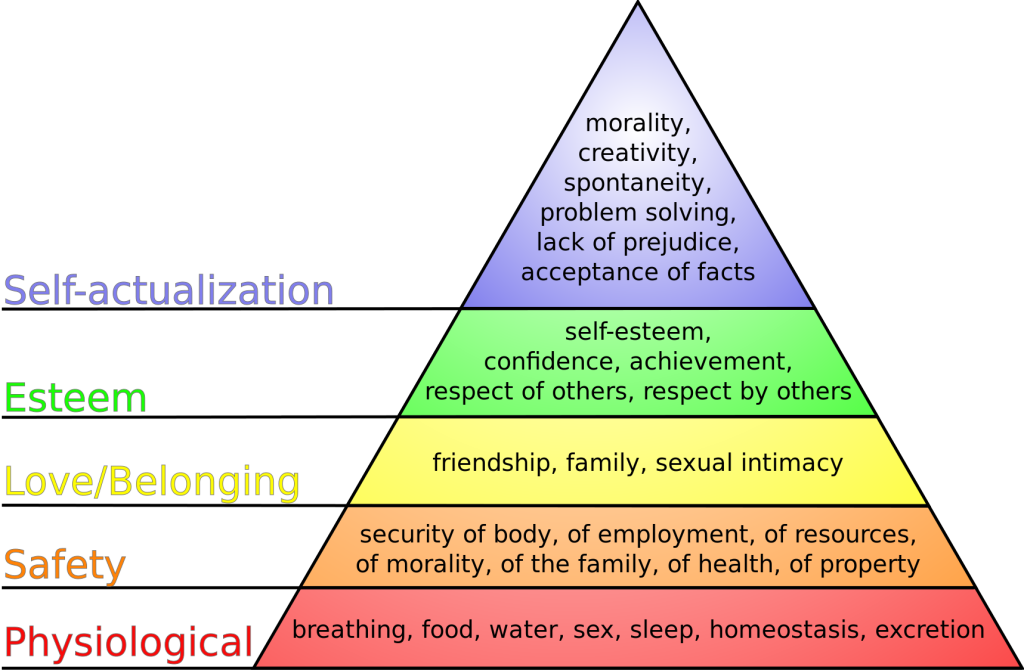
Maslow’s Hierarchy of Needs is commonly used to prioritize the most urgent patient needs. It is based on the theory that people are motivated by five levels of needs: physiological, safety, love, esteem, and self-actualization. The bottom levels of the pyramid represent the priority physiological needs intertwined with safety, whereas the upper levels focus on belonging, esteem, and self-actualization. Physiological needs must be met before focusing on higher level needs.[5]For example, priorities for a client experiencing mania are the need for food, fluid, and sleep, as well as controlling the agitation and impulsivity to ensure safety. These needs would need to be met before focusing on strategies to improve relationships with family and friends, build respect and acceptance for self and others, and engage in activities promoting personal growth. It is important to note that although safety is not described as a top priority in this theory, nurses must always prioritize safety needs in addition to physiological needs. See Figure 4.6[6] for an image of Maslow’s Hierarchy of Needs.
Common Nursing Diagnosis for Mental Health Conditions
Commonly used nursing diagnoses related to caring for clients with mental health conditions are included in Table 4.4. As always, when providing client care, refer to a current, evidence-based nursing care planning resource.
Table 4.4 Common Nursing Diagnoses Related to Mental Health[7]
| Nursing Diagnosis | Definition | Selected Defining Characteristics |
|---|---|---|
| Risk for Suicide | Susceptible to self-inflicted, life-threatening injury. |
|
| Ineffective Coping | A pattern of impaired appraisal of stressors with cognitive and/or behavioral efforts that fails to manage demands related to well-being. |
|
| Readiness for Enhanced Coping | A pattern of effective appraisal of stressors with cognitive and behavioral efforts to manage demands related to well-being, which can be strengthened. |
|
| Self-Neglect | A collection of culturally framed behaviors involving one or more self-care activities in which there is a failure to maintain a socially accepted standard of health and well-being. |
|
| Fatigue | An overwhelming sustained sense of exhaustion and decreased capacity for physical and mental work at the usual level. |
|
| Imbalanced Nutrition: Less than Body Requirements | Intake of nutrients insufficient to meet metabolic needs. |
|
| Constipation | Decrease in normal frequency of defecation accompanied by difficult or incomplete passage of stool and/or passage of excessively dry, hard stool. |
|
| Sleep Deprivation | Prolonged periods of time without sustained natural, periodic suspension of relative consciousness that provides rest. |
|
| Social Isolation | Aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state. |
|
| Chronic Low Self-Esteem | Negative evaluation and/or feelings about one’s own capabilities, lasting at least three months. |
|
| Hopelessness | Subjective state in which an individual sees limited or no alternatives or personal choices available and is unable to mobilize energy on own behalf. |
|
| Spiritual Distress | A state of suffering related to the impaired ability to experience meaning in life through connections with self, others, the world, or a superior being. |
|
| Readiness for Enhanced Knowledge | A pattern of cognitive information related to a specific topic or its acquisition, which can be strengthened. |
|
Sample Case A
During an interview with a 32-year-old client diagnosed with Major Depressive Disorder, Mr. J. exhibited signs of a sad affect and hopelessness. He expressed desire to die and reported difficulty sleeping and a lack of appetite with weight loss. He reports he has not showered in over a week, and his clothes have a strong body odor. The nurse analyzed this data and created four nursing diagnoses using a nurse care plan reference[8]:
- Hopelessness related to social isolation
- Risk for Suicide as manifested by reported desire to die
- Imbalanced Nutrition: Less than Body Requirements related to insufficient dietary intake
- Self-Neglect related to insufficient personal hygiene
The nurse established the top priority nursing diagnosis of Risk for Suicide and immediately screened for suicidal ideation and a plan using the Patient Safety Screener.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- “Mental_Disorder_Silhouette.png” by Paget Michael Creelman is licensed under CC BY-SA 4.0 ↵
- Maslow, A. H. (1943). A theory of human motivation. Psychological Review, 50(4), 370–396. https://doi.org/10.1037/h0054346 ↵
- “Maslow's hierarchy of needs.svg” by J. Finkelstein is licensed under CC BY-SA 3.0 ↵
- McLeod, S. (2020, December 7). Piaget’s theory and stages of development. SimplyPsychology. https://www.simplypsychology.org/piaget.html ↵
- Ackley, B., Ladwig, G., Makic, M. B., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care (12th ed.). Elsevier. ↵
Used to prioritize the most urgent patient needs.

