Severe substance use disorders, also called addictions, were once considered a moral failing or character flaw but are now known to be chronic illnesses. Scientific evidence shows that addiction to alcohol or drugs is a chronic brain disease that has potential for relapse and recovery.[1]
All addictive substances have powerful effects on the brain. These effects account for the euphoric or intensely pleasurable feelings that people experience during their initial use of alcohol or other substances. These feelings motivate people to use those substances again and again, despite the risks for significant harm. As individuals continue to misuse alcohol or other substances, progressive changes, called neuroadaptations, occur in the structure and function of the brain. These neuroadaptations drive the transition from controlled, occasional substance use to chronic misuse that can be difficult to control and can endure long after an individual stops using the substances. These changes can lead to the need for increased amounts of substances to achieve the same effect, referred to as tolerance. They may produce continued, periodic craving for the substance that can lead to relapse. More than 60 percent of people treated for a substance use disorder experience relapse within the first year after they are discharged from treatment, and a person can remain at increased risk of relapse for many years.[2]
For many people, initial substance use involves an element of impulsivity (i.e., acting without foresight or regard for the consequences). For example, an adolescent may impulsively take a first drink, smoke a cigarette, experiment with marijuana, or succumb to peer pressure and try a party drug like Ecstasy. If the experience is pleasurable, this feeling positively reinforces the substance use, making the person more likely to take the substance again. Another person may take a substance to relieve negative feelings such as stress, anxiety, or depression. In this case, the temporary relief the substance brings from the negative feelings reinforces substance use, increasing the likelihood that the person will use again.[3]
Many other environmental and social stimuli can reinforce a behavior. For example, peer approval positively reinforces substance use for some people. Likewise, if drinking or using drugs with others provides a feeling of relief from social isolation, substance use is reinforced.[4]
Eventually, in the absence of the substance, a person may experience negative emotions such as stress, anxiety, or depression or the individual may feel physically ill. This is called withdrawal, which often leads the person to use the substance again to relieve the withdrawal symptoms. As use becomes an ingrained behavior, impulsivity shifts to compulsivity, and the primary drivers of repeated substance use shift from positive reinforcement (feeling pleasure) to negative reinforcement (feeling relief) as the person seeks to stop the negative feelings and physical illness that accompany withdrawal. Eventually, the person begins taking the substance not to get “high,” but rather to escape the “low” feelings from withdrawal. Compulsive substance seeking is a key characteristic of addiction, as well as loss of control over use. Compulsivity helps to explain why many people with addiction experience relapses after abstinence.[5]
Three regions of the brain are the key components in the development and persistence of substance use disorders: the basal ganglia, the extended amygdala, and the prefrontal cortex:
- The basal ganglia controls the rewarding, pleasurable effects of substance use and is responsible for the formation of habitual substance taking. Two subregions of the basal ganglia are particularly important in substance use disorders:
- The nucleus accumbens, involved in motivation and the experience of reward.
- The dorsal striatum, involved in forming habits and other routine behaviors.
- The extended amygdala is involved in the stress response and the feelings of unease, anxiety, and irritability that typically accompany substance withdrawal.
- The prefrontal cortex is involved in executive function (e.g., the ability to organize thoughts and activities, prioritize tasks, manage time, and make decisions), including exerting control over substance use.
These changes in the brain persist long after substance use stops and are associated with a high incidence of relapse with substance use disorders.
Addiction Cycle
The addiction process involves a three-stage cycle that becomes more severe as a person continues to misuse substances, causing neuroadaptions in brain function that reduce a person’s ability to control their substance use. Each stage is associated with one of the brain regions previously described (i.e., basal ganglia, extended amygdala, and prefrontal cortex). See Figure 14.7[6] for an image of the brain regions associated with the three stages of addiction. This three-stage model provides a useful way to understand the symptoms of addiction, the ways it can be prevented and treated, and the steps for recovery.[7]
These are the three stages of addiction:
- Binge/Intoxication: The stage at which an individual consumes an intoxicating substance and experiences its rewarding or pleasurable effects.
- Withdrawal/Negative Affect: The stage at which an individual experiences a negative emotional state in the absence of the substance.
- Preoccupation/Anticipation: The stage at which one seeks substances again after a period of abstinence.
![Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health [Internet]. Washington (DC): US Department of Health and Human Services; 2016 Nov. Figure 2.3, The Three Stages of the Addiction Cycle and the Brain Regions Associated with Them. Used under Fair Use. Available from https://www.ncbi.nlm.nih.gov/books/NBK424849/figure/ch2.f3 Illustration showing Brain Regions Associated With the Three Stages of Addiction, with textual labels](https://opentextbooks.uregina.ca/app/uploads/sites/293/2022/03/ch2f3.jpg)
Binge/Intoxication
All addictive substances produce feelings of pleasure. These “rewarding effects” positively reinforce their use and increase the likelihood of repeated use. The rewarding effects of substances involve activity in the nucleus accumbens, including activation of the brain’s dopamine and opioid signaling system. Studies show that antagonists, or inhibitors, of dopamine and opioid receptors can block drug and alcohol-seeking behaviors.[8] See Figure 14.8[9] for an illustration of rewarding actions of addictive substances on the nucleus accumbens.
![Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health [Internet]. Washington (DC): US Department of Health and Human Services; 2016 Nov. Figure 2.5, Actions of Addictive Substances on the Brain. Used under Fair Use. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424849/figure/ch2.f5/ Illustration showing Rewarding Actions of Addictive Substances on the Nucleus Accumbens (NAc)](https://opentextbooks.uregina.ca/app/uploads/sites/293/2022/08/ch2f5.jpg)
Dopamine neurons (DA) are activated, either directly or indirectly, by all addictive substances, but particularly by stimulants and nicotine.[10]
The brain’s opioid system includes naturally occurring opioid molecules (i.e., endorphins) and three types of opioid receptors (i.e., mu, delta, and kappa) and plays a key role in mediating the rewarding effects of opioids and alcohol. Activation of the opioid system stimulates the nucleus accumbens (NAc) directly or indirectly through the GABA and dopamine (DA) system.[11]
Tetrahydrocannabinol (THC), the primary psychoactive component of marijuana, targets GABA neurons that stimulate the dopamine (DA) system, as well as directly stimulating the nucleus accumbens (NAc).[12]
Activation of the brain’s reward system by alcohol and drugs not only generates the pleasurable feelings associated with those substances, but also ultimately triggers changes in the way a person responds to stimuli associated with the use of those substances. A person learns to associate the stimuli present while using a substance, including people, places, drug paraphernalia, and even internal states, such as mood, with the substance’s rewarding effects. Over time, these stimuli can activate the dopamine system on their own and trigger powerful urges to take the substance. These “cravings” can persist even after the rewarding effects of the substance have diminished. As a result, exposure to people, places, or things previously associated with substance use can serve as triggers or cues that promote substance seeking and taking, even in people who are in recovery.[13]
Withdrawal/Negative Affect Stage
The withdrawal/negative affect stage of addiction follows the binge/intoxication stage, and, in turn, sets up future rounds of binge/intoxication. During this stage, a person who has been using alcohol or drugs experiences withdrawal symptoms, including negative emotions and symptoms of physical illness when they stop taking the substance. Symptoms of withdrawal may occur with all addictive substances, although they vary in intensity and duration depending on both the type of substance and the severity of use. The negative feelings associated with withdrawal are thought to come from two sources: diminished activation in the reward circuitry of the basal ganglia and activation of the brain’s stress systems in the extended amygdala.[14]
When used long-term, all addictive substances cause dysfunction in the brain’s dopamine reward system. For example, brain imaging studies in individuals with addictions show long-lasting decreases in dopamine receptors even after stopping substance abuse. See Figure 14.9[15] for an image of brain imaging studies comparing an individual with cocaine addiction to someone without addiction. Decreases in the activity of the dopamine system have also been observed during withdrawal from stimulants, opioids, nicotine, and alcohol. Other studies also show that when an addicted person is given a stimulant, it causes a smaller release of dopamine than when the same dose is given to a person who is not addicted.[16]
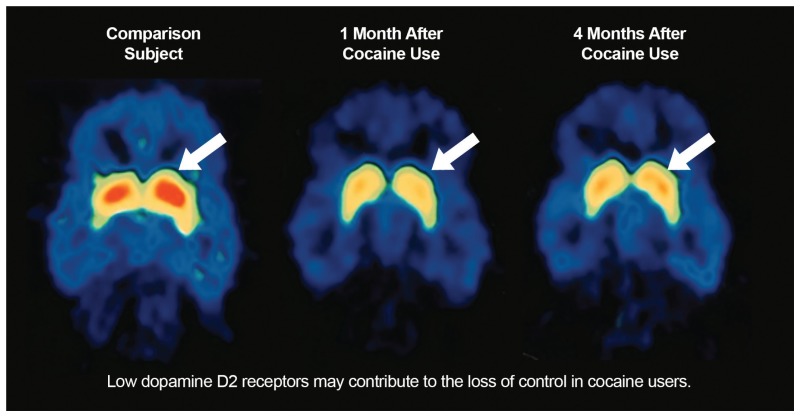
These findings suggest that people addicted to substances experience an overall reduction in the sensitivity of the brain’s reward system (especially in the brain circuits involving dopamine), both to addictive substances and also to natural reinforcers, such as food and sex. This impairment explains why individuals who develop a substance abuse disorder often do not derive the same level of satisfaction or pleasure from once-pleasurable activities and may neglect eating. This loss of reward sensitivity may also account for the compulsive escalation of substance use as addicted individuals attempt to regain the pleasurable feelings the reward system once provided.[17]
At the same time, a second process occurs during the withdrawal stage related to the activation of stress neurotransmitters in the extended amygdala. These stress neurotransmitters include corticotropin releasing factor (CRF), norepinephrine, and dynorphin. These neurotransmitters play a key role in the negative feelings associated with withdrawal and in stress-triggered substance use. When researchers used antagonists to block activation of addicted individuals’ stress neurotransmitter systems, it reduced their substance intake in response to withdrawal and stress.[18]
Preoccupation/Anticipation Stage: Prefrontal Cortex
The preoccupation/anticipation stage of the addiction cycle is the stage in which a person may begin to seek to use substances again after a period of abstinence. In this stage, an addicted person becomes preoccupied with using substances again, referred to as craving. This stage of addiction involves the brain’s prefrontal cortex, the region that controls executive function (e.g., the ability to organize thoughts and activities; prioritize tasks; manage time; make decisions; and regulate one’s own actions, emotions, and impulses). Executive function is essential for a person to make appropriate choices about whether or not to use a substance and to override strong urges to use it, especially when experiencing triggers related to the substance (e.g., being at a party where alcohol is served) or stressful experiences. People with alcohol, cocaine, or opioid use disorders show impairments in executive function, including disruption of decision-making and behavioral inhibition.[19]
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health [Internet]. Washington (DC): US Department of Health and Human Services; 2016 Nov. Figure 2.3, The Three Stages of the Addiction Cycle and the Brain Regions Associated with Them. Used under Fair Use. Available from https://www.ncbi.nlm.nih.gov/books/NBK424849/figure/ch2.f3/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health [Internet]. Washington (DC): US Department of Health and Human Services; 2016 Nov. Figure 2.5, Actions of Addictive Substances on the Brain. Used under Fair Use. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424849/figure/ch2.f5/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. Used under Fair Use. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
Progressive changes in the structure or function of the brain due to misue of alcohol or other substances.

