Mental health is an essential component of health. The World Health Organization (WHO) defines health as a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. Mental health is a state of well-being in which an individual realizes their own abilities, copes with the normal stresses of life, works productively, and contributes to their community. The promotion, protection, and restoration of mental health is a vital concern of individuals, nurses, communities, and societies throughout the world.[1]
According to the American Psychiatric Association, mental illness is a health condition involving changes in emotion, thinking, or behavior (or a combination of these) associated with emotional distress and problems functioning in social, work, or family activities.[2] Mental illness is common in the United States. Nearly one in five (19 percent) of adults experience some form of mental illness, one in twelve (8.5 percent) have a substance use disorder, and one in 24 (4 percent) have a serious mental illness.[3]
Poor mental health increases the risk of chronic physical illnesses, such as heart disease, cancer, and strokes, and can lead to thoughts and intentions of suicide. Suicide is a common symptom associated with mental illness and is the second leading cause of death in Americans aged 15-34.[4]
View the following YouTube video on WHO’s Special Initiative on Mental Health (2019-2023)[5]: WHO Special Initiative on Mental Health (2019-2023)
Mental Health Continuum
Mental health fluctuates over the course of an individual’s life span and can range from well-being to emotional problems and/or mental illness as indicated on the mental health continuum illustrated in Figure 1.1.[6],[7],[8]
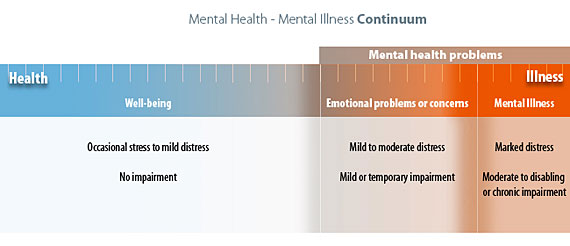
Well-being is on the “healthy” range of the mental health continuum in which individuals are experiencing a state of good mental and emotional health. They may experience stress and discomfort resulting from occasional problems of everyday life, but they are able to cope effectively with these stressors and experience no impairments to daily functioning.
On the other end of the mental health continuum are mental health problems where individuals have progressively more difficulty coping with serious problems and stressors. Within this range are two categories: emotional problems/concerns and mental illness. For individuals experiencing emotional problems, discomfort has risen to a level of mild to moderate distress, and they are experiencing mild or temporary impairments in functioning, such as insomnia, lack of concentration, or loss of appetite. As their level of distress increases, they may seek treatment and often start with visiting their primary health care provider.
Emotional problems become classified as “mental illness” when an individual’s level of distress becomes significant, and they have moderate to severe impairment in daily functioning at work, school, or home. Mental illness includes relatively common disorders, such as depression and anxiety, as well as less common disorders such as schizophrenia. Mental illness is characterized by alterations in thinking, mood, or behavior. The term serious mental illness refers to mental illness that causes disabling functional impairment that substantially interferes with one or more major life activities. The Americans With Disabilities Act defines major life activities as, “caring for oneself, performing manual tasks, seeing, hearing, eating, sleeping, walking, standing, lifting, bending, speaking, breathing, learning, reading, concentrating, thinking, communicating, and working.”[9] Examples of serious mental illnesses that commonly interfere with major life activities include major depressive disorder, schizophrenia, and bipolar disorder.[10] Individuals with serious mental illnesses may experience long-term impairments ranging from moderate to disabling in nature, but many can lead productive lives with effective treatment. Roughly half of schizophrenia patients recovered or significantly improved over the long-term, suggesting that functional remission is possible.[11],[12]
Mental health providers, such as psychiatrists, psychologists, therapists, social workers, or advanced practice mental health nurses, use the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) published by the American Psychiatric Association to assess a client’s signs and symptoms and determine a mental health diagnosis. The manual lists diagnostic criteria including feelings, behaviors, and time frames to be officially classified as a mental health disorder.[13]
There are more than 200 types of mental illness. People can experience different types of mental health disorders, and different disorders can occur at the same time or vary in intensity over time. Mental illness can be ongoing, occur over a short period of time, or be episodic (i.e., it comes and goes with discrete beginnings and ends).[14]
Read more information about specific mental health disorders at the Medline Plus Mental Health and Behavior webpage.
Assessing Dysfunction and Impairment
Mental health disorders have been defined as a type of dysfunction that causes distress or impaired functioning and deviates from typical or expected behavior according to societal or cultural standards. This definition includes three components referred to as dysfunction, distress, and deviance.[15]
Dysfunction includes disturbances in a person’s thinking, emotional regulation, or behavior that reflects significant dysfunction in psychological, biological, or developmental processes underlying mental functioning. In other words, dysfunction refers to a breakdown in cognition, emotion, and/or behavior. For instance, an individual experiencing a delusion that they are an omnipotent deity has a breakdown in cognition because their thought processes are not consistent with reality. An individual who is unable to experience pleasure has a breakdown in emotion, and an individual who is unable to leave home and attend work due to fear of having a panic attack is exhibiting a breakdown in behavior.[16]
Distress refers to psychological and/or physical pain. Simply put, distress refers to suffering. For example, the loss of a loved one causes anyone to experience emotional pain, distress, and a temporary impairment in functioning. Impairment refers to a limited ability to engage in activities of daily living (i.e., they cannot maintain personal hygiene, prepare meals, or pay bills) or participate in social events, work, or school. Impairment can also interfere with the ability to perform important life roles such as a caregiver, parent, or student.[17]
Deviance refers to behavior that violates social norms or cultural expectations because one’s culture determines what is “normal.” When a person is described as “deviant,” it means they are not following the stated and unstated rules of their society (referred to as social norms).[18]
Nurses complete and document initial and ongoing assessments of dysfunction, distress, and behavior associated with an individual’s diagnosed mental health disorder. The World Health Organization Disability Assessment Scale (WHODAS) is a tool recommended in the DSM-5 to assess impairments resulting from mental illness.[19] The WHODAS is a generic assessment instrument that provides a standardized method for measuring health and disability across cultures.[20] The WHODAS assesses functioning in six domains: cognition, mobility, self-care, getting along, life activities, and participation.[21]
View the WHODAS 2.0 webpage.
The Global Assessment of Functioning (GAF) was historically used to rate the seriousness of a mental illness and measure how symptoms affect an individual’s day-to-day life on a scale of 0 to 100. It is an overall (global) measure of how clients are doing and rates psychological, social, and occupational functioning on the continuum from mental well-being to serious mental illness. The higher the score, the better the daily functioning. The GAF was omitted from the DSM-5 because it had questionable validity and reliability, but some government agencies and insurance companies continue to include it in paperwork to assess client functioning.[22]
Recovery
Mental illness is treatable. Research shows that people with mental illness can get better, and many recover completely.[23] The majority of individuals with mental illness continue to function in their daily lives. Recovery refers to a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential.[24] Dimensions that support a life in recovery include the following:
- Health: Overcoming or managing one’s disease(s), as well as living in a physically and emotionally healthy way
- Home: Having a stable and safe place to live
- Purpose: Participating in meaningful daily activities, such as a job, school, volunteerism, family caretaking, or creative endeavors, and the independence, income, and resources to participate in society
- Community: Enjoying relationships and social networks that provide support, friendship, love, and hope
Early Signs of Mental Health Problems
Mental health problems are common. We all experience problems and stressors from daily living at the milder end of the mental health continuum, and at some point in our lives, we are likely to experience emotional problems or concerns. Mental illness, though less common, is nevertheless a frequent occurrence, and it is estimated that approximately one in five Americans will personally experience a mental illness in their lifetime.[25],[26]
Nurses in all care settings must recognize signs and symptoms of diagnosed and undiagnosed emotional and mental health problems in clients. Each mental health disorder has specific signs and symptoms, but common signs of mental health problems in adults and adolescents are as follows[27]:
- Excessive worrying or fear
- Excessive sad or low feelings
- Confused thinking or problems concentrating and learning
- Extreme mood changes, including uncontrollable “highs” or feelings of euphoria
- Prolonged or strong feelings of irritability or anger
- Avoidance of friends and social activities
- Difficulty understanding or relating to other people
- Changes in sleeping habits or feeling tired and low energy
- Changes in eating habits, such as increased hunger or lack of appetite
- Changes in sex drive
- Disturbances in perceiving reality referred to as hallucinations (i.e., when a person senses things that don’t exist in reality)
- Inability to perceive changes in one’s own feelings, behavior, or personality (i.e., lack of insight)
- Misuse of substances like alcohol, drugs, or prescription medications
- Multiple physical ailments without obvious causes (such as headaches, stomachaches, or vague and ongoing “aches and pains”)
- Thoughts of suicide
- Inability to carry out daily activities or handle daily problems and stress
- Intense fear of weight gain or being overly concerned with appearance
Mental health disorders can also be present in young children. Because children are still learning how to identify and talk about thoughts and emotions, their most obvious symptoms are behavioral or complaints of physical symptoms. Behavioral symptoms in children can include the following[28]:
- Changes in school performance
- Excessive worry or anxiety, for example fighting to avoid going to bed or school
- Hyperactive behavior
- Frequent nightmares
- Frequent disobedience or aggression
- Frequent temper tantrums
View the following YouTube video about warning signs of mental health problems[29]: 10 Common Warning Signs of a Mental Health Condition
Cultural Impact
Cultural values and beliefs impact how a person views certain ideas or behaviors. In the case of mental health, it can impact whether or not the individual seeks help, the type of help sought, and the support available. Every individual has different cultural beliefs and faces a unique journey to recovery. In general, historically marginalized communities in the United States are less likely to access mental health treatment, or they wait until symptoms are severe before seeking assistance.[30]
Four ways that culture can impact mental well-being are the following[31]:
- Cultural stigma. Every culture has a different perspective on mental health, and most cultures have a stigma surrounding mental health. Mental health challenges may be considered a weakness and something to hide, which can make it harder for those struggling to talk openly and ask for help.
- Describing symptoms. Culture can influence how people describe or feel about their symptoms. It can affect whether someone chooses to recognize and talk openly about physical symptoms, emotional symptoms, or both. For example, members of the Amish community are typically stoic and endure physical and emotional pain without complaining.
- Community support. Cultural factors can determine how much support someone gets from their family and community when it comes to mental health. Because of existing stigma, it can be challenging for individuals to find mental health treatment and support.
- Resources. When looking for mental health treatment, it can be difficult to find resources and treatment options that take into account a specific culture’s concerns and needs.
Nurses can help clients by understanding the role culture plays in their mental health. If potential signs of undiagnosed or poorly managed mental health disorders are present, nurses should make appropriate referrals for further assessment and follow-up.
Read more about cultural diversity and providing culturally responsive care in the “Diverse Patients” chapter of Open RN Nursing Fundamentals.
Causes of Mental Illness
Mental health researchers have developed several theories to explain the causes of mental health disorders, but they have not reached consensus. One factor in which they all agree is that an individual is not at fault for the condition, and they cannot simply turn symptoms on or off at will. There are likely several factors that combine to trigger a mental health disorder, including environmental, biological, and genetic factors.[32]
Environmental Factors
Individuals are affected by broad social and cultural factors, as well as by unique factors in their personal environments. Social factors such as racism, discrimination, poverty, and violence (often referred to as “social determinants of health”) can contribute to mental illness.
Read more about addressing social determinants of health in the “Advocacy” chapter of Open RN Nursing Management and Professional Concepts.
Additionally, it is estimated that 61% of adults have experienced early adverse childhood experiences (ACEs) such as abuse, neglect, or growing up in a household with violence, mental illness, substance misuse, incarceration, or divorce. Chronic stress from ACEs can change brain development and affect how the body responds to stress. ACEs are linked to chronic health problems, mental illness, and substance misuse in adulthood.[33],[34] See Figure 1.2[35] for an image of adverse childhood experiences.
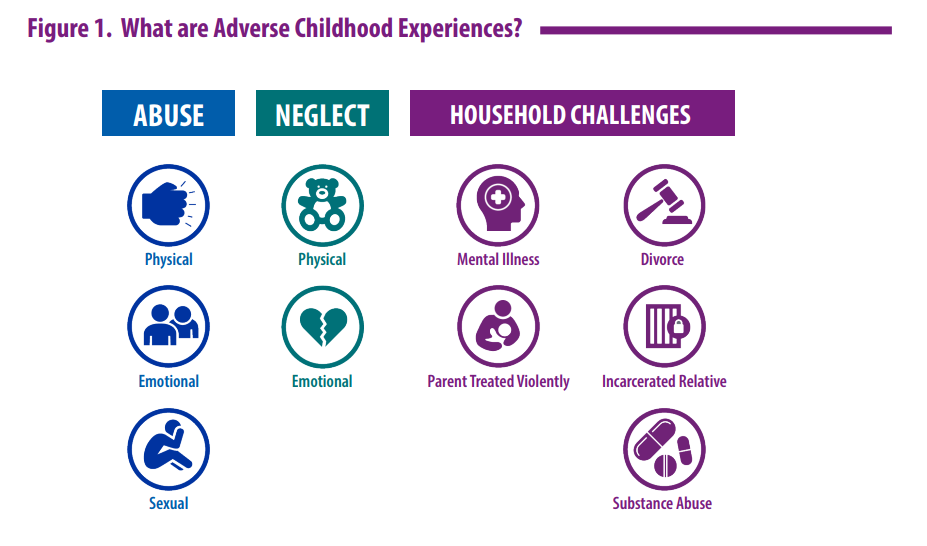
Individual trauma resulting from an event, series of events, or set of circumstances that is experienced as physically or emotionally harmful can have lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.[36] Read more about ACEs and addressing individual trauma in the “Introduction to Trauma-Informed Care” section of this chapter.
Take the Adverse Childhood Experiences Questionnaire for Adults to better understand how previous experiences can affect one’s well-being.
Current stressors such as relationship difficulties, the loss of a job, the birth of a child, a move, or prolonged problems at work can also be important contributory environmental factors.[37]
Biological Factors
Scientists believe the brain can have an imbalance of neurotransmitters, such as dopamine, acetylcholine, gamma-aminobutyric acid (GABA), norepinephrine, glutamate, and serotonin, resulting in changes in behavior, mood, and thought. While causes of fluctuations in brain chemicals aren’t fully understood, contributing factors can include physical illness, hormonal changes, reactions to medication, substance misuse, diet, and stress.[38]
Some studies also suggest that depressive and bipolar disorders are accompanied by immune system dysregulation and inflammation.[39]
Genetics
There appears to be a hereditary pattern to some mental illnesses. For example, individuals with major depressive disorder often have parents or other close relatives with the same illness. Research continues to investigate genes involved in specific disorders so that treatment can be effectively targeted to the individual.[40]
View the following YouTube video on causes of mental illness[41]: Understanding the Biology of Mental Illness
WHO Guidelines for Mental Health Care
It is vital for nurses to protect and promote the mental well-being of all individuals and address the needs of individuals with diagnosed mental disorders.[42] The World Health Organization (WHO) published the Mental Health Intervention Guide for nurses and primary health care providers that provides evidence-based guidance and tools for assessing and managing priority mental health and substance use disorders using clinical decision-making protocols. Essential principles for providing mental health care include promoting respect and dignity for the individuals seeking care; using effective communication skills to ensure care is provided in a nonjudgmental, nonstigmatizing, and supportive manner; and conducting comprehensive assessments.[43]
Promoting Respect and Dignity
Individuals with mental health and substance use conditions should be treated with respect and dignity in a culturally appropriate manner. Health care professionals should promote the preferences of people with mental health and substance use disorders and support them, their family members, and their loved ones in an inclusive and equitable manner. These are some tips discussed in the WHO Mental Health Intervention Guide[44]:
Do:
- Treat people with mental health and substance use conditions with respect and dignity.
- Protect confidentiality.
- Ensure privacy.
- Provide access to information and explain the proposed treatment risks and benefits in writing when possible.
- Make sure the person provides consent to treatment.
- Promote autonomy and independent living in the community.
- Provide access to decision-making options.
Don’t:
- Discriminate against people with mental health and substance use conditions.
- Ignore individual preferences.
- Make decisions for or on behalf of individuals.
- Use overly technical language when explaining proposed treatment.
Using Effective Communication Skills
Using effective communication skills promotes quality mental health care. Tips for effective communication from the WHO Mental Health Intervention Guide include the following[45]:
- Create an environment that facilitates open communication.
- Meet the person in a private space, if possible.
- Be welcoming and conduct introductions in a culturally appropriate manner.
- Use culturally appropriate eye contact, body language, and facial expressions that facilitate trust.
- Explain to adults that information discussed during the visit will be kept confidential. (Special considerations regarding “conditional confidentiality” and mandatory reporting for minors are discussed in the “Childhood and Adolescence Disorders” chapter.)
- If caregivers are present, suggest speaking with the client alone (except for young children) and obtain consent from the client to share clinical information.
- When interviewing a young person, consider having another person present who identifies with the same gender to maintain feelings of a psychologically safe environment.
- Involve the person.
- Include the person (and with their consent, their caregivers and family members) in all aspects of assessment and management as much as possible. This includes children, adolescents, adults, and older adults.
- Start by listening.
- Actively listen. Be empathic and sensitive. (Read more about active listening in the “Therapeutic Communication and the Nurse-Client Relationship” chapter.)
- Allow the person to speak without interruption.
- Be patient and ask for clarification of unclear information.
- For children, use language that they can understand. For example, ask about their interests (toys, friends, school, etc.).
- For adolescents, convey that you understand their feelings and situation.
- Be friendly, respectful, and nonjudgmental.
- Always be respectful.
- Be nonjudgmental about an individual’s behaviors and appearances.
- Remain calm and professional.
- Use good verbal communication skills.
- Use simple language. Be clear and concise. Avoid medical terminology only understood by health care professionals.
- Use open-ended questions and other therapeutic communication techniques. (Read more about specific techniques in the “Therapeutic Communication and the Nurse-Client Relationship” chapter.) For example:
- Use open-ended questions: “Tell me more about what happened?”
- Summarize: “So, your brother pushed you off your bike and then laughed when you fell and started crying?”
- Clarify: “To clarify, were you at home or a neighbor’s house when this happened?”
- Summarize and repeat key points at the end of the conversation.
- Allow the person to ask questions about the information provided. For example, “What questions do you have about what we have discussed today?”
- Respond with sensitivity when people disclose traumatic experiences (e.g., sexual assault, violence, or self-harm).
- Thank the person for sharing this sensitive information.
- Show extra sensitivity when discussing difficult topics.
- Remind the person that what they tell you will only be shared with the immediate treatment team to provide the best possible care.
- Acknowledge that it may have been difficult for the person to disclose the information.
Therapeutic Relationship
In all nursing care, the therapeutic relationship with the client is essential. This is especially so in psychiatric care, where the therapeutic relationship is considered to be the foundation of client care and healing.[46] Although nurse generalists are not expected to perform advanced psychiatric interventions, all nurses are expected to engage in compassionate, supportive relationships with their patients and use therapeutic communication as part of the “art of nursing.”[47]
The nurse-client relationship establishes trust and rapport with a specific purpose. It facilitates therapeutic communication and engages the client in decision-making regarding their plan of care. Read more about therapeutic communication and the nurse-client relationship in the “Therapeutic Communication and the Nurse-Client Relationship” chapter.
Conducting Comprehensive Assessments
Clients undergo comprehensive assessments related to their disorder, including mental status examination, psychosocial assessment, physical examination, and review of laboratory results. Specific nursing assessments are further discussed in the “Application of the Nursing Process in Mental Health Care” chapter as well in each “Disorder” chapter. Persons with severe mental health and substance use disorders are two to three times more likely to die of preventable disease like infections and cardiovascular disorders, so it is also important for nurses to advocate for the medical treatment of existing physical disorders.[48]
- World Health Organization. (2018, March 30). Mental health: Strengthening our response. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response ↵
- American Psychiatric Association. (n.d.). What is mental illness? https://www.psychiatry.org/patients-families/what-is-mental-illness ↵
- American Psychiatric Association. (n.d.). What is mental illness? https://www.psychiatry.org/patients-families/what-is-mental-illness ↵
- Centers for Disease Control and Prevention. (2021, July 20). Mental health. https://www.cdc.gov/mentalhealth/index.htm ↵
- World Health Organization (WHO). (2020, July 20). WHO special initiative on mental health (2019-2023) [Video]. YouTube. All rights reserved. https://youtu.be/ti7OIMq7V9I ↵
- “continuum.jpg” by University of Michigan is used with permission. Access the original at https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse ↵
- William, S. (2021, January 18). The continuum between temperament and mental illness as dynamical phases and transitions. Frontiers in Psychiatry, 11, 1617. https://doi.org/10.3389/fpsyt.2020.614982 ↵
- University of Michigan Human Resources. (n.d.). Section 1: What you need to know about mental health problems and substance misuse. https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse ↵
- Office of Federal Contract Compliance Programs. (2009, January 1). ADA Amendments Act of 2008 frequently asked questions. U.S. Department of Labor. https://www.dol.gov/agencies/ofccp/faqs/americans-with-disabilities-act-amendments ↵
- American Psychiatric Association. (n.d.). What is mental illness? https://www.psychiatry.org/patients-families/what-is-mental-illness ↵
- Vita, A., & Barlati, S. (2018). Recovery from schizophrenia: Is it possible? Current Opinion in Psychiatry, 31(3), 246–255. https://doi.org/10.1097/YCO.0000000000000407 ↵
- Rakitzi, S., Georgila, P., & Becker-Woitag, A. P. (2021). The recovery process for individuals with schizophrenia in the context of evidence-based psychotherapy and rehabilitation: A systematic review. European Psychologist, 26(2), 96–111. https://doi.org/10.1027/1016-9040/a000400 ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- Centers for Disease Control and Prevention. (2021, July 20). Mental health. https://www.cdc.gov/mentalhealth/index.htm ↵
- Culture and Psychology by Worthy, Lavigne, and Romero is licensed under CC BY-NC-SA 4.0 ↵
- Culture and Psychology by Worthy, Lavigne, and Romero is licensed under CC BY-NC-SA 4.0 ↵
- Culture and Psychology by Worthy, Lavigne, and Romero is licensed under CC BY-NC-SA 4.0 ↵
- Culture and Psychology by Worthy, Lavigne, and Romero is licensed under CC BY-NC-SA 4.0 ↵
- Office of Federal Contract Compliance Programs. (2009, January 1). ADA Amendments Act of 2008 frequently asked questions. U.S. Department of Labor. https://www.dol.gov/agencies/ofccp/faqs/americans-with-disabilities-act-amendments ↵
- World Health Organization. (2012). Measuring health and disability: Manual for WHO disability assessment schedule (WHODAS 2.0). [Manual]. https://www.who.int/publications/i/item/measuring-health-and-disability-manual-for-who-disability-assessment-schedule-(-whodas-2.0) ↵
- National Academies of Sciences, Engineering, and Medicine. (2016). Measuring specific mental illness diagnoses with functional impairment: Work-shop summary. J. C. Rivard and K. Marton, Rapporteurs. Committee on National Statistics and Board on Behavioral, Cognitive, and Sensory Sciences, Division of Behavioral and Social Sciences and Education. Board on Health Sciences Policy, Institute of Medicine. The National Academies Press. http://elibrary.pcu.edu.ph:9000/digi/NA02/2016/21920.pdf ↵
- Smith, M. (2021, February 6). What is the global assessment of functioning (GAF) scale? WebMD. https://www.webmd.com/mental-health/gaf-scale-facts ↵
- Centers for Disease Control and Prevention. (2021, July 20). Mental health. https://www.cdc.gov/mentalhealth/index.htm ↵
- Center for Substance Abuse Treatment (US). (2014). Trauma-informed care in behavioral health services. https://www.ncbi.nlm.nih.gov/books/NBK207201/ ↵
- William, S. (2021, January 18). The continuum between temperament and mental illness as dynamical phases and transitions. Frontiers in Psychiatry, 11, 1617. https://doi.org/10.3389/fpsyt.2020.614982 ↵
- National Alliance on Mental Illness (NAMI). (2022, June). Mental health by the numbers. https://www.nami.org/mhstats#:~:text=21%25%20of%20U.S.%20adults%20experienced,represents%201%20in%2020%20adults ↵
- National Alliance on Mental Illness. (n.d.). Warning signs and symptoms. https://nami.org/About-Mental-Illness/Warning-Signs-and-Symptoms ↵
- National Alliance on Mental Illness. (n.d.). Warning signs and symptoms. https://nami.org/About-Mental-Illness/Warning-Signs-and-Symptoms ↵
- NAMI. (2015, February 2). 10 common warning signs of a mental health condition [Video]. YouTube. All rights reserved. https://youtu.be/zt4sOjWwV3M ↵
- Mental Health First Aid USA. (2019, July 11). Four ways culture impacts mental health. National Council for Mental Wellbeing. https://www.mentalhealthfirstaid.org/2019/07/four-ways-culture-impacts-mental-health/ ↵
- Mental Health First Aid USA. (2019, July 11). Four ways culture impacts mental health. National Council for Mental Wellbeing. https://www.mentalhealthfirstaid.org/2019/07/four-ways-culture-impacts-mental-health/ ↵
- University of Michigan Human Resources. (n.d.). Section 1: What you need to know about mental health problems and substance misuse. https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse ↵
- University of Michigan Human Resources. (n.d.). Section 1: What you need to know about mental health problems and substance misuse. https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse ↵
- National Human Trafficking Training and Technical Assistance Center. (n.d.) The original ACE study. https://nhttac.acf.hhs.gov/soar/eguide/stop/adverse_childhood_experiences ↵
- “ACEs.png” by unknown author for Centers for Disease Control and Prevention is licensed in the Public Domain. Access for free at https://www.cdc.gov/injury/pdfs/priority/ACEs-Strategic-Plan_Final_508.pdf ↵
- U.S. Department of Health & Human Services. (2020, January 24). Strategic goal 3: Strengthen the economic and social well-being of Americans across the lifespan. https://www.hhs.gov/about/strategic-plan/strategic-goal-3/index.html ↵
- University of Michigan Human Resources. (n.d.). Section 1: What you need to know about mental health problems and substance misuse. https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse ↵
- University of Michigan Human Resources. (n.d.). Section 1: What you need to know about mental health problems and substance misuse. https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse ↵
- Kraybill, O. (2019, May 31). Inflammation and mental health symptoms. Psychology Today. https://www.psychologytoday.com/us/blog/expressive-trauma-integration/201905/inflammation-and-mental-health-symptoms ↵
- University of Michigan Human Resources. (n.d.). Section 1: What you need to know about mental health problems and substance misuse. https://hr.umich.edu/benefits-wellness/health-well-being/mhealthy/faculty-staff-well-being/mental-emotional-health/mental-emotional-health-classes-training-events/online-tutorial-supervisors/section-1-what-you-need-know-about-mental-health-problems-substance-misuse ↵
- Alabama Department of Health. (2011, July 29). Understanding the biology of mental illness [Video]. YouTube. All rights reserved. https://youtu.be/LLUoG9Se77w . ↵
- World Health Organization. (2018, March 30). Mental health: Strengthening our response. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response ↵
- mhGAP Intervention Guide - Version 2.0 by World Health Organization is licensed under CC BY-NC-SA 3.0 IGO ↵
- mhGAP Intervention Guide - Version 2.0 by World Health Organization is licensed under CC BY-NC-SA 3.0 IGO ↵
- mhGAP Intervention Guide - Version 2.0 by World Health Organization is licensed under CC BY-NC-SA 3.0 IGO ↵
- Ross, C. A., & Goldner, E. M. (2009). Stigma, negative attitudes and discrimination towards mental illness within the nursing profession: A review of the literature. Journal of Psychiatric and Mental Health Nursing, 16(6), 558-567. https://doi.org/10.1111/j.1365-2850.2009.01399.x ↵
- Centers for Disease Control & Prevention. (2021, July 22). Coping with stress. https://www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/index.html ↵
- mhGAP Intervention Guide - Version 2.0 by World Health Organization is licensed under CC BY-NC-SA 3.0 IGO ↵
A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.
A state of well-being in which an individual realizes their own abilities, copes with the normal stresses of life, works productively, and contributes to their community.
A health condition involving changes in emotion, thinking, or behavior (or a combination of these) associated with emotional distress and problems functioning in social, work, or family activities.
A continuum of mental health, ranging from well-being to emotional problems to mental illness.
The “healthy” range of the mental health continuum where individuals are experiencing a state of good mental and emotional health.
Mental illness that causes disabling functional impairment that substantially interferes with one or more major life activities.
Caring for oneself, performing manual tasks, seeing, hearing, eating, sleeping, walking, standing, lifting, bending, speaking, breathing, learning, reading, concentrating, thinking, communicating, and working.
Disturbances in a person’s thinking, emotional regulation, or behavior that reflects significant dysfunction in psychological, biological, or developmental processes underlying mental functioning.
Psychological and/or physical pain.
A limited ability to engage in activities of daily living.
Behavior that violates social norms or cultural expectations because one's culture determines what is "normal."
Stated and unstated rules of their society.
A generic assessment instrument that provides a standardized method for measuring health and disability across cultures.
A process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential.
Traumatic circumstances experienced during childhood such as abuse, neglect, or growing up in a household with violence, mental illness, substance use, incarceration, or divorce.

