15. “Patience required” — Recovery, Part 4
Listen to Chapter 15
|
Have you ever felt like a heavy weight was lifted off your shoulder, only to realize that the weight is — and will be there — for the rest of your life?
That is what I felt like three days after finishing my radiation therapy treatments. I was attending my second ovarian cancer support group meeting online. I recognized some of the faces but was not familiar with the lady who shared the saddest news of the evening. Her cancer had returned within one year of going into remission, and she was now undergoing her second round of chemotherapy. “Where is my tissue box?” I said out loud. Then, I wiped the tears from my face and rejoiced when she said that her new nausea medication was working perfectly.
When it was my turn to talk, I made everyone laugh by telling them about my complicated relationship with boiled carrots. Another participant then admitted that she was still struggling with diarrhea years after finishing treatments. “Could this be me?” I wondered anxiously.
Others expressed their concern about a local oncologist who was not into ordering tests such as CT scans and blood work, especially after the two-year mark had passed. “I have talked to my GP about this, and he will order them for me now,” one lady said. Since I had a CT scan done in January, a PET scan in February, and an MRI scan in March, I hoped that blood work would be the only test the oncologist would order for me in late May, if that.
The following day, March 30, 2021, would have been my mom’s 95th birthday, which she shared with my oldest friend from university, who was turning 60. I celebrated their accomplishments with a long walk, having spent much of the weekend at home, either resting in bed because of fatigue or praying to the diarrhea gods for mercy. Working on the book manuscript had been impossible, much to my regret.
When I got home, the phone rang.
“Just a heads-up,” said my best friend. “I have to go back to the hospital because my lymphoma wound is not healing properly.”
“Wow! I am so sorry to hear that,” I said. How long was her cancer journey going to continue? She had been through so much already. “I will call you every day,” I promised her, and for good reason. A “no visitors allowed” Covid-19 rule took effect the very next day. Since case numbers in the city had begun to skyrocket once again, I felt more grateful than ever to be finished with treatments.
Holy Week sacrifices
On Maundy Thursday, I had not expected to become so emotional while watching the Lutheran Bishop of Saskatchewan reverently washing his daughter’s and grandchildren’s feet in the sanctuary. Nor had I been prepared to cry myself through countless hymns on Holy Wednesday and Holy Saturday. The sacred poetry focused on healing and drew attention to sacrifices that had been asked of me during my journey back to health. And I was not out of the woods yet, as fatigue, headaches, and, of course, diarrhea, as well as belly pains and vaginal discharge continued to upset my body.
On Good Friday morning, I took a deep breath before I opened the drawer of my bathroom vanity, took out the vaginal stretcher, and followed the instructions it had come with. Then, I pressed the start button on my phone’s timer and meditated together with Deepak Chopra. I concluded that my “pelvic homework” had been neither long nor scary four minutes later when I removed the device and cleaned it before putting it back into a boring, see-through plastic bag. Maybe a more exciting storage container would help me accept the fact that I would have to engage in this less than glamorous behaviour four times a week for an entire year. It certainly felt like a chore if not a sacrifice, albeit a small one.
As a frequent traveller prior to the pandemic, I also wondered how I would incorporate this routine if I ever were to leave town for extended periods of time again. Visions of locking myself into a bathroom and lying on the floor or in an empty bathtub, device in hand, made me cringe and crave Nutella on the spot. At least my new travel companion would not be as cumbersome as the sleep apnea equipment my oldest sister had been required to pack whenever she wanted to see her children and grandchild.
On Easter Sunday morning, I spontaneously decided to go on an early-morning walk. Enjoying the sunshine and blue sky, I felt like someone (Jesus?) had literally pulled the stone from the tomb in which I had found myself during treatments. After a hearty breakfast and listening to the joyful organ prelude that I had pre-recorded, I sang countless “Hallelujahs” while worshipping online, albeit by myself. For the first time in a long time, the words “untroubled” and “carefree” popped into my head, much to my delight.
In the afternoon, I got in touch with many relatives and friends to wish them a Happy Easter. My intention was to make them and myself laugh by emphasizing that I did not resemble a rabbit after all, despite sporting white hair and eating boiled carrots almost daily. A delicious, diet-friendly supper, courtesy of my trusted neighbour, made it official: this had been an excellent Easter Sunday!
“When do you think you will be able to eat real food again?” my colleague, the fellow German who had visited me at the hospital when I had surgery, joked during our usual Sunday evening chat.
“When I run out of chocolate Easter eggs!” I quipped. My answer signalled to both of us that I was on the mend, both physically and mentally.
Two days later, my favourite radiation oncology nurse wanted to know how I was doing. She was pleased to hear that I was managing the side effects to the best of my abilities. “Be gentle with yourself,” she reminded me before confirming the time and date of my follow-up appointment in late May. The radiologist did not need to see me, only the medical oncologist, the nurse informed me. “And you won’t need to do any blood work either.” Thank the Lord! I never once minded being poked by a lab technician or nurse since I have good veins, but I always hated waiting for the results afterwards, for obvious reasons.
I also wondered when it would be safe for me to go to the pool again. “Give it four to six weeks,” the nurse advised. Her answer pleased me, even though I knew I was not going to rush back to my favourite physical activity anytime soon. Under normal circumstances, I would have considered booking myself into the “spa,” a resort-style hotel with a geothermal pool in a small prairie town 45 minutes west of the city.
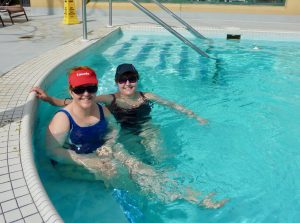
“Darn pandemic,” I said to my twin sister that evening. We had such a great time the last time we stayed there in August 2019 to celebrate our birthday. “It would have been the ideal place to ‘take the waters’,” my older sister in Germany commented, and I could not agree more — except that a “no travel” advisory had been in effect for weeks now, which some people blatantly chose to ignore, arguing that they just “needed to get out.” Others continued to demonstrate in front of the legislative building and, to my horror, also outside the hospital at which I had gotten my CT and MRI scans.
“It is all a hoax,” they claimed, referring to the provincial health authority as “serial killers.” Why did these individuals not realize that they put us all at risk, especially folks like myself and my best friend whose immune systems were compromised?
A shot in the arm
On the afternoon of Friday, April 8, 2021, I made sure to wear a short-sleeved shirt and put my medical insurance card into my wallet before driving myself to the university. Seven minutes later I pulled into the same lot in which I had parked prior to all my classes being moved online over a year ago. A yellow-vested individual greeted me, while another directed me to a spot closer to the building which I needed to enter to get my first shot.
After showing my ID to a security officer and answering a few Covid-19-related questions, I felt weird lining up in the same gym in which I used to play badminton years ago. I had quit after the fellow professor who loved to chase me around the court decided to retire and moved away. To everyone’s surprise, including my own, I began taking Zumba and Jazzercise classes at a YWCA fitness centre near my house and stuck with it for several years. “I love the music and the dance routines,” I remember telling my twin sister. “The best part is that I never see any of my students there who assume their university professors live in their offices 24/7.”
When it was my turn to check in to be vaccinated, I showed my medical card and then walked around the corner to receive my shot. The nurse first went through a detailed questionnaire; after finding out that I had finished radiation therapy less than two weeks ago she left her station to pick up a form.
“Please sign this to indicate that we cannot guarantee full efficacy due to your compromised immune system,” she said when she returned. Then she administered the Pfizer-BioNTech vaccine and asked me to wait for 15 minutes at the back of the gym.
Feeling unexpectedly underwhelmed, I thanked her, found a chair, and checked my watch to figure out when it would be safe for me to leave. I was not impressed when I noticed that several people who had taken a seat well after me, got up early and exited the building. “Well, at least they got their shots today, which is a good thing,” I concluded on my way back to the parking lot.
“My upper left arm is killing me,” I announced to my twin sister later that afternoon when it was time for our daily workout. I was not surprised as it had also hurt when I received the flu vaccine in early November of last year.
“We did a bunch of biceps and triceps lifts yesterday, so you might be sore from that as well,” she noted.
When I woke up in the middle of the night with even more pain, however, I decided it was time to pop a pill. “Can you adjust today’s exercise routine, so it won’t involve me lifting my arm?” I asked her. My twin sister did, and by Saturday morning, my muscle soreness and arm pain were gone.
Many firsts
That same morning, I also enjoyed my first cup of black tea since my last chemotherapy treatment on January 20, 2021. The hot, dark brown liquid had tasted better than chocolate — at least initially. Then, I started to cough, my throat began to itch, and my irritated bladder sent me a message as well. “I’d better go easy on the caffeine for the next while,” I decided, as not to stress my body unnecessarily.
A fascial release massage that afternoon helped me relax, as did a lovely conversation with my massage therapist. We had kept in close touch ever since my diagnosis. I was ever so grateful that she never once complained about me moving appointments and happily triple-disinfected the treatment room prior to my arrival. To my delight, she commented on how much my hair had grown and its colour but refrained from identifying body parts that desperately needed shaving.
Three days after the massage, I finally tried it, noticing how soft the hair under my armpits had grown back. While I did not dare to pluck my unexpectedly bushy eyebrows, I did put mascara on my baby eye lashes. Life was good!

Exactly one week after being vaccinated, I tried out a new, bright red lipstick and wore a nice pair of earrings in honour of the 333rd birthday of Johann Friedrich Fasch, my “composer husband,” as I have been known to call him. Under normal circumstances, I would have attended the 16th International Fasch Festival in the small town of Zerbst in Central Germany, where Fasch had spent 36 years as court Kapellmeister or director of music.
In fact, I had been scheduled to present two public lectures and a conference paper on archival materials related to his life and works over the course of five days. Instead, I was waiting for the festival organizers, who had already moved the festival from mid-April to mid-June 2021 due to Covid-19 restrictions, to announce its cancellation — which they did on April 20, 2021, a first in the 30-year history of my favourite baroque music festival.
“How do you feel about that?” my best friend asked me on the phone. I had called her with the news while taking my car for a spin down a secondary highway, passing two huge Travel not recommended signs on the way.
“I think I would have been more disappointed if it had run as usual and I could not have been there,” I told her. In the past, relatives and friends had teased me mercilessly for planning my life around this biennial event, a highlight in my work life ever since I had attended my first festival as a graduate student in 1993. Now, I could not imagine what the next one would look like — if there would be one — and did not care when my scholarly book on Fasch would be finished, if ever.
“Wow,” I thought, after acknowledging how little I cared about my career trajectory these days. Clearly, I had changed since last July; in fact, I hardly recognized that person. “I do, and I have missed her terribly,” said the little girl inside me, and hugged me for the first time in a long time.
Living with the fear of dying
“I have excellent news,” my clergy friend from Alberta said on the phone the next day. She had been cancer-free for five years! I was so relieved and grateful to be able to celebrate this milestone with her, albeit virtually.
Unlike me, she had almost died during her first chemotherapy session due to a severe allergic reaction and decided to discontinue them in favour of taking medication. Every six months she had to go in for a check-up, and every single one had been a nail-biter, to say the least. I wondered whether it was going to be like that for me as well, just at shorter intervals because the recurrence rate of endometrial cancer was much higher than breast cancer.
“What’s on your agenda today, Barb?” she asked, bringing me back into the present.
“I am going to attend a webinar hosted by the Ovarian Cancer Society tonight,” I told her. According to the support group participants, the presenter was a most engaging and knowledgeable individual. Moreover, the topic was of great interest to me as I was still grieving my friend’s untimely death in mid-October 2020.
“Hello everyone,” said the moderator to 48 people (if not more) who had logged on from all over Canada. About five minutes into the presentation, I realized that I had misunderstood the title, “Living with the fear of dying.” It was not about the possibility of one’s cancer reoccurring. Instead, the speaker addressed the taboo of talking about death and dying in Western Culture and what to do about it.
“Should I leave?” I asked my main guide, somewhat frustrated with my “chemo brain.” “Stay put and pay attention,” he answered. “You’ll learn something important.”
He was right, of course.
To my surprise, several of the fears associated with a terminal diagnosis that were identified turned out to apply to me, even though my prognosis was excellent. I worried less about my academic legacy — what else were students, colleagues, and publications for? — and more about being remembered as a kind relative and a supportive friend, especially since I had never given birth or been partnered. As someone who had watched her mother look after her ill husband, my father, for many years, I also did not wish to be a burden to anyone.
Missing out on living life to the fullest resonated the most with me. “Your body cannot tell the difference between good stress and bad stress,” my oldest sister would remind me when I had wrestled with life-work balance issues in the past. What, if anything, would I change if I had only a few more months or years to live? “This is heavy stuff,” I concluded, unsure as to whether I should watch the rest of the presentation or not.
The speaker went on to give examples of what dying people talked about. I immediately identified with feeling isolated, not just during a pandemic, and having been told by others, including my main guide, to adjust my attitude. Like terminally ill patients, I had struggled with loss of control and experienced feelings of unfairness during my cancer journey, especially at the beginning.
“In truth, we have little and sometimes no control over the things that really count,” the presenter emphasized. Dying was “not a punishment for not trying hard enough and being good enough,” she stressed. As an eternal optimist and woman of strong faith, I had never viewed the end of my life through that lens. Would I blame myself if the cancer returned or would I take it in stride?
The question of whether oncologists should pose a “Patient Dignity Question” intrigued me. I would certainly have appreciated being asked by my medical team at the very beginning of my journey what they needed to know about me as a person to provide the best care.
A quotation from Stephen Jenkinson’s film The Meaning of Death touched me deeply as well. It read: “All we need of you is that you be human, now. Our work is to sort out what being human should be in such a time.” Was this a map of sorts for how I was to approach the future? If nothing else, I viewed it as a challenge that appealed to my competitive nature.
Two comments from the questions and answers session were particularly memorable. The first one — “Is it wrong not to want to engage with the cancer world after finishing treatments?” — gave me pause. I certainly did not want to become an attraction of sorts as an author, with “university prof shares cancer journey” as the tagline. Nor did I want to be pitied, judged, or criticized for what I had been through.
Would receiving negative feedback perhaps feel like when others introduced me as “the German lady”? People’s reactions to meeting me — “You don’t have much of an accent,” I would be told — had ranged from bizarre (“Do you know my third cousin from Düsseldorf?”) to plain rude (“I like your red top — they only wear black or grey in Nazi movies”). I determined that my best course of action was to focus on the overall goal of this book, i.e., to educate and entertain others and raise funds for cancer research. The rest — whatever that meant — I would surrender to the universe to handle.
The other comment made me laugh even though it was not meant as a joke. A 20-year cancer survivor had questioned her fear of “dying of something stupid.” My inner stand-up comedian promptly offered a myriad of possible scenarios, including death by poisoning from boiled carrots or by choking from chocolate-covered almonds.
After signing off, I realized that this webinar represented an important step in my own healing journey: it had given me a glimpse of what my personal space in the world of cancer survivors might look like.
The final question
My GP called me the next day, Thursday, April 22, 2021.
“How are you, Barb?” he asked.
“I did not expect the side effects from radiation to be this awful,” I replied. Then, I listed the most memorable ones. “I am also still dealing with low energy and fatigue — I had another bad episode last Saturday that came out of nowhere,” I told him. The numbness in my left foot and right thumb were another daily reminder of having finished chemotherapy only (or already?) three months ago, as were the occasional headache, sleepless night, and hot flash.
“Give it time,” my GP advised and wondered whether I had any questions for him. “I have an entire list,” I said, dead serious. “Dr. Barb” had been working on them diligently over the last couple of days.
Since I had received my first shot two weeks ago, could I start going on walks again with others who had been vaccinated as well? And would it be okay to begin playing at church again as of mid-May, at which time the pastor and church musician would be vaccinated as well? “Yes” was my GP’s response to both queries.
Little did he know that my pastor would successfully talk me out of the latter idea the very next day. “It’s not safe yet,” she argued convincingly, citing viral load concerns and the fact that services would not be held in the big sanctuary until Covid-19 restrictions were lifted. “Fair enough,” I told her and volunteered to record a prelude for Pentecost Sunday in late May.
My next question focused on when I could join my relatives out west.
“It’s been really tough,” I said with a big sigh. I had not seen them in the flesh since late 2019 and, despite being able to use technology to communicate with them regularly, missed them more every day.
“I understand that, but let me explain something to you,” my GP replied. Then, he launched into an eloquent mini-lecture on how dangerous the new variants of Covid-19 were. Referencing medical journals (“What, no footnotes?” I thought, but kept my mouth shut), he described the seriousness of the situation, and insisted that extreme caution was the best course of action. The bottom line was that my GP advised me not to travel until I had received my second shot and then wait at least two weeks before I said goodbye to my friends in town.
“That’s not really the answer I was hoping for,” I said. Since the province I lived in was leading the country as far as vaccinations were concerned, I had talked my twin sister, who was scheduled to receive her first shot in late April, into booking a cheap flight in late May. “Come and get me,” I had begged her. A miracle of sorts would now be required for that to happen; travelling out west sometime in June was more realistic.
“Thanks to Covid, this health marathon is turning into an Iron Woman competition,” I moaned. My GP’s response — “patience is required” — was an effective reminder that making plans of any kind during a pandemic was futile.
Then we discussed when I might be well enough to return to my day job in the second half of 2021.
There was no denying it: the radiation therapy treatments had taken an unexpected toll on me, specifically regarding my energy household. With that backdrop in mind, I told my GP that “pre-cancer Barb” had been able to generate seemingly limitless energy and committed much of it to her work year-round. The medical teams’ ambitious treatment plans for “cancer patient Barb” had depleted both her energetic savings account and line of credit and, as a result, seriously damaged her energy credit history. Excelling at minimum wage jobs in the physical fitness and attitude sectors had not been enough to prevent declaring energy bankruptcy after only a few short months. “Post-cancer Barb” was enrolled in an energy management programme but continued to struggle to make monthly rent payments. How long would it take for her to inspire confidence in her energy bank again?
In other words, there was no way to tell when I would recover from the mental fatigue that had quietly replaced my “chemo brain” symptoms after radiation therapy treatments had begun, if ever. Despite engaging in daily exercise — and looking perfectly fine on the outside because of it — good energy days now felt completely different and were the exception, not the rule.
This new reality also had an impact on breathing life into my cancer story on paper. How difficult could it be to write a book that involved no actual research besides scrutinizing my diary to ensure chronological and contextual accuracy?
Prior to the surgery, I would have given myself a month and then, as a seasoned and fast writer, would have tried to get it done in half the time. Instead, I had woken up feeling sluggish, listless, and lethargic, if not uninspired on most days in March and many in April and, to my horror, turned into “Zombie Barb.” The daily editing process — which has always been my favourite part of the writing process — was turning into a terrible chore.
I had even complained to my main guide about it on Easter Monday.
“Therapeutic or not — this is hard,” I said.
“Who said it was going to be easy?” he replied.
That comment made me laugh because he had just quoted a response that I would often give to students expressing their dissatisfaction with an assignment to me. To cheer myself up, I followed my main guide’s advice to add clever subtitles to what I had written so far for a couple of days, only to admit to myself that I had run out of steam and would need to finish the manuscript later.
When my inner child promptly nodded in agreement, I realized that the universe had never set a specific deadline or indicated when I should or could stop keeping a cancer diary.
The cut-off date as far as my health journey was concerned dawned on me when I arrived at the last question to pose to my GP.
“What is my current patient status, now that I have finished radiation therapy?” I asked him.
“You are in remission, Barb,” he announced, “because none of the scans have shown any evidence of cancer being present.”
“That was the answer I was hoping for,” I said, literally jumping up and down for joy. I had not realized how much I had craved hearing these words.
“What a relief!” my relatives and close friends said. “You have no idea,” I replied and smiled from ear to ear. Life was really good!
And this marks the end of my recollections of how I coped with cancer during a pandemic. It is, however, not the conclusion of this book.

