A substance is defined as a psychoactive compound with the potential to cause health and social problems, including substance use disorder. Substances can be divided into four major categories: alcohol, illicit drugs (including nonmedical use of prescription drugs), over-the-counter drugs, and other substances. See examples of substances known to have a significant public health impact in Table 14.2a. Substance use refers to the use of any of the psychoactive substances listed in Table 14.2a.
Table 14.2a Categories and Examples of Substances[1]
| Substance Category | Examples |
|---|---|
| Alcohol | Beer, malt liquor, wine, and distilled spirits |
| Illicit drugs (including prescription drugs used nonmedically) |
|
| Over-the-counter drugs (used nonmedically) | Dextromethorphan, pseudoephedrine, and other cold medications |
| Other substances | Inhalants such as spray paint, gasoline, and cleaning solvents; Delta-8 THC |
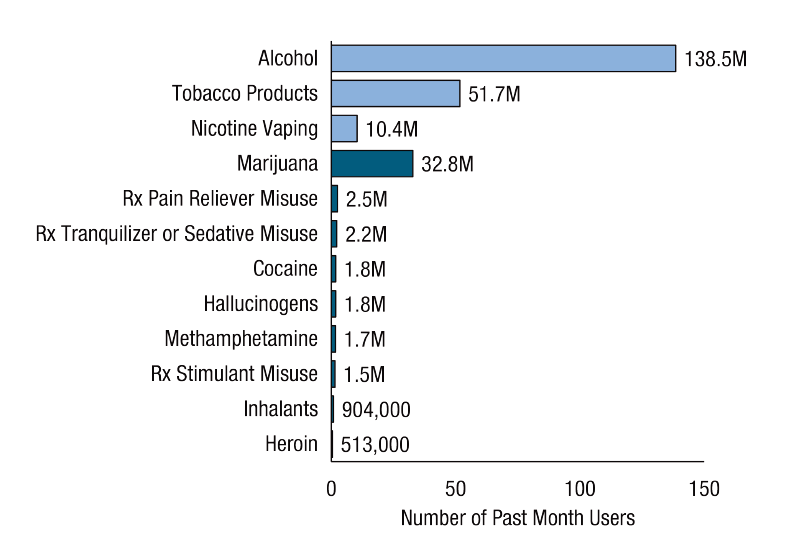
Millions of Americans misuse substances. See Figure 14.1[2]regarding the number of people aged 12 and older who reported using various substances in a one-month period of time.
Controlled Substances
The Controlled Substances Act is a federal law that places all controlled substances (i.e., substances regulated by the U.S. Drug Enforcement Agency) into one of five categories called schedules. This placement is based on the substance’s medical use, its potential for abuse or dependency, and related safety issues. For example, Schedule I drugs have a high potential for abuse and potentially cause severe psychological and/or physical dependence, whereas Schedule V drugs represent the least potential for abuse.[3] Dependence means that when a person suddenly stops using a drug, their body goes through withdrawal, a group of physical and mental symptoms that can range from mild to life-threatening. See examples of controlled substances categorized by schedule in Table 14.2b.
Table 14.2b Examples of Substances by Schedule[4]
Schedule |
Definition |
Examples |
|---|---|---|
| Schedule I | No currently accepted medical use and a high potential for abuse. | Heroin, LSD, MDMA (Ecstasy), and cannabis (marijuana) |
| Schedule II | High potential for abuse, with use potentially leading to severe psychological or physical dependence. These drugs are also considered dangerous. | Hydrocodone, cocaine, methamphetamine, methadone, hydromorphone, meperidine, oxycodone, fentanyl, amphetamine/dextroamphetamine salts (Adderall), methylphenidate (Ritalin), and phencyclidine (PCP) |
| Schedule III | Moderate to low potential for physical and psychological dependence. Abuse potential is less than Schedule I and Schedule II drugs but more than Schedule IV. | Acetaminophen with codeine, ketamine, anabolic steroids, and testosterone |
| Schedule IV | Low potential for abuse and low risk of dependence. | Alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), zolpidem (Ambien), and tramadol (Ultram) |
| Schedule V | Lower potential for abuse than Schedule IV and consist of preparations containing limited quantities of certain narcotics. Generally used for antidiarrheal, antitussive, and analgesic purposes. | Cough medications with codeine, diphenoxylate/atropine (Lomotil), and pregabalin (Lyrica) |
Substance Misuse
Substance misuse is defined as the use of alcohol or drugs in a manner, situation, amount, or frequency that could cause harm to the user or to those around them.[5] Misuse can be of low severity and temporary, but it can increase the risk for serious and costly consequences such as motor vehicle crashes; overdose death; suicide; various types of cancer; heart, liver, and pancreatic diseases; HIV/AIDS; and unintended pregnancies. Substance use during pregnancy can cause complications for the baby such as fetal alcohol spectrum disorders (FASDs) or neonatal abstinence syndrome (NAS). Substance misuse is also associated with intimate partner violence, child abuse, and neglect.[6] Substance abuse, an older diagnostic term, referred to unsafe substance use (e.g., drunk or drugged driving), use that caused legal problems, or use that continued despite failure to meet work and family responsibilities. However, the term “substance abuse” is now avoided by professionals because it does not accurately account for the neurobiological knowledge we now have about addictive disorders. Instead, the term “substance use disorder” is preferred and is further discussed in the “Substance Use Disorder” subsection of this chapter.[7]
Intoxication and Overdose
Intoxication refers to a disturbance in behavior or mental function during or after the consumption of a substance. Overdose is the biological response of the human body when too much of a substance is ingested. Signs of intoxication and overdose for categories of psychoactive substances are described in the following subsections.
Anyone can call a regional poison control center at 1-800-222-1222 for consultation regarding toxic ingestion of substances and overdoses. Poison control centers are available at all times, every day of the year. Some hospitals also have toxicologists available for bedside consultation for overdoses.[8]
Alcohol Use and Intoxication
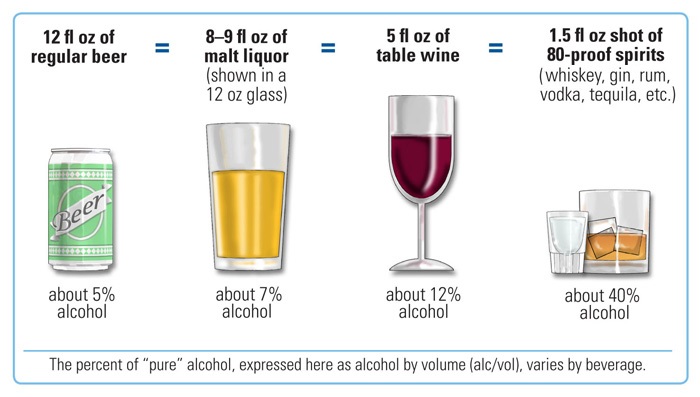
Based on the 2015-2020 Dietary Guidelines for Americans, a standard drink is defined as 14 grams (0.6 ounces) of pure alcohol. Examples of a standard drink are one 12-ounce beer, 8 – 9 ounces of malt liquor, 5 ounces of wine, or 1.5 ounces of distilled spirits. See Figure 14.2[9] for images of standard drinks.
The 2020 National Survey on Drug Use and Health reports that 50 percent (139.7 million) of Americans aged 12 or older use alcohol, 22.2 percent are binge drinkers, and 6.4 percent are heavy alcohol users.[10] Heavy drinking is defined as a female consuming 8 or more drinks per week or a male consuming 15 or more standard drinks per week, or either gender binge drinking on 5 or more days in the past 30 days. Binge drinking is defined as consuming several standard drinks on one occasion in the past 30 days; for men, this refers to drinking five or more standard alcoholic drinks on one occasion, and for women this refers to drinking four or more standard drinks on one occasion.[11] Alcohol intoxication refers to problematic behavioral or psychological changes (e.g., inappropriate sexual or aggressive behavior, mood lability, or impaired judgment) that develop during or shortly thereafter alcohol ingestion. Signs and symptoms of alcohol intoxication are as follows[12]:
- Slurred speech
- Incoordination
- Unsteady gait
- Nystagmus
- Impairment in attention or memory
Alcohol Overdose
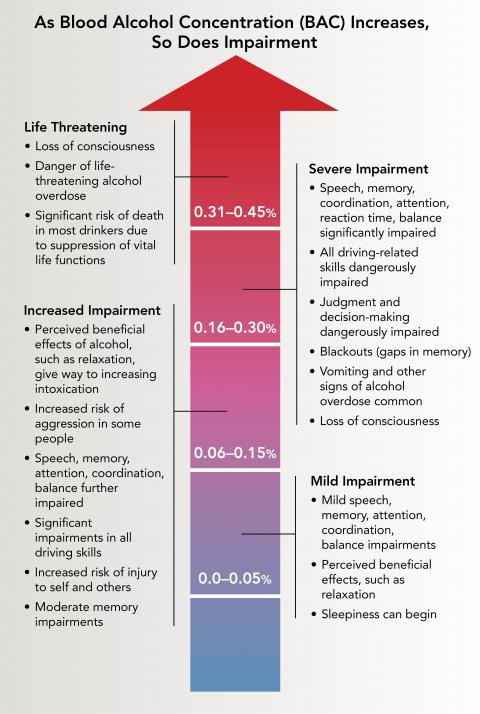
An alcohol overdose occurs when there is so much alcohol in the bloodstream that areas of the brain controlling autonomic nervous system functions (e.g., breathing, heart rate, and temperature control) begin to shut down. Signs of alcohol overdose include mental confusion, difficulty remaining conscious, vomiting, seizures, trouble breathing, slow heart rate, clammy skin, dulled gag reflex, and extremely low body temperature. Alcohol intoxication while also taking opioids or sedative-hypnotics (such as benzodiazepines or sleep medications) increases the risk of an overdose. Alcohol overdose can cause permanent brain damage or death.[13] Anyone who consumes too much alcohol too quickly is in danger of an alcohol overdose, especially for individuals who engage in binge drinking. As blood alcohol concentration (BAC) increases, so does the risk of harm. When BAC reaches high levels, blackouts (gaps in memory), loss of consciousness (passing out), and death can occur. BAC can continue to rise even when a person stops drinking or is unconscious because alcohol in the stomach and intestine continues to enter the bloodstream and circulate throughout the body. See Figure 14.3[14] for the impairments related to rising BAC.
It is dangerous to assume that a person who drank an excessive amount of alcohol will “sleep it off.” One potential danger of alcohol overdose is choking on one’s vomit and dying from lack of oxygen because high levels of alcohol intake hinder the gag reflex, resulting in the inability to protect the airway. Asphyxiation can occur due to an obstructed airway or from aspiration of gastric contents into the lungs. For this reason, do not leave a person alone who has passed out due to alcohol misuse. Keep them in a partially upright position or roll them onto one side with an ear toward the ground to prevent choking if they begin vomiting.[15] Critical signs and symptoms of an alcohol overdose include the following[16]:
- Mental confusion or stupor
- Difficulty remaining conscious or inability to wake up
- Vomiting
- Seizures
- Slow respiratory rate (fewer than 8 breaths per minute)
- Irregular breathing (10 seconds or more between breaths)
- Slow heart rate
- Clammy skin
- No gag reflex
- Extremely low body temperature
- Bluish skin color or paleness
If you suspect someone has overdosed on alcohol, seek emergency assistance or call 911. While waiting for help to arrive, be prepared to provide information to the responders, such as the type and amount of alcohol the person drank and any other drugs they ingested, current medications, allergies to medications, and any existing health conditions.[17]
Medical Treatment of Acute Alcohol Intoxication
Acute alcohol intoxication can cause hypotension and tachycardia as a result of peripheral vasodilation or fluid loss. Treatment begins with the evaluation of the client’s blood alcohol level (BAC). It is important to know if other drugs like opioids, benzodiazepines, or street drugs have been ingested because this increases the risk of overdose, and other treatments (such as naloxone) may be required. For clients with moderate to severe intoxication, routine lab work includes serum glucose and electrolytes to assess for hypoglycemia, hypokalemia, hypomagnesemia, hypocalcemia, hypophosphatemia, and hyperlactatemia. If hypoglycemia is present, a dextrose intravenous infusion is provided.[18] Severely intoxicated clients may receive intravenous thiamine, along with dextrose, to prevent Wernicke’s encephalopathy. Wernicke’s encephalopathy is an acute, life-threatening neurological condition characterized by nystagmus, ataxia, and confusion caused by thiamine (B1) deficiency associated with alcohol use disorder. Thiamine is required for cerebral energy utilization.[19] If untreated, Wernicke’s encephalopathy can progress to Korsakoff’s syndrome, a chronic, irreversible memory disorder resulting from thiamine deficiency.[20]
Some clients with acute alcohol intoxication can become agitated, violent, and uncooperative. Chemical sedation with administration of benzodiazepines may be required to prevent the client from harming themselves or others. However, benzodiazepines must be used with caution because they worsen the respiratory depression caused by alcohol.[21] Approximately one percent of clients with acute alcohol intoxication require critical care. Risk factors for admission to the intensive care unit (ICU) include abnormal vital signs (hypotension, tachycardia, fever, or hypothermia), hypoxia, hypoglycemia, and the need for parenteral sedation. If the client has inadequate respirations or airway maintenance, intubation and mechanical ventilation are required. Activated charcoal and gastric lavage are generally not helpful because of the rapid rate of absorption of alcohol from the gastrointestinal tract. Some acutely intoxicated clients experience head traumas due to severe intoxication from injuries sustained while intoxicated. If the client’s mental status does not improve as their BAC level decreases, a CT scan of the head may be obtained.[22]
Opioid Use and Intoxication
In 2020, 9.5 million (3.4%) of Americans aged 12 and older reported using opioids in the past year. Among this population, 9.3 million people misused prescription pain relievers, and 902,000 people used heroin.[23] Opioids are substances that act on opioid receptors in the central nervous system. Medically, they are used for relief of moderate to severe pain and anesthesia. When misused, opioids cause a person to feel relaxed and euphoric (i.e., experience an intense feeling of happiness). Opioid prescription medications include Schedule II medications such as morphine, oxycodone, hydrocodone, fentanyl, and hydromorphone. Heroin, an illegal street drug, is also an opioid, but it is classified as a Schedule I drug.[24] Injected opioid misuse is a risk factor for contracting HIV, hepatitis B, hepatitis C, and bacterial endocarditis. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016.[25] Opioid intoxication causes problematic behavioral or psychological changes such as initial euphoria followed by apathy, dysphoria, psychomotor retardation or agitation, and impaired judgment. These are some signs of opioid intoxication[26]:
- Pupillary constriction (or dilation from severe overdose)
- Drowsiness or coma
- Slurred speech
- Impairment in attention or memory
The typical signs of opioid overdose are referred to as the opioid overdose triad and include pinpoint pupils, respiratory depression, and decreased level of consciousness.[27]
Increasing Rates of Opioid Overdose Deaths
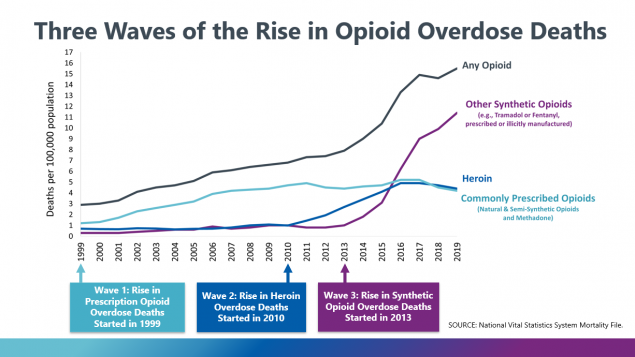
From 1999 to 2019, nearly 500,000 people died from an overdose involving prescription or illicit opioids. This rise in opioid overdose deaths can be outlined in three distinct waves. See Figure 14.4[28] for an illustration of these three waves of opioid overdose. The first wave of overdose deaths began with the increased prescription rate of opioids in the 1990s. The second wave began in 2010 with rapid increases in overdose deaths involving heroin. The third wave began in 2013 with significant increases in overdose deaths involving synthetic opioids, particularly illicitly manufactured fentanyl.[29]
There are two types of fentanyl: pharmaceutical fentanyl prescribed for severe pain, and illicitly manufactured fentanyl. Most recent cases of fentanyl-related overdose are associated with illicitly manufactured fentanyl that is added to other street drugs that make them more powerful, more addictive, and more dangerous.[30]
Carfentanil is a new factor in opioid overdose rates. Carfentanil is synthetic opioid used to tranquilize large mammals like elephants. It is approximately 10,000 times more potent than morphine and 100 times more potent than fentanyl. A miniscule amount of powder containing two milligrams of carfentanil can be lethal. Carfentanil can be accidentally absorbed through the skin or inhaled by unsuspecting parties. If carfentanil or another fentanyl-related drug is suspected to be present on an individual, first responders and health care professionals must carefully follow safety protocols to avoid accidental lethal exposure.[31]
Read a U.S. Department of Justice Officer Safety Alert PDF: Carfentanil: A Dangerous New Factor in the U.S. Opioid Crisis.
Treating Opioid Overdose
Naloxone reverses the effects of an opioid overdose. A single-step nasal spray delivery of naloxone is the easiest and most successful route of administration for members of the community and first responders. Naloxone intramuscular injection is also available.[32]
Five basic steps are recommended for nurses, first responders, health professionals, and other bystanders to rapidly recognize and treat opioid overdose to prevent death.[33]
- Recognize Signs of Opioid Overdose
- Signs of opioid overdose include the following:
- Unconsciousness or inability to awaken
- Pinpoint pupils
- Slow, shallow breathing; breathing difficulty manifested by choking sounds or a gurgling/snoring noise from a person who cannot be awakened; or respiratory arrest
- Fingernails or lips turning blue or purple
- If an opioid overdose is suspected, try to stimulate the person by calling their name or vigorously grinding one’s knuckles into their sternum.
- Signs of opioid overdose include the following:
- Obtain Emergency Assistance: If the person does not respond, call 911 or obtain emergency assistance.
- Provide Rescue Breathing, Chest Compressions, and Oxygen As Needed[34]
- Provide rescue breathing if the person is not breathing on their own. A barrier device is recommended to reduce the risk of disease transmission. Rescue breathing for adults involves the following steps:
- Be sure the person’s airway is clear.
- Place one hand on the person’s chin, tilt the head back, and pinch the nose closed.
- Place your mouth over the person’s mouth to make a seal and give two slow breaths.
- Watch for the person’s chest (but not the stomach) to rise.
- Follow up with one breath every five seconds.
- If the individual becomes pulseless, provide cardiopulmonary resuscitation (CPR).
- Administer oxygen as needed.
- Provide rescue breathing if the person is not breathing on their own. A barrier device is recommended to reduce the risk of disease transmission. Rescue breathing for adults involves the following steps:
- Administer the First Dose of Naloxone[35]
- Naloxone should be administered to anyone suspected of an opioid overdose.
- Research has shown that women, older adults, and those without obvious signs of opioid use disorder are undertreated with naloxone and, as a result, have a higher death rate. Therefore, naloxone should be considered for women and the elderly who are found unresponsive.
- Naloxone can be used in life-threatening opioid overdose circumstances in pregnant women.
- Naloxone can be given intranasally, intramuscularly, subcutaneously, or intravenously. The nasal spray is a prefilled device that requires no assembly and delivers a single dose into one nostril. An auto-injector is injected into the outer thigh to deliver naloxone intramuscularly or subcutaneously.
- All naloxone products are effective in reversing opioid overdose, including fentanyl-involved opioid overdoses, although overdoses involving potent or large quantities of opioids may require additional doses of naloxone.
- Withdrawal triggered by naloxone can feel unpleasant; some people may awaken confused, agitated, or aggressive. Provide safety, reassurance, and explain what is happening.
- Administer a Second Dose of Naloxone If the Person Does Not Respond[36]:
- If the person overdosing does not respond within 2 to 3 minutes after administering a dose of naloxone, administer a second dose of naloxone.
- People who have taken long-acting or potent opioids (like fentanyl) may require additional intravenous bolus doses or an infusion of naloxone.
- The duration of effect of naloxone depends on dose, route of administration, and overdose symptoms. It is shorter than the effects of some opioids, so a second dose may be required.
- Monitor the Person’s Response[37]:
- Most people respond to naloxone by returning to spontaneous breathing within 2 to 3 minutes. Continue resuscitation while waiting for the naloxone to take effect.
- The goal of naloxone therapy is to restore adequate spontaneous breathing but not necessarily achieve complete arousal.
- The individual should be monitored for recurrence of signs and symptoms of opioid toxicity for at least four hours from the last dose of naloxone. People who have overdosed on long-acting opioids like fentanyl require prolonged monitoring.
- Because naloxone has a relatively short duration of effect, overdose symptoms may return. Therefore, it is essential to get the person to an emergency department or other source of medical care as quickly as possible, even if the person revives after the initial dose of naloxone and seems to feel better.
Preventing Opioid Overdose
Nearly 85% of overdose deaths involve illicitly manufactured fentanyl, heroin, cocaine, or methamphetamine. Potential opportunities to link people to care or to implement life-saving actions have been identified for more than 3 in 5 people who died from drug overdose. Circumstances that represent a potential touchpoint for linkage to care are as follows[38]:
- Bystander present: Nearly 40% of opioid and stimulant overdose deaths occurred while a bystander was present.
- Recent release from an institution: Among the people who died from overdoses involving opioids, about 10% had recently been released from an institution (such as jail/prison, inpatient rehabilitation facilities, or psychiatric hospitals). Risk increased for this population because they were unaware of decreased tolerance to the drug due to abstinence from it while in the institution.
- Previous overdose: Among the people who died from overdoses involving opioids, about 10% had a previous overdose.
- Mental health diagnosis: Among all the people who died of a drug overdose, 25% had a documented mental health diagnosis.
- Substance use disorder treatment: Among the people who died from opioid overdose, nearly 20% had previously been treated for substance use disorder.
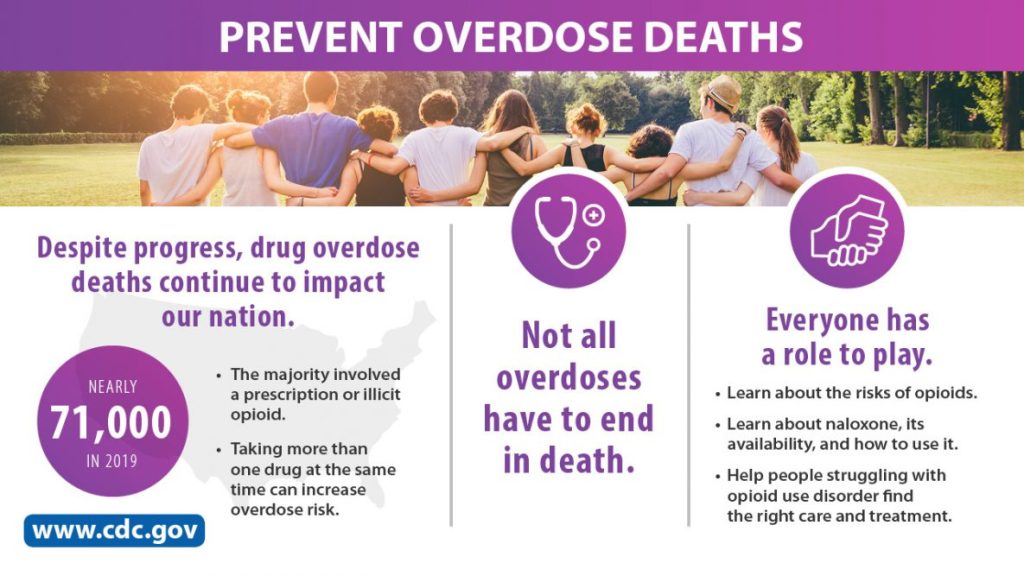
Opioid overdoses can be prevented by helping individuals struggling with opioid use disorder find the right treatment and recovery services, as well as providing public education about administering naloxone. See Figure 14.5.[39] for an image related to these strategies.[40] Read more about treatment and recovery in the “Treatment of Substance Use Disorders” section.
Cannabis (Marijuana) Use and Intoxication
Approximately 48.2 million (17.5 percent) of Americans aged 12 or older used cannabis (marijuana) in the past year, and 14.2 million people (5.1%) have a cannabis use disorder.[41] Changes in marijuana policies across states have legalized marijuana for recreational and/or medicinal uses (e.g., pain control, increased appetite for individuals undergoing chemotherapy, etc.). Although many states now permit dispensing marijuana for medicinal purposes, the U.S. Food and Drug Administration has not approved “medical marijuana.” Therefore, it is important for nurses to educate people about both the adverse health effects and the potential therapeutic benefits linked to marijuana.[42]
The main psychoactive chemical in marijuana is Delta-9-tetrahydrocannabinol (THC). THC alters the functioning of the hippocampus and other areas of the brain that enable a person to form new memories and shift their attentional focus. As a result, marijuana causes impaired thinking and interferes with a person’s ability to learn and perform complicated tasks. THC also disrupts functioning of the cerebellum and basal ganglia that regulate balance, posture, coordination, and reaction time. For this reason, people who have used marijuana may not drive safely and may have problems playing sports or engaging in other physical activities.[43]
When marijuana is smoked, THC and other chemicals pass from the lungs into the bloodstream and are rapidly carried to the brain. The person begins to experience effects such as euphoria and sense of relaxation almost immediately. Other common effects include heightened sensory perception (e.g., brighter colors), laughter, altered perception of time, and increased appetite. Other people experience anxiety, fear, distrust, or panic, especially if they take too much, the marijuana has high potency, or the person is inexperienced in using cannabis. People who have taken large or highly potent doses of marijuana may experience acute psychosis, including hallucinations, delusions, and a loss of the sense of personal identity.[44]
If marijuana is consumed in foods or beverages, the effects are delayed for 30 minutes to 1 hour, because the drug must first pass through the digestive system. Eating or drinking marijuana delivers significantly less THC into the bloodstream. Because of the delayed effects, people may inadvertently consume more THC than they intend to.[45] Although detectable amounts of THC may remain in the body for days or even weeks after use, the noticeable effects of smoked marijuana generally last from 1 to 3 hours, and marijuana consumed in food or drink may last for many hours.[46]
Delta-8 THC products are manufactured from hemp-derived cannabidiol (CBD) and have psychoactive and intoxicating effects similar to Delta-9 THC. Some Delta-8 THC products are labeled as “hemp products,” which can mislead consumers who associate “hemp” with being non-psychoactive. Delta-8 THC is available for purchase online and in stores but has not been approved by the U.S. Food and Drug Administration for safe use in any context. It should be kept out of reach of children and pets. Some manufacturers use unsafe chemicals to make Delta-8 THC through a chemical synthesis process that can contaminate the end product. As a result, there has been a recent increase in reports of adverse events with 8% of cases requiring admission to a critical care unit.[47]
THC affects brain systems that are still maturing through young adulthood, so regular use by teens may have negative and long-lasting effects on their cognitive development. Marijuana smoking is associated with large airway inflammation, increased airway resistance, lung hyperinflation, and chronic bronchitis. Vaping products that contain THC are associated with serious lung disease and death. Also, contrary to popular belief, marijuana can be addictive. THC stimulates neurons in the brain’s reward system to release higher levels of dopamine and encourages the brain to repeat the rewarding behavior.[48]
The potential medicinal properties of marijuana and THC have been the subject of research and heated debate for decades. THC itself has proven medical benefits in particular formulations. For example, the U.S. Food and Drug Administration (FDA) has approved the use of THC-based oral medications dronabinol (Marinol) and nabilone (Cesamet) for the treatment of nausea in clients undergoing cancer chemotherapy and to stimulate appetite in clients with wasting syndrome due to AIDS.[49] Marijuana is also used by individuals with certain illness such as multiple sclerosis for the management of spasticity, tics, convulsions, and dyskinesia.[50]
Cannabis intoxication is defined as problematic behavior or psychological changes (e.g., impaired motor coordination, euphoria, anxiety, sensation of slowed time, impaired judgment, social withdrawal) that developed during or shortly after cannabis use. Signs and symptoms of cannabis intoxication include the following[51]:
- Enlarged conjunctival vessels
- Increased appetite
- Dry mouth
- Tachycardia
According to the CDC, a fatal overdose caused solely by marijuana is unlikely. However, effects from marijuana can lead to unintentional injury, such as a motor vehicle crash, fall, or poisoning. Overconsumption of marijuana can occur when using marijuana-infused products like edibles and beverages because it can take up to two hours to feel the effects from the drug.[52] Additionally, marijuana purchased as a street drug may be laced with other substances like synthetic fentanyl that can cause overdose.
Sedative, Hypnotic, and Anxiolytic Use and Intoxication
Examples of medications in the sedative, hypnotic, or anxiolytic class include benzodiazepines, such as alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), chlordiazepoxide (Librium), and clonazepam (Klonopin). An example of a hypnotic is zolpidem (Ambien). Although these are prescription medications, they are commonly misused.
Chronic use of benzodiazepines causes changes in the gamma-aminobutyric acid (GABA) receptor, resulting in decreased GABA activity and the development of tolerance. When benzodiazepines are no longer present, or suddenly present at lower doses, withdrawal occurs.
Sedatives, hypnotics, and anxiolytic intoxication cause behavioral or psychological changes similar to alcohol intoxication, such as inappropriate sexual or aggressive behavior, mood lability, and impaired judgment. Symptoms of intoxication are as follows[53]:
- Slurred speech
- Incoordination
- Unsteady gait
- Nystagmus
- Impaired attention and memory
- Stupor or coma
Benzodiazepines are not detected by standard urine tests for drugs of abuse. However, specific benzodiazepine urine tests identify the metabolites of some benzodiazepines.[54]
Overdose
Benzodiazepines cause CNS depression and are commonly involved in drug overdose. They are often co-ingested with other drugs, such as alcohol or opioids that cause stupor, coma, and respiratory depression. When treating benzodiazepine overdose, end tidal CO2 (i.e., capnography) is used to monitor clients at risk for hypoventilation. Endotracheal intubation and mechanical ventilation may be required.[55],[56] Flumazenil is an antidote to reverse benzodiazepine-induced sedation following general anesthesia and procedural sedation. However, it is used cautiously for benzodiazepine overdose because it is associated with withdrawal seizures in individuals who have developed a tolerance to benzodiazepines.
Hallucinogen Use and Intoxication
In 2020, 7.1 million (2.6 percent) people in America aged 12 or older used hallucinogens.[57] Hallucinogens are a diverse group of drugs that alter a person’s awareness of their surroundings, as well as their own thoughts and feelings. They are commonly split into two categories: classic hallucinogens (such as LSD and peyote) and dissociative drugs (such as phencyclidine and ketamine). Dextromethorphan is an over-the-counter cough suppressant misused for its hallucinogenic and dissociative properties at high doses.
Hallucinogens cause hallucinations (sensations and images that seem real though they are not), and dissociative drugs can cause users to feel out of control or disconnected from their bodies and environments. Historically, some cultures have used hallucinogens like peyote as a part of religious or healing rituals.[58] Users of hallucinogens and dissociative drugs have increased risk for serious harm because of altered perceptions and moods. As a result, users might do things they would never do when not under the influence of a hallucinogen, like jump off a roof or act on suicidal thoughts.[59]
Phencyclidine (PCP) is an example of a hallucinogen. It is an illegal street drug that usually comes as a white powder that can be inhaled through the nose, injected into a vein, smoked, or swallowed.[60] PCP intoxication causes problematic behavioral changes (e.g., belligerence, assaultiveness, impulsiveness, unpredictability, psychomotor agitation, impaired judgment) that occur during or shortly thereafter use.[61] Because of these symptoms, PCP is associated with violent and aggressive behavior including self-injury and violent criminal offenses (such as assaults, intimate partner violence, and homicide).[62] Within one hour of ingestion, two or more of the following signs or symptoms occur[63]:
- Vertical or horizontal nystagmus (an involuntary eye movement that causes the eye to rapidly move up and down or from side to side)
- Hypertension
- Tachycardia
- Numbness or diminished responsiveness to pain
- Ataxia (impaired balance or coordination)
- Slurred speech
- Muscle rigidity
- Seizures or coma
- Hyperacusis (sensitivity to noise)
Physical restraints may be necessary to control clients experiencing psychomotor agitation, followed by chemical sedation with intravenous benzodiazepines.[64]
Overdose
Overdose can occur with some dissociative drugs like PCP. High doses of PCP can cause seizures, coma, and death, especially if taken with depressants such as alcohol or benzodiazepines.[65]
Dextromethorphan is an over-the-counter medication that is misused due to its hallucinogenic effects and can cause overdose. Nonmedical use of dextromethorphan results in approximately 6,000 emergency department visits annually in the United States, often with co-ingestion of alcohol. Signs of toxic doses include neurobehavioral changes (e.g., hallucinations, inappropriate laughing, psychosis with dissociative features, agitation, and coma); tachycardia; dilated pupils; diaphoresis; and a “zombie-like” ataxic gait. Because acetaminophen is commonly present in cough and cold medications, toxic doses can cause severe delayed hepatotoxicity, hepatic failure, and death; serum acetaminophen levels should be obtained in all clients presenting with toxic levels of dextromethorphan.[66]
Stimulant Use and Intoxication
Stimulants include amphetamine-type substances, cocaine, and crack. Stimulants cause the release of dopamine in the brain and are highly addictive because the flood of dopamine in the brain’s reward circuit strongly reinforces drug-taking behaviors. With continued drug use, the reward circuit adapts and becomes less sensitive to the drug. As a result, people take stronger and more frequent doses in an attempt to feel the same high and to obtain relief from withdrawal symptoms. Because the high from stimulants starts and fades quickly, people often take repeated doses in a form of binging, often giving up food and sleep while continuing to take the drug every few hours for several days. Both the use and withdrawal from amphetamines can cause psychosis with symptoms of hallucinations and paranoia.[67]
Approximately 2 million Americans used methamphetamine in the past year. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine quadrupled from 2011 to 2017.[68] Methamphetamine comes in many forms and can be ingested by smoking, swallowing a pill, snorting, or injecting the powder that has been dissolved in water or alcohol. Methamphetamine can be easily made in small clandestine laboratories with relatively inexpensive over-the-counter ingredients such as pseudoephedrine, a common ingredient in cold medications. (To curb this illegal production, federal law requires pharmacies take steps to limit sales and obtain photo identification from purchasers.) Methamphetamine production also involves a number of other very dangerous chemicals. Toxic effects from these chemicals can remain in the environment long after the lab has been shut down, causing a wide range of health problems for people living in the area. These chemicals can also result in deadly lab explosions and house fires.[69]
Long-term use of methamphetamine has many negative consequences, including extreme weight loss, severe dental problems, intense itching leading to skin sores from scratching, involuntary movements (dyskinesia), anxiety, memory loss, and violent behavior.[70]
Cocaine is another powerfully addictive stimulant drug made from the leaves of the coca plant native to South America. It is estimated that 5.5 million people aged 12 or older have used cocaine, including about 778,000 users of crack.[71] Users may snort cocaine powder through the nose, rub it into their gums, or dissolve the powder and inject it into the bloodstream. Cocaine that has been processed to make a rock crystal is called “crack.” The crystal is heated (making crackling sounds) to produce vapors that are inhaled into the lungs.[72],[73] In the short-term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long-term, severe medical complications of cocaine use include heart attacks and seizures.[74]
Stimulant intoxication causes problematic behavioral or psychological changes such as euphoria or blunted affect; changes in sociability; hypervigilance; interpersonal sensitivity; anxiety, tension, or anger; and impaired judgment. These are some symptoms of stimulant intoxication[75],[76]:
- Tachycardia
- Hypertension
- Pupillary dilation
- Elevated or decreased blood pressure
- Perspiration or chills
- Nausea or vomiting
- Weight loss
- Psychomotor agitation or retardation
- Muscular weakness
- Respiratory depression
- Chest pain or cardiac dysrhythmias
- Confusion, seizures, or coma
- Psychosis/hallucinations
- Dyskinesia (involuntary, erratic, writhing movements of the face, arms, legs, or trunk)
- Dystonia (involuntary muscle contractions that result in slow repetitive movements)
It is important for nurses to be aware that individuals with acute methamphetamine intoxication may, without provocation, develop severe agitation with extreme violence and place themselves, family members, medical staff, and other clients at risk of major injury. Control of agitation and hyperthermia (body temperature over 41 degrees Celsius) receive top priority for treatment with the following interventions[77]:
- Intravenous benzodiazepines are administered immediately for chemical sedation of severely agitated individuals.
- Physical restraints should be avoided because clients who physically struggle against restraints undergo isometric muscle contractions that are associated with lactic acidosis, hyperthermia, sudden cardiac collapse, and death.
- Airway management with endotracheal intubation and mechanical ventilation may be required.
- Aggressive cooling is achieved through sedation, fluid resuscitation, external cooling blankets, or evaporative cooling techniques. Antipyretics are not used because the increased body temperature is caused by muscular activity, not an alteration in the hypothalamic temperature set point.
Read DrugFacts by the National Institute on Drug Abuse for more information about substances, intoxication, and overdose.
Inhalant Use and Intoxication
In 2020, 2.4 million (0.9 percent) of people aged 12 or older in America used inhalants. Unlike other illicit drugs, the percentage of inhalant use was highest among adolescents aged 12 to 17.[78] Inhalants are various products easily bought or found in the home, such as spray paints, markers, glue, gasoline, and cleaning fluids. People who use inhalants breathe in the fumes through their nose or mouth, usually by sniffing, snorting, bagging, or huffing. Although the high that inhalants produce usually lasts just a few minutes, people often try to make it last by continuing to inhale again and again over several hours.[79]
Prescription medications can also be misused as inhalants. For example, amyl nitrate is a prescription medication administered via inhalation to relieve chest pain. However, it is misused by individuals to cause a high. It is referred to by the street drug of “poppers.”
Inhalant intoxication causes problematic behavioral or psychological changes such as belligerence, assaultiveness, apathy, and impaired judgment. Inhalant intoxication includes these symptoms[80]:
- Dizziness
- Nystagmus
- Incoordination
- Slurred speech
- Unsteady gait
- Lethargy
- Depressed reflexes
- Psychomotor retardation
- Tremor
- Generalized muscle weakness
- Blurred or double vision
- Stupor or coma
- Euphoria
Long-term effects of inhalant use may include liver and kidney damage, hearing loss, bone marrow damage, loss of coordination and limb spasms (from nerve damage), delayed behavioral development (from brain problems), and brain damage (from cut-off oxygen flow to the brain).[81]
Acute intoxication with inhalants can cause life-threatening seizures and coma. Many solvents and aerosol sprays are highly concentrated with many other active ingredients; sniffing these products can cause the heart to stop within minutes. This condition, known as sudden sniffing death, can happen to otherwise healthy young people the first time they use an inhalant.[82] Treatment consists of maintaining cardiorespiratory function with 100 percent oxygen administration by rebreather mask and implementation of Pediatric Advanced Life Support (PALS) protocols that may require endotracheal intubation and mechanical ventilation.[83]
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- This image is a derivative of “Past Month General Substance Use and Nicotine Vaping: Among People Aged 12 and Older; 2020” table by Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Used under Fair Use. Retrieved from https://www.samhsa.gov/data/report/2020-nsduh-annual-national-report ↵
- United States Drug Enforcement Administration. (n.d.). The Controlled Substance Act. U.S. Department of Justice. https://www.dea.gov/drug-information/csa ↵
- United States Drug Enforcement Administration. (n.d.). The Controlled Substance Act. U.S. Department of Justice. https://www.dea.gov/drug-information/csa ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Substance Abuse and Mental Health Services Administration, & Office of the Surgeon General. (2016). Facing addiction in America: The surgeon general's report on alcohol, drugs, and health. United States Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK424857/ ↵
- Rosenbaum, C., & Boyer, E. (2021, January 20). Dextromethorphan abuse and poisoning: Clinical features and diagnosis. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- “NIH_standard_drink_comparison.jpg” by National Institutes of Health is in the Public Domain ↵
- National Survey on Drug Use and Health. https://nsduhweb.rti.org/respweb/homepage.cfm ↵
- National Survey on Drug Use and Health. https://nsduhweb.rti.org/respweb/homepage.cfm ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5 ↵
- National Institute on Alcohol Abuse and Alcoholism, & National Institutes of Health. (2021, May). Understanding the dangers of alcohol overdose. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-dangers-of-alcohol-overdose ↵
- “NIAAA_BAC_Increases_Graphic.jpg” by The National Institute on Alcohol Abuse and Alcoholism is in the Public Domain. Access for free at https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-dangers-of-alcohol-overdose ↵
- National Institute on Alcohol Abuse and Alcoholism, & National Institutes of Health. (2021, May). Understanding the dangers of alcohol overdose. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-dangers-of-alcohol-overdose ↵
- National Institute on Alcohol Abuse and Alcoholism, & National Institutes of Health. (2021, May). Understanding the dangers of alcohol overdose. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-dangers-of-alcohol-overdose ↵
- National Institute on Alcohol Abuse and Alcoholism, & National Institutes of Health. (2021, May). Understanding the dangers of alcohol overdose. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-dangers-of-alcohol-overdose ↵
- Cowan, E., & Su, M. K. (2020, March 19). Ethanol intoxication in adults. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- This work is a derivative of StatPearls by Vasan and Kumar and is licensed under CC BY 4.0 ↵
- National Institute of Neurological Disorders and Stroke. (n.d.). Wernicke-Korsakoff syndrome. https://www.ninds.nih.gov/health-information/disorders/wernicke-korsakoff-syndrome#:~:text=Korsakoff%20syndrome%20(also%20called%20Korsakoff's,the%20brain%20involved%20with%20memory. ↵
- Cowan, E., & Su, M. K. (2020, March 19). Ethanol intoxication in adults. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- Cowan, E., & Su, M. K. (2020, March 19). Ethanol intoxication in adults. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- National Survey on Drug Use and Health. https://nsduhweb.rti.org/respweb/homepage.cfm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2022. Opioid intoxication; [updated 2022, February 18]. https://medlineplus.gov/ency/article/000948.htm ↵
- Substance Abuse and Mental Health Services Administration. (2022, March 2). Alcohol, tobacco, and other drugs. U.S. Department of Health & Human Services. https://www.samhsa.gov/find-help/atod ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- StatPearls by Schiller, Goyal, & Mechanic is licensed under CC BY 4.0 ↵
- “3-waves-2019-medium.PNG” by The Centers for Disease Control and Prevention is in the Public Domain. Access for free at https://www.cdc.gov/drugoverdose/epidemic/index.html ↵
- Centers for Disease Control and Prevention. (2021, March 17). Understanding the epidemic. U.S. Department of Health & Human Services. https://www.cdc.gov/drugoverdose/epidemic/index.html ↵
- Centers for Disease Control and Prevention. (n.d.). The facts about fentanyl [Handout]. https://www.cdc.gov/stopoverdose/fentanyl/pdf/fentanyl_fact_sheet_508c.pdf ↵
- Drug Enforcement Administration. (n.d.). Officer safety alert. U.S. Department of Justice. https://www.justice.gov/usao-edky/file/898991/download ↵
- Eggleston, W., Podolak, C., Sullivan, R.W., Pacelli, L., Keenan, M., and Wojcik, S. (2018). A randomized usability assessment of simulated naloxone administration by community members. Addiction, 113(12):2300-2304. https://doi.org/10.1111/add.14416 ↵
- Substance Abuse and Mental Health Services Administration. (2018). SAMHSA opioid overdose prevention toolkit: Five essential steps for first responders [Manual]. U.S. Department of Health & Human Services. https://store.samhsa.gov/sites/default/files/d7/priv/five-essential-steps-for-first-responders.pdf ↵
- Substance Abuse and Mental Health Services Administration. (2018). SAMHSA opioid overdose prevention toolkit: Five essential steps for first responders [Manual]. U.S. Department of Health & Human Services. https://store.samhsa.gov/sites/default/files/d7/priv/five-essential-steps-for-first-responders.pdf ↵
- Substance Abuse and Mental Health Services Administration. (2018). SAMHSA opioid overdose prevention toolkit: Five essential steps for first responders [Manual]. U.S. Department of Health & Human Services. https://store.samhsa.gov/sites/default/files/d7/priv/five-essential-steps-for-first-responders.pdf ↵
- Substance Abuse and Mental Health Services Administration. (2018). SAMHSA opioid overdose prevention toolkit: Five essential steps for first responders [Manual]. U.S. Department of Health & Human Services. https://store.samhsa.gov/sites/default/files/d7/priv/five-essential-steps-for-first-responders.pdf ↵
- Substance Abuse and Mental Health Services Administration. (2018). SAMHSA opioid overdose prevention toolkit: Five essential steps for first responders [Manual]. U.S. Department of Health & Human Services. https://store.samhsa.gov/sites/default/files/d7/priv/five-essential-steps-for-first-responders.pdf ↵
- Centers for Disease Control and Prevention. (2020, September 4). Overdose deaths and the involvement of illicit drugs. U.S. Department of Health & Human Services. https://www.cdc.gov/drugoverdose/featured-topics/VS-overdose-deaths-illicit-drugs.html ↵
- “prevent-overdose-deaths-71k-large.jpg” by Centers for Disease Control and Prevention, National Center for Injury Prevention and Control is in the Public Domain. Access for free at https://www.cdc.gov/drugoverdose/resources/graphics/overdose.html ↵
- Centers for Disease Control and Prevention. (2020, September 4). Overdose deaths and the involvement of illicit drugs. U.S. Department of Health & Human Services. https://www.cdc.gov/drugoverdose/featured-topics/VS-overdose-deaths-illicit-drugs.html ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- U.S. Food & Drug Administration. (2022, May 4). 5 things to know about Delta-8 tetrahydrocannabinol - Delta-8 THC. https://www.fda.gov/consumers/consumer-updates/5-things-know-about-delta-8-tetrahydrocannabinol-delta-8-thc ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- National Institute on Drug Abuse. (2020). Marijuana research report. https://nida.nih.gov/publications/research-reports/marijuana/letter-director ↵
- Shepard, S. (2021, December 6). Can medical marijuana help your MS? WebMD. https://www.webmd.com/multiple-sclerosis/multiple-sclerosis-medical-marijuana#:~:text=Surveys%20show%20that%20many%20people%20with%20MS%20already,that%20attacks%20your%20brain%2C%20spinal%20cord%2C%20and%20nerves. ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- Centers for Disease Control and Prevention. (2021, June 11). Marijuana FAQs. U.S. Department of Health & Human Services. https://www.cdc.gov/marijuana/faqs.htm ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- Greller, H., & Gupta, A. (2020, October 20). Benzodiazepine poisoning and withdrawal. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- This work is a derivative of StatPearls by Kang, Galuska, & Ghassemzadeh and is licensed under CC BY 4.0 ↵
- Greller, H., & Gupta, A. (2020, October 20). Benzodiazepine poisoning and withdrawal. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- National Survey on Drug Use and Health. https://nsduhweb.rti.org/respweb/homepage.cfm ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2021, November). Hallucinogens drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/hallucinogens ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2021, November). Hallucinogens drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/hallucinogens ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2022. Substance use - phencyclidine (PCP); [updated 2022, February 18]. https://medlineplus.gov/ency/patientinstructions/000797.htm#:~:text=Phencyclidine%20(PCP)%20is%20an%20illegal,into%20a%20vein%20(shooting%20up) ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- Crane, C. A., Easton, C. J., & Devine, S. (2013). The association between phencyclidine use and partner violence: An initial examination. Journal of Addictive Diseases, 32(2), 150–157. https://doi.org/10.1080/10550887.2013.797279. ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- Heard, K., & Hoppe, J. (2020, March 19). Phencyclidine(PCP) intoxication in adults. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2021, November). Hallucinogens drug facts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/hallucinogens ↵
- Rosenbaum, C., & Boyer, E. (2021, January 20). Dextromethorphan abuse and poisoning: Clinical features and diagnosis. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2019, May). Methamphetamine drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/methamphetamine ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2019, May). Methamphetamine drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/methamphetamine ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2019, May). Methamphetamine drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/methamphetamine ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2019, May). Methamphetamine drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/methamphetamine ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2019, May). Methamphetamine drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/methamphetamine ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- Boyer, E. W., & Hernon, C. (2019, December 24). Methamphetamine: Acute intoxication. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2019, May). Methamphetamine drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/methamphetamine ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- Boyer, E. W., & Hernon, C. (2019, December 24). Methamphetamine: Acute intoxication. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- Boyer, E. W., & Hernon, C. (2019, December 24). Methamphetamine: Acute intoxication. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2020, April). Inhalants drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/inhalants ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2020, April). Inhalants drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/inhalants ↵
- American Psychiatric Association. (2013). Desk reference to the diagnostic criteria from DSM-5. ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2020, April). Inhalants drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/inhalants ↵
- National Institute on Drug Abuse, & National Institutes of Health. (2020, April). Inhalants drugfacts. U.S. Department of Health & Human Services. https://nida.nih.gov/publications/drugfacts/inhalants ↵
- Boyer, E. W., & Hernon, C. (2019, December 24). Methamphetamine: Acute intoxication. UpToDate. Retrieved March 21, 2022, from www.uptodate.com ↵
A psychoactive compound with the potential to cause health and social problems, including substance use disorder.
The use of any of the psychoactive substances.
Substances regulated by the U.S. Drug Enforcement Agency.
When a person suddenly stops using a drug, their body goes through withdrawal, a group of physical and mental symptoms that can range from mild to life-threatening.
A group of physical and mental symptoms that can range from mild to life-threatening.
The use of alcohol or drugs in a manner, situation, amount, or frequency that could cause harm to the user or to those around them.
A disturbance in behavior or mental function during or after the consumption of a substance.
The biological response of the human body when too much of a substance is ingested.
Defined as 14 grams (0.6 ounces) of pure alcohol.
A female consuming 8 or more drinks per week and a male consuming 15 or more standard drinks per week, or either gender binge drinking on 5 or more days in the past 30 days.
Defined as a pattern of alcohol consumption that brings the blood alcohol concentration level to 0.08% or more.

