Expanding Active Learning
3
Karin Hamilton and Tricia Todd
Keywords
interprofessional, team, health profession, course, case study
History and purpose of the course
The New Health Professions Team course began as a conversation between two instructors – one from the field of public health, and the other from the field of veterinary medicine. The result of the conversation was an agreement that the current common focus on interprofessional teams as strictly teams, of health professionals providing direct patient care in a clinical setting, was limiting. Having worked on complex professional challenges ranging from zoonotic diseases to foodborne outbreaks, the instructors wanted to demonstrate how the skills and competencies of working in interprofessional health teams go beyond the hospital walls.
In addition to expanding the scope of interprofessional health teams, the instructors wanted to apply the concepts of interprofessional education to undergraduate student learning. The goal was to help undergraduate students learn about the competencies (skills, attitudes, and behaviors) needed to work effectively in teams made up of diverse professionals striving to solve complex health problems. The challenge was to teach the interprofessional competencies to students before they enrolled in health professional programs.
Undergraduates are in a unique situation as they have little to no professional identity or role affiliation. Often, teaching them about interprofessional team dynamics is challenging because their own past experiences do not represent the complexities of an interprofessional team. In addition, the many skills and competencies interprofessional research identifies as vital often fall into the broad and elusive “soft skills” category. With soft skills often best gained through experiences, teaching the competencies we identified required us as instructors to bring simulation, cases, role play, and other interactive activities into undergraduate, professional practice courses.
Goals and Learning Objectives of the Course
The goals of the course were to raise awareness and build interprofessional competency among pre-health students. The original competency domains and learning objectives for year one, Spring 2015, were developed by reviewing the competencies identified in the Interprofessional Education Collaborative (IPEC) Report on Core Competencies for Interprofessional Collaborative Practice (IPEC, 2011) and the University of Minnesota Student Learning and Development Outcomes (UMN SLO, UMN SDO). Due to the narrow focus on patient-centered teams in the IPEC report, the instructors expanded the learning objectives to apply to interdisciplinary teams addressing public health challenges. This resulted in fourteen learning objectives within the four IPEC domains of Values and Ethics for Interprofessional Practice, Roles and Responsibilities, Interprofessional Communication and Team and Teamwork.
The following year, Spring, 2016, the objectives were reorganized into content specific objectives and personal growth objectives. The content specific objectives focused on the four IPEC domains, while the personal growth objectives focused on self-assessment and building self-awareness around development of interprofessional competency. This reorganization was done to better align the learning objectives with the course goals and subsequent activities while also making the learning objectives clearer to the students and more measurable.
In 2016, an updated edition of the IPEC report (IPEC, 2016) was published with the language sufficiently broadened so that the IPEC domains will now provide the foundation for the 2017 course objectives.


Figure 1: Students participating in the Marshmallow Challenge activity
Evolution of the course
Spring 2015 Class
The course was developed in Summer and Fall 2014 and first taught in Spring 2015. The semester was designed to include a mix of theory around interprofessional competencies, real life examples, discussion, and activities for each class. Some examples of the activities used include: 1) practicing giving and receiving feedback; 2) completing the Marshmallow Challenge (Figure 1) (Wujec, 2015); and 3) watching and discussing selected videos demonstrating both good and bad communication skills. In order to connect the interprofessional competencies to teams working in the health professions, sites of the students’ future careers, two realistic disease outbreak case scenarios were created and used throughout the course: one based on rabies and the second on Lyme disease. Students were split into four teams, two of which worked through the rabies case and two of which worked through the Lyme case. The students were assigned to teams with the goal of maximizing team diversity in gender, college, degree program, and health career interest. The instructors provided teams with a weekly update on the progression of their respective case.
While the students were learning about the cases, they were doing so in teams and reflecting on team dynamics. Therefore, the assignments focused primarily on (1) self-reflection and evaluation, (2) writing assignments about the interprofessional competencies within the case scenarios, (3) obtaining external feedback on one’s interprofessional competency level, (4) providing peer evaluations of team members, and (5) a final team presentation. For their final team presentations, teams were tasked with describing the stakeholders and their roles and responsibilities with regard to the assigned scenario. They were asked to provide examples in the scenario where interprofessional competencies were demonstrated well and where they could have been improved. They also proposed possible solutions to the case.
Early in the semester, the instructors quickly learned how challenging it is to teach the concepts of interprofessional teamwork to pre-professional students. Students typically relied on previous team-based experiences, often in sports settings, to assess their current knowledge and skill levels as a team member. While there are some similarities, the dynamics at play in interprofessional teams are far more nuanced and often linked to roles, responsibilities, and power. An additional challenge the instructors observed was the lack of accurate self-awareness among many undergraduates. Frequently, the students ranked themselves at the highest level of competency in interprofessional skills when in reality most did not have sufficient experience or evidence to support this level of competency. As the interprofessional competencies are less “concrete” than other forms of knowledge, such as descriptions of different types of bacteria, it was also challenging to write the assignment and activity instructions with enough detail to satisfy the students, while leaving enough room to encourage students to think independently and reflect at a deeper level.
In this class with pre-health students the cases had a health focus. The intention, however, was to have the students focus more on the interprofessional dynamics versus solving the health problem. To keep students from focusing on solving the case quickly, they were given updates at the end of each week to further unfold the case. This resulted in the cases and related assignments being relatively disconnected from the theory and activities completed in class. Ultimately, there was less interest and engagement in the cases and the final presentations did not reach the level of depth and reflection desired by the instructors.
After teaching the first year, the instructors decided to push the course to a new level and applied for an Experiments in Learning Innovations grant. The vision was to create an ongoing, experiential-based case where students would work in interprofessional teams throughout the semester to problem solve, and while doing so, would be made aware of interprofessional challenges within a team, as well as practice strategies to overcome them. The instructors were awarded the grant, and proceeded to initiate the development of their “big, hairy, and audacious goal” (BHAG). And as happens, life intervened. Weddings, surgeries, global travel, and a variety of other situations caused the instructors to tone down the goals for the Spring 2016 class and create a two year implementation plan instead.
Spring 2016 Class
For the 2016 class, the instructors consulted with the Minnesota Department of Health and decided to modify a pre-existing foodborne disease outbreak training scenario based upon real outbreak experiences (US FDA, 2015). The most significant modification was adapting the case scenario to occur on campus so the students could have a context that also allowed for interactions with local health professionals. The course was broken into four phases:
Phase 1 (4 weeks): Interprofessional Competencies
In this phase, the students were given interactive class-based activities to learn about concepts such as sharing power, roles and responsibilities, communication, developing group norms, team dynamics, and cultural humility. This phase was similar to the structure from the original Spring 2015 course.
Phase 2 (3 weeks): Subject Matter Expert (SME) Teams
The students were assigned into uniprofessional SME teams and first introduced to the fictional on-campus foodborne disease outbreak scenario within these teams so that they could initially learn about the roles and responsibilities of the various experts who would be engaged in the case. There were three teams: Hospital/Laboratory, Epidemiology/Public Health, and Environmental Health/Food Safety. As in 2015, the students were assigned to teams with the goal of maximizing team diversity in gender, college, degree program, and health career interest. The first class in this phase started with time for the students to meet their teammates and establish their new teams with the optimistic hope that they would use some of the skills and activities introduced in Phase 1 of the course. However, rather than taking time to team-build, most teams jumped right into the case scenario. When brought to their attention that they skipped right over the processes of team-building identified in the first few weeks of class, they all made the connection and asked to have a second chance.
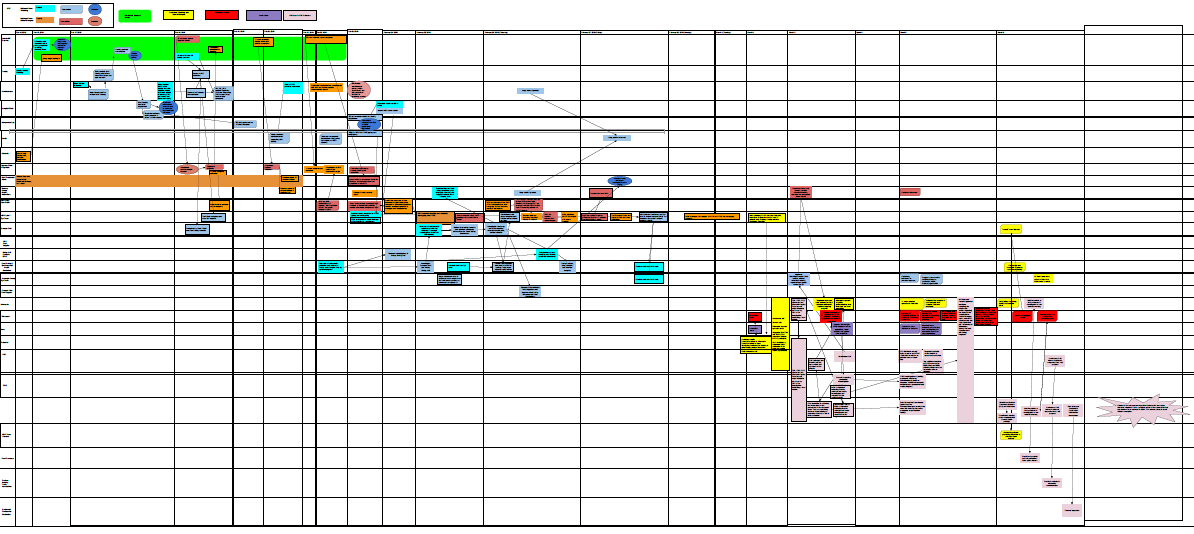 Figure 2: Example of interprofessional team case map
Figure 2: Example of interprofessional team case map
Students were also introduced to stakeholder and systems mapping and given the option of several free tools (Diagramo, Draw IO, Excel, Lucid) to choose from as they were tasked to create team maps of the outbreak scenario. Each week the teams received SME specific updates for the case which they added to their respective case maps (Figure 2). One additional assignment during this phase was for students to interview a health professional in the same field as each team’s SME to help them develop a better understanding of the roles and responsibilities of that particular health profession. The health professionals were from the community and volunteered their time to talk with the students. During the last class of this phase, the students were surprised with an unannounced press conference. Volunteers role-played as reporters and interviewed the teams on what was happening in the case at that particular time (students had already received communication training and practice in Phase 1). The volunteer reporters created and shared some very interesting headlines from the information they received during the press conference (Figure 3). Phase 2 ended with self and peer evaluation on the interprofessional competencies within their SME teams.
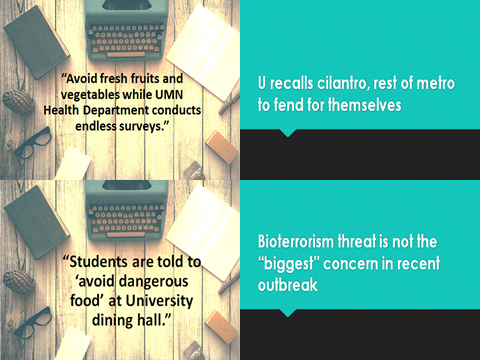
Figure 3: Example headlines created by role playing reporters after an unannounced press conference activity (left) and a second announced press conference (right)
Phase 3 (4 weeks): Interprofessional Teams
At this point in the semester, the students were reassigned to interprofessional teams to continue problem solving the case. An interprofessional team consisted of 1-2 members from each of the previous SME teams. Once again, the students jumped right into the case instead of team building. Again the issue was raised, and the students explained that because they knew each other, they had skipped over the more formal processes of team-building.
Each new interprofessional team was challenged to combine the three SME team case maps into one new interprofessional team case map. Again, local health professionals volunteered to meet with the students in this phase. This time volunteers played roles within the case scenario and provided information and updates the interprofessional teams needed to continue mapping and figuring out the case. Another press conference occurred during Phase 3, but this time the teams were given advance notice to prepare a statement and be ready to answer questions. These press conferences were included to help them understand and deal with the public communication necessary when working on a case where the public has a vested interest. Phase 3 ended with the conclusion to the foodborne disease outbreak case scenario.
Phase 4 (3 weeks): Wrap Up
Throughout the course, students completed individual writing assignments about the interprofessional competencies, incorporating self-reflection and evaluation, and peer evaluation. In addition, each interprofessional team was tasked to reflect on the interprofessional competencies, both as found in the case scenario and as experienced working in their teams throughout the third phase. Finally, each team led the class through a new activity to introduce, practice, and debrief about one of the interprofessional competencies they found to be most important. Several of the health professional volunteers participated in a panel discussion about their real life experiences working in interprofessional teams. The course wrapped up with a summary and debrief about what the students liked and what they would change in the course.
Instructor reflections on lessons learned from the course
Teaching Interprofessional Team Skills
Whether educating undergraduate students or those in health professions programs, teaching and evaluating interprofessional team skills is challenging. Each semester we have tightened and clarified the learning objectives in an effort to help students understand the focus, purpose, goals, and expected outcomes of the course. A specific challenge that is not unique to undergraduates, but also pertains to professional students and professionals, is the tendency to want to focus on the scientific problem, not the interprofessional challenges. Building intentional interprofessional challenges into the fictional case scenarios has helped students to understand and appreciate the importance of trust, communication, roles, responsibilities and the team-building processes; however, it is an ongoing challenge to find the balance between interest and motivation to solve the case versus learning about and developing interprofessional competencies.
Solving the Case vs. Building the Competencies
In an effort to make the course more engaging and interactive, we used two variations of multi-week cases that the students needed to solve, all the while paying attention to both the case and the interprofessional challenges. While providing a realistic scenario helped demonstrate the interprofessional team competencies, the students generally lacked the knowledge and experience with their subject matter expertise roles, often leaving them confused and disengaged. Students tended to stay in their student role and wanted to solve the case rather than Instead of taking on the role they were assigned, instead of taking on the role they were assigned, and focusing on the process and team dynamics. This is a normal tendency, even in a real team situation, as often team dynamics are not as clear, or as easy to address as the scientific problem at hand.
Real World Perspective
As mentioned previously, finding the “right” case that students can relate to without having had significant real world experience in the health field is an ongoing challenge. We started in 2015 with two cases, one focusing on rabies and the other on Lyme disease, which had mixed results. In 2016, we used a fictional on campus foodborne disease outbreak which again had mixed results. Some of the students thoroughly enjoyed learning about and role-playing in different health professionals than they had previously been aware of whereas other students were frustrated by not be allowed to focus on their specific health profession interest. In an effort to address this, the course has changed each semester it has been taught, to provide an engaging realistic case that both fits in students’ future career interest while expanding their experience and perspectives of interprofessional teams working on health challenges.
Interacting with Health Professionals
To address the lack of familiarity with the professions, we utilized real health professionals as volunteer role players within the case. Our volunteers for 2016 included a physician, state and county epidemiologists, and graduate students from “Team Diarrhea” at the Minnesota Department of Health. The student teams took different approaches to interacting with the health professionals with some meeting in person as a team, others sending one or two student representatives, and some communicating via email or the telephone. The interactions by students who met in person with the health professionals seemed to have had the greatest positive impact both on the students and the volunteers. The volunteers generally enjoyed communicating with the students as they appreciate our interest in building interprofessional competence in future health professionals.
Systems Thinking
In addition to learning about interprofessional teams, we are helping students understand how systems (e.g. public health systems, healthcare systems) function. Previously, this was a challenge because students had a limited understanding of the various stakeholders needed to solve complex health challenges. Systems thinking requires enough awareness of the parts of the system to really appreciate how they impact each other, and where there will be similar challenges to those found in interprofessional teams. In Spring 2016, the students were taught how to develop a case map. This activity was appreciated some students who saw the map as a useful tool and dreaded by others as a “busy work” task.
Self-Reflection
The most important goal of the course is to help students learn about and practice the skills, attitudes, behaviors, and competencies needed to work effectively in interprofessional teams. This requires students to spend time reflecting on their own actions and the actions of others. We have built in a significant number of reflection activities throughout the semester. One observation is that students generally lack the ability to reflect with any real depth or even accuracy. Therefore, it is essential to give students sequenced guided reflection questions to help them reflect at a deeper level. In both 2015 and 2016, we found students tended to have an inflated view of their own interprofessional skills. We also learned that students do not like to provide feedback to each other, particularly if it has any sense of criticism. Teaching students how to critique and give feedback is an ongoing challenge and yet an essential skill as a member of an interprofessional team.
Incorporating Technology
One of the new goals after receiving the Experiments in Learning Innovations grant was to incorporate technology to support the class. We learned a number ways to use Moodle to help provide a clearer course structure using the four phases, and added a new mapping tool that students could use to record case progress, tracking stakeholders, communications, decisions, and so on. While we feel the case mapping is a useful skill, particularly in following an extended case scenario, we learned through reflection assignments and a feedback session that not all of the students shared that opinion. As we move into the next iteration of the class, the plan is to continue to explore technology that can assist the students in the learning process.
Assessing Student Learning
Student learning has been assessed formally and informally through a variety of methods including writing assignments, self and peer evaluations, self-reflection, team case mapping, final team presentations, and feedback sessions. Grading rubrics were used for formally assessed writing and final project assignments. We continue to address the challenge to effectively articulate the reflection and final team project assignments so that they convey, guide, and support students in developing the depth of critical thinking we desired.
Next Steps
The Experiments in Learning Innovations grant offered us the opportunity to think creatively about the course: how to make it more experiential, and how to better integrate interprofessional competency theory with real world experiences. While the Spring 2016 class has shown significant improvements from the Spring 2015 class, we recognize the opportunities for improvement and look forward to adding some additional activities in the third iteration of the course in Spring 2017 based on our experiences and student feedback. The core interprofessional competencies will remain the basis for the course, and each class will continue to feature an activity that engages students in practicing those competencies. To allow for more in-class time for the activities, case studies, discussion and reflection, the classroom so in the sense that students will complete readings or learning activities about the competencies before in-class activities each week. Some of the new learning activities will be set up as interactive online modules created using Articulate Storyline software, and other video resources.
Getting the case study “right” has been one of the biggest challenges with this course. We started with two infectious disease case studies that two teams each worked through over the semester in a relatively passive sense. In the second iteration, we used a foodborne disease outbreak case study that required more interaction and integration into the course. For the case components of the Spring 2017 course, we plan to have the students participate in two distinct case modes. One will involve working through weekly cases involving interprofessional health teams, with each case study tied to one of four interprofessional competency domains. We hope having a larger variety of case scenarios will allow students the comfort of thinking about interprofessional teams through their future health profession lens, as well as pushing them to learn about and appreciate the contributions of other health professions they may work with in future careers.
Second, student working in teams will problem solve a relevant health challenge that they may encounter on campus. For example, they could choose binge drinking, mental health, or some other topic that is both relevant and requires working with a diverse group of people to problem solve. Having all groups focus on the same challenge will hopefully create some competitive tension resulting in deeper team dynamic experiences. Each group will be tasked to develop a proposal on how to approach the complex health challenge on the campus. The interprofessional competencies will need to be integrated into their approach and proposal. The groups will use the case mapping tool from the Spring 2016 course to identify stakeholders and approach the health challenge with systems thinking. Students will also need to interact with local health professionals, as well as others, while developing the proposal to address the health challenge. We will continue to explore new ways to assess student learning of the interprofessional competencies as well.
The initial intention, to raise awareness and develop interprofessional competencies among pre-health profession students, remained the same throughout the evolution of the course. The question of how to best do this has been a constant challenge for us. One factor that keeps us motivated is the recognition that this challenge is not unique to teaching interprofessional competencies to undergraduate students, but is an ongoing challenge among health professionals as well. Feedback from students’ reflections (some sample quotes below) through writing assignments and a feedback session on the final day of class has helped us to recognize that even if the course is not perfect, students are learning and so we continue to push on modifying and teaching this course. The following comments reflect students’ comments overall:
- Previous to this course, I had considered communication to be active talking and active listening, but it is so much more.
- I have learned to be more self-aware and self-critical, but have a long way to go to fully develop reflective skills that reveal five levels of why.
- Because of my experience in this class, I think I will be better outfitted in the real world for interprofessional work as it has helped me understand the hardships and false assumptions that can be made when working with others not in my field of “expertise” per se at least in the scenarios presented to us.
- Entering this class I thought I already had a fairly decent foundation for working in teams. Throughout school and extracurricular activities I have always worked in teams in some sort of setting. Little did I know I had a weak foundation that needed to be broken down and rebuilt if I wanted to see any measurable improvement in my interprofessional team skills.
References
Interprofessional Education Collaborative (IPEC) Expert Panel (2011). Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, D.C.: Interprofessional Education Collaborative.
Interprofessional Education Collaborative (IPEC) (2016). Core Competencies for Interprofessional Collaborative Practice: 2016 update. Washington, DC: Interprofessional Education Collaborative.
U.S. Food and Drug Administration (FDA). ‘Stealthy Situation’ of Food Related Emergency Exercise Bundle (FREE-B) http://www.fda.gov/Food/FoodDefense/ToolsEducationalMaterials/ucm295902.htm. Accessed March 15, 2015.
University of Minnesota (UMN). Student Development Outcomes (SDO). http://www.sdo.umn.edu/. Accessed March 15, 2015.
University of Minnesota (UMN). Student Learning Outcomes (SLO).
http://academic.umn.edu/provost/teaching/cesl_loutcomes.html Accessed March 15, 2015.
Wujec, Tom. Marshmallow challenge. http://www.tomwujec.com/design-projects/marshmallow-challenge/. Accessed March 15, 2015.
Acknowledgements
We would like to acknowledge and thank the following people for supporting us in this course development and evolution and/or volunteering to interact with our students during the course.
Judy Beniak, DNP, MPH, RN, Director, Health Careers Center
Christina Petersen, PhD, Education Program Specialist, Center for Educational Innovation, Office of the Vice Provost for Faculty and Academic Affairs
Yelena Yan, Instructional Designer, Academic Technology Support Services, Office of Information Technology
Dave Johnson, MPH, Supervisor, Hennepin County Epidemiology
Dave Golden, Director of Public Health and Communications, Boynton Health Services, University of Minnesota
Carol Nelson, MD, Physician, Boynton Health Services, University of Minnesota
Joshua Rounds, MPH and Dana Eikmeier, MPH, Epidemiologists, Minnesota Department of Health
Team Diarrhea students, Minnesota Department of Health
Tracey Dutcher, DVM, MS, DACVPM, One Health Coordination Center, US Department of Agriculture: Animal and Plant Health Inspection Service: Veterinary Services

