9 Social Work Practice and Mental Health Services Outside of Urban Settings
Nuelle Novik; Brent McKee; and Karmen Pearce
This chapter provides an overview of social work practice focused on the delivery of mental health services in rural, remote, and northern communities. As social workers, we know that the prevalence, scope, and range of mental health issues in locations outside of urban centres is significant, and has an impact on the lives of individuals, families and communities. We also know that populations living in these communities don’t always have adequate and necessary access to mental health services and supports. In efforts to fill existing gaps in mental health services, social workers living and practicing outside of urban centres are required to work collaboratively and creatively, while utilizing generalist social work practice skills. Increasingly, mental health issues are a growing public health concern in Canada, with mental illness now identified as one of the leading causes of disability (Chen et al., 2020).
This chapter will highlight the characteristics of rural, remote and northern communities that affect mental health service delivery from a social work perspective; it also discusses select mental health-related issues. Attitudes and beliefs that result in stigma related to mental illness, and towards those experiencing mental health challenges, will also be explored.
Learning Objectives
By the end of this chapter you will have had the opportunity to:
- Understand the scope of practice of social workers providing mental health support services in rural, remote and northern settings.
- Describe factors influencing mental health and addictions outside of urban settings.
- Identify common types of mental health concerns found in rural, remote, and northern settings.
- Understand the barriers and enablers for social workers at the micro-, mezzo- and macro-levels of mental health service provision in rural, remote, and northern settings.
- Recognize how the stigma surrounding mental illness affects service access in locations outside of urban settings, and to identify strategies to reduce that stigma.
What is Mental Health?
The World Health Organization (2021) stresses the importance of understanding mental health as not just the absence of mental illness, but as a concept that applies to everyone under a range of circumstances. The World Health Organization [WHO] defines mental health as a state of well-being in which the individual realizes their own abilities, can cope with regular stresses of life, can work productively, and is able to make a contribution to their community (2021). The Canadian Mental Health Association [CMHA] describes mental illness as a disturbance in thoughts, feelings, and perceptions that is severe enough to affect everyday functioning. Some examples of mental illnesses are anxiety disorders, schizophrenia, and mood disorders such as major depressive disorder and bipolar disorder. Substance misuse is often linked to poor mental health or mental illness (CMHA, 2021). Internationally, and in most jurisdictions across Canada, supports and services are often offered to address both mental health- and addictions-related issues. In the literature, and in practice, mental illness is sometimes referred to as: mental conditions, mental health issues, mental health difficulties, psychological disorders, and challenges to mental health (Baxter et al., 2022; Chen et al., 2020; Lister et al., 2021).
The Mental Health Continuum Model
Within mental health service delivery, the mental health continuum [MHC] model refers to a specific model that has been developed to help with understanding mental health that incorporates a self-help tool. This model is used to:
- Identify the underlying causes of impairment in daily-life functioning;
- Gather information about mental health of individuals over time;
- Indicate when it would be ideal to seek professional assistance for restoring balance in mental health; and
- Learn how to recognize symptoms of psychological disorders (Chowdhury, 2021).
Originally developed by the Canadian Armed Forces [CAF], the MHC model describes four main states of mental health a person could possibly experience. The model is presented as a continuum, which means that a person can move back and forth along the continuum scale and can also land somewhere between the four main areas at any given time (Chen et al., 2020; NSCAD, 2021).
Figure 1
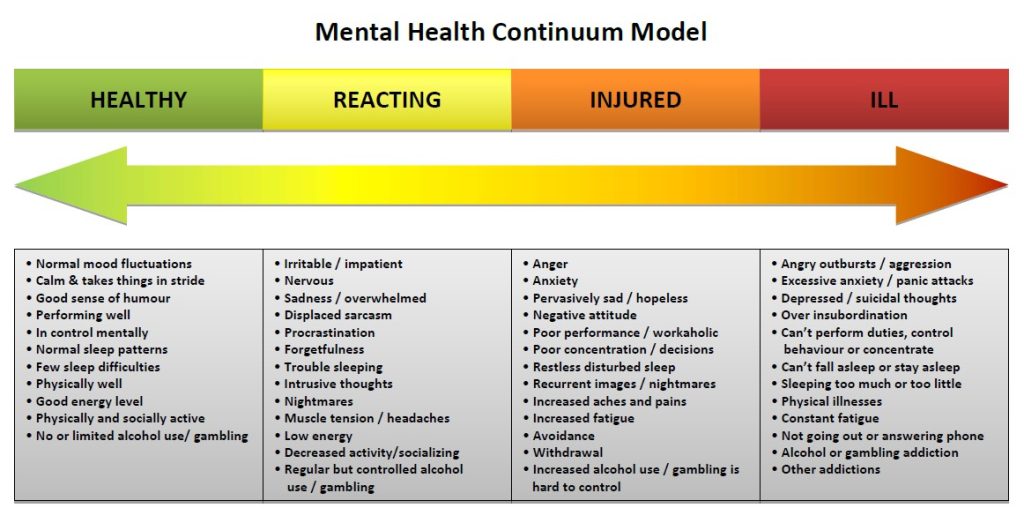
In a more general sense, the mental health continuum refers to a range of mental wellbeing with mental health and mental illness at the two extreme ends. Depending upon the circumstances of an individual at any given point in time, he/she/they can be situated at one point of the continuum but can actually shift position as their situation improves or deteriorates, which is seen as being an effective way to interpret mental health (Allport, 1937; Chen et al., 2020). Consistent throughout the literature is the acknowledgement that there is a place for everyone on the mental health continuum (Chen et al., 2020; Chowdhury, 2021), and that this approach can potentially reduce stigma due to the idea that everyone fits in. The model is intended to serve as a self-reflection and self-monitoring tool, with colours indicating the level of severity of illness. By incorporating colours, the intention is to further reduce stigma by limiting use of jargon and reducing the potential impact of diagnostic labels (Chen et al., 2020). The MHC model has been adopted widely as a tool to promote mental health in various settings and contexts in Canada and internationally (Chen et al., 2020; Franken et al., 2018). The mental health continuum short form [MHC-SF] has been validated in nonclinical samples and incorporated in various countries and cultures (Franken et al., 2018).
Social Workers and the Mental Health Continuum Model
An approach to practice that incorporates the MHC model can be helpful for social workers, regardless of practice setting. However, especially in rural, remote, and northern communities, this model can help social work practitioners to recognize specific behavioral patterns in clients that may need attention and allow them to suggest ways of dealing with service needs in creative ways. Creative approaches and out-of-the-box thinking can be helpful in settings that lack a comprehensive range of formal mental health supports.
For practicing social workers, this model can also offer helpful information to consider as they strive to maintain their own mental health and wellness by serving as a practical and reliable tool for social workers to identify their own sources of personal and professional stress by:
- Understanding how to identify symptoms of mental illness in oneself and others;
- Encouraging the growth and maintenance of a healthy mindset that can assist in overcoming distress and create positive movement on the continuum; and
- Learning how to deal with psychological and emotional crises effectively while not allowing one’s well-being to be jeopardized (Chowdhury, 2021).
Generalist Social Work Practice in Mental Health Service Delivery
Undergraduate social work programs across Canada and North America focus on a generalist approach to social work practice (Weshues et al., 2001). This approach equips social workers with information on the basic concepts in social work, as well as a range of skills and a level of awareness that prepares them for a variety of social work roles in a range of settings. By focusing on generalist practice, students are introduced to ideas that include the promotion of well-being and the application of preventative and intervention methods to address social problems at individual (micro), group (mezzo), and community (macro) levels (Weshues et al., 2001). Although these levels are often spoken of as distinct, they actually occur in tandem and are linked to, and constantly influence, one another.
Rural, remote and northern locations offer unique opportunities for practicing social workers. In fact, many new social workers seek employment in these settings in order to gain practical experience in a relatively short period of time (Schmidt, 2008). Social workers in urban settings will tend to work in areas of practice considered to be more focused and specialized, whereas settings outside of urban areas require the social worker to engage in a number of areas of practice simultaneously. These areas of practice may include child protection services, addictions, mental health, income support, community development, and policy.
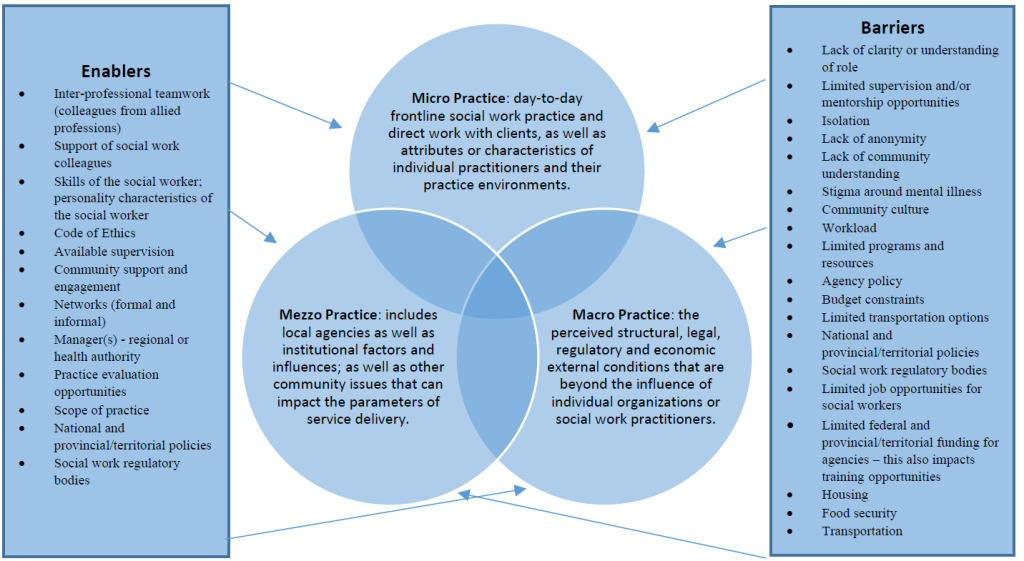
Mental Health Enablers and Barriers outside of Urban Settings
As discussed previously in this book, individuals who live outside of urban centres face unique factors that impact directly upon everyday life. While the quality of life in rural, remote and northern communities is idyllic in many ways, and is often sought after, the challenges associated with living outside of large centres can also affect that quality of life in negative ways – especially in relation to mental health. These negative effects include:
- Less comprehensive, available, and accessible support services,
- Transportation limitations due to geographic accessibility,
- Fragmented continuity of care,
- Difficulties with workforce recruitment and retention,
- Lack of access to affordable housing, and
- Limited access to population-based funding (CMHA Ontario, 2009).
In this context, a barrier to access is understood as any process or intervention by which access to mental health supports is impeded. Enablers are defined as any process or intervention by which access to mental health services and wellbeing is facilitated (Baxter et al., 2022; Lister et al., 2021). Figure 2 provides an overview of enablers and barriers to accessing mental health supports in rural, remote, and northern communities.
Figure 2
Enablers and Barriers to Mental Health Support Availability outside of Urban Settings
Rural, remote, and northern communities are not homogenous. The populations of people who live in these communities are diverse and represent distinct cultures, ethnicities, ages, and backgrounds. Despite this diversity, most individuals seeking supports and services for mental illness experience widespread stigma regardless of their backgrounds (Friesen, 2019; MacLeod et al., 2022).
Mental Health Issues and Stigma
The concept of stigma has been well-researched over the past 6 decades and has led to the conceptualization of stigma as a social construct. Dudley (2000) defined stigma as “stereotypes or negative views attributed to a person or groups of people when their characteristics or behaviors are viewed as different from, or inferior to, societal norms” (p. 449). These views may focus on what are seen to be mental, physical, or social deficiencies (CMHA Ontario, 2022). Stigma differs from discrimination, which is viewed as unfair treatment due to a person’s identity. This identity can include race, ancestry, place of origin, colour, ethnic origin, citizenship, creed, sex, sexual orientation, gender identity, gender expression, age, marital status, family status or disability, including mental disorder (CMHA Ontario, 2022). In other words, stigma is the negative stereotype, and discrimination is the behaviour that results from this negative stereotype.
It is important to note that, because stigma is a social construct, it changes over time. What was stigmatized in the past may not be stigmatized today, or has changed in terms of how it is expressed at the micro-, mezzo- and macro-levels. This change often will occur as a shifting between the three levels. Goffman (1963) referred to this as the “process of devaluation” (p. 3), which can dehumanize anything or anyone that sits outside the lines of what the community believes to be acceptable. This process can create an “us versus them” scenario that is founded in difference, stereotypes, and misinformation; it can result in fear leading to unfair treatment of individuals. In a rural or remote community, this discrimination can be devastating, as an already small social network can become yet smaller, or even non-existent.
Stigma related to mental illness and mental health issues can have detrimental consequences. The World Health Organization [WHO] (2001) has suggested that stigma is one of the largest barriers to mental illness treatment engagement, despite the fact that treatment has been shown to be effective. Due to stigmatization, people may delay seeking help, may exit treatment prematurely, or may completely avoid seeking services. These realities will often increase psychological distress and when individuals can no longer wait due to an increase in symptoms, the level of distress is significantly greater. Stigma can impact social activities for individuals experiencing mental illness, along with education, housing, and employment; the result is often social isolation. Herek (2002) stated: “stigma and discrimination are the enemies of public health” (p. 604). Stigma in the rural and remote areas of Canada can be further compromised by a shortage of services in the areas of mental health and addictions, and difficulty in accessing those services. Stigma at the micro-, mezzo- and macro-levels, in conjunction with a lack of formal supports, can leave people in a very precarious position.
Social workers work with a variety of complex cases that require a thoughtful approach. Working in rural and remote areas with under-served populations requires the social worker to have a sophisticated level of knowledge and understanding of mental health and mental illness, as well as ethical fortitude. Further, a knowledge base of the current and historical culture of the geographic region in which they are practicing is critically important. No two communities are the same and each will have distinct enablers and protective factors, as well as specific barriers and factors that may put people at greater risk. An insular community may have a variety of protective and enabling factors, but someone who is marginalized within that community may also feel like an outsider. This experience will undoubtedly affect that individual’s mental health. Social workers working in rural and remote communities have a unique opportunity to influence efforts to de-stigmatize mental illness. They will work with individuals and their families and can mitigate stigma at the micro- and mezzo-levels. For example, involving the family will support the individual with mental illness, and help the family to understand conditions impacting mental health; this can re-build the family structure and support system. On a macro-level, the social worker will have opportunities to support educational efforts to de-stigmatize mental illness and advocate for local and regional changes. They can advocate for policy change, and ensure that mental health policy is being developed at the same time and rate as health policy. Through the nature of their generalist practice approaches, social workers will also be networking with various agencies and can be an agent of change to support community-wide mental health and wellness initiatives.
A social worker working in mental health services requires the ability to self-reflect about their own stereotypes, beliefs and prejudices. It is also important to acknowledge that we, the community in which we serve, as well as the person in need; all have known and unknown attitudes about what they are coming to discuss. We must create a space where these attitudes and beliefs can be explored and tested, in order to determine their impact on services.
Areas of Practice in Mental Health Services
As discussed throughout this book, a social worker engaging in practice outside of urban settings will have many opportunities to work with a range of individuals from diverse backgrounds. These individuals will seek support services from social workers in order to deal with many aspects of mental health and mental illness. This section will focus on five select areas of social work practice specific to mental health in rural and remote settings: suicide prevention and intervention, substance use and addictions, chronic mental illness, maternal mental health, and violence.
Suicide Prevention and Intervention
In Canada, suicide is identified as the ninth leading cause of death among the general population. However, for individuals between the ages of 15 and 34, suicide is the second leading cause of death (MHCC, 2022b). In first world countries, men are three times more likely than women to die by suicide (WHO, 2017). Lesbian, gay, bisexual, transgender, queer/questioning and other sexual and gender minority (2SLGBTQ+) youth have also been consistently identified as having an elevated risk for suicide (Wang et al., 2021).
The Mental Health Commission of Canada (2022b) reports that alcohol abuse is the second most common mental health problem identified in people who die by suicide, and one in four deaths by suicide are completed by those who abused alcohol. Suicide rates are also higher in rural areas as compared to urban areas (Creighton et al., 2017; Frederick, 2020; Reccord et al., 2021). The rates of suicide in Canada are consistent with suicide rates in other first world countries that experience similarities in terms of poverty levels, aging populations, lack of employment opportunities, and out-migration to urban centres (Cleary, 2012).
Suicide has had a profound impact on communities that are predominantly First Nations, Métis and Inuit. In fact, the suicide rates among First Nations and Métis adults have been reported to be twice as high as among non-Indigenous adults (Park et al., 2015). The rates of suicide in Northern Saskatchewan are very high, and suicide is identified as the leading cause of death for people aged between 10 years to 40 years (Irvine & Quinn, 2017). Suicide intervention approaches need to be culturally responsive in areas that have a higher First Nation, Métis and Inuit population; where the impacts of colonization and inter-generational trauma are the predominant underlying factors impacting suicide rates.
Suicide prevention strategies should be targeted to the local demographics and culture in rural and remote communities, and designed by local stakeholders with a focus on community needs and assets. Social workers can play an important role in suicide prevention, education, and intervention.
Suicide in in rural and remote areas is of significant concern, yet populations impacted by suicide continue to be overlooked and underserved at all three levels of intervention (micro, mezzo, and macro). A review of the literature by Hirsch and Cukrowicz (2014) identified that successful interventions require a thoughtful approach which focuses on the geographic location, social belief systems, and determinants of health that impact suicide. It is also important to recognize the effects of poverty and lack of employment opportunities, as well as the importance of creating literacy around mental wellness and building trauma-informed communities.
As social workers, we have to pay attention to social, cultural, and economic-specific strengths and adversities of communities, as well as social and cultural norms. Every rural or remote community will have its own nuances about what is stigmatizing, its own history within Canada, and its own trauma legacy.
Substance Use and Addictions
Addictions can affect anyone. The Canadian Mental Health Association estimates that approximately 21% of the Canadian population (about 6 million people) will meet the criteria for addiction at some point in their lifetime (CMHA, 2022). Alcohol is identified as the most common drug used by Canadians, and those living in rural and remote areas of the country were more likely to report heavy drinking compared to those living in urban areas (CCSA, 2019; Statistics Canada, 2019).
The American Society of Addiction Medicine (2019) defines addiction as “a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences”. The topic of addictions is vast as it includes the abuse of illegal substances, the misuse of legal substances, as well as compulsive behaviors involving gambling, internet/gaming, and sex. As social workers, it is important to be aware of language and how that language is used in this area of practice. In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM-5] (APA, 2021), revisions were made to include Substance-Related and Addictive Disorders with substantive changes to the disorders grouped there, plus changes to the criteria of certain conditions. The DSM-5 explains that the essential feature of a substance use disorder is that it includes a cluster of cognitive, behavioral, and physiological symptoms highlighting that with this disorder, the individual continues using the substance despite significant substance-related problems (APA, 2021). In other words, people with addictions use substances or engage in behaviors that become compulsive and often continue the behaviors despite harmful consequences.
Understanding the complexity of addiction is essential for social workers and those working to support individuals with addictions; Gabor Mate (2011) explains that addiction is more than a disease or human choice, it is a response to human suffering. Using substances may provide the person temporary relief from emotional and physical pain, however it can exacerbate the problem and have harmful impacts on one’s health, relationships, work/responsibilities, finances, and may lead to legal problems.
The misuse of alcohol and drugs is influenced by individual, cultural and social factors which can serve as protective and/or risk factors (enablers and barriers). These factors need to be considered when working with individuals and families as part of preventative programming, intervention/treatments and rehabilitation processes. For social workers working in rural and remote areas with people and communities experiencing addiction, consideration of these factors is essential to the working relationship and change process. First, the rural and remote location must be acknowledged and considered, as these places throughout Canada do not have the same access and availability of services as do urban centres. This can be challenging for individuals and families experiencing concerns with mental health and substance use as it may require additional time and financial resources in order to connect with supports; all which can further complicate one’s physical, social and mental wellbeing.
Telehealth services and online programming are often options that can be beneficial for individuals and families living in rural and remote communities, as these options create possibilities for people to connect with informal and formal supports in order to address physical health concerns, as well as mental health concerns. An example of services being utilized in this way can be found in remotely delivered Alcoholics Anonymous or Narcotics Anonymous group meetings. Online meetings allow people more options to attend virtual gatherings that support their schedule, can reduce the need to travel long distances, and also can provide greater anonymity. Although this modality of service may increase accessibility for some, it is not always possible for others as this approach requires internet access, computer literacy skills and a safe and quiet space to connect. Understanding how these factors can be barriers is essential to the helping process.
Individuals misusing substances can be at different stages in their use and readiness for change. A harm reduction approach includes strategies to reduce individual harm through managed consumption and overdose prevention sites. This approach, which was initially developed in the 1980s, recognizes the individual and meets them “where they are at” to help reduce harm, address basic needs, and increase safety and wellness. This approach to service delivery also increases engagement of clients, and supports willingness to change. Harm reduction and social work share common values and approaches, not the least of which is recognizing the client (service-user) as expert, and using strengths-based efforts to build collaborative working alliances (Vakharia & Little, 2017).
Navigating the system to help support individuals with substance use disorders can be especially challenging in rural and remote locations, due to limited outpatient and inpatient services and waitlists. It is important for social workers to understand how social and health determinants contribute to risk, to the treatment of substance misuse, as well as overall wellbeing.
As discussed earlier, individuals living in rural and northern locations report high levels of excessive use of alcohol. Higher rates of driving while impaired is also common. In recent years, opioid use has emerged as a crisis across Canada, and this issue is especially difficult to address in rural and northern communities. These two types of addictions will be discussed further below, as will the issue of impaired driving.
Alcohol
Accessibility and availability of resources for alcohol abuse prevention, intervention and recovery are influenced by social and cultural factors. Poor socio-economic conditions found in many rural communities is correlated with higher levels of alcohol consumption, psychosocial stress, and decreased physical activity and preventive service use (Smith et al., 2019). The limited resources available create an additional challenge when trying to arrange services that are appropriate and meet the individual’s needs. Rural physicians show an awareness and concern for alcohol consumption in their communities, but they also report difficulties in accessing resources to refer patients for substance use treatment (Slaunwhite & MacDonald, 2015).
Communities with smaller populations and/or communities that are located in isolated areas can create more familiarity for individuals. This factor can be understood as both an enabler and as a barrier when it comes to seeking support services. Familiarity may bring people a sense of belonging and support, yet it can also be isolating for those who don’t fit the identified community norms and expectations. The lack of anonymity can prevent individuals and families from seeking help due to shame and stigma. Stigma continues to be a factor that potentially isolates people experiencing difficulties with substance use.
It may be helpful for social workers to consider a social-ecological perspective for explaining influences on alcohol use. Individual-level factors that influence alcohol use are found within home, work, and school environments, which are located within the larger community. Macro-level factors, such as exposure to advertising, may influence family and peer network attitudes and norms, which ultimately impact individual attitudes and behaviors. Social work focuses on the person within their environment and recognizes the importance of family, community, culture, legal, social, spiritual, and economic influences that impact well-being of individuals, families, groups, and communities.
Opioids
There is an opioid crisis affecting communities across Canada (Pijl et al., 2022). This crisis is affecting individuals, families, and communities, often resulting in long term health issues like HIV and hepatitis, possible overdose, and death.
Jones and Quinn (2021) illustrate the impact of remote geography on clinical decisions, adequate medication supply, and the importance of engaging pharmacy and nursing colleagues in delivering addictions care specific to the use of opioids. National practice guidelines for opioid use disorder recommend buprenorphine–naloxone as a first‑line treatment. In rural areas, medications that can be administered on a monthly basis, like buprenorphine and/or naltrexone formulations, might be particularly effective since distance and transportation can present barriers to daily-dose treatment approaches (NIDA, 2021). Clinical practice guidelines state that methadone maintenance therapy (MMT) is the standard of care for treating patients with opioid dependence. Methadone maintenance therapy is a substitution/maintenance treatment model whereby methadone is administered in a structured treatment environment to reduce or eliminate the uncontrolled use of illicit opioids (NIDA, 2021).
Impaired Driving
Research has shown that rates of impaired driving tend to be about twice as high in rural areas as compared to urban areas (Perreault, 2019). For the purpose of this discussion, impaired driving refers to driving while under the influence of alcohol, cannabis, or other mind-altering substances. Greene et al. (2018) found that these rates were often higher in younger age groups and identified specific factors that contribute to those higher rates: social context (peer pressure and parental modeling), rural cultural values (independence, stoicism, and social cohesion), as well as the realities of the legal and physical environment (minimal police presence, sparse population, and no alternative transportation). Since 2018 when Canada became the second country to legalize non-medical cannabis, emerging research has confirmed that driving under the influence of cannabis is an increasingly prevalent road safety issue (Brands et al., 2021). As discussed earlier, higher rates of cannabis and alcohol use are also linked to increased suicidal ideation in young people. Suicidal ideation, or suicidal thoughts, means having thoughts or ideas about the possibility of ending one’s own life.
Social workers practicing outside of large urban centres play a key role in working with individuals with substance use and co-occurring disorders, as well as their families and communities. As such, knowledge about substances, behavioral indicators of substance use, relevant assessment tools, and knowledge about available and accessible treatment and support options is essential.
Chronic Mental Illness
Long-term and chronic mental illness is multi-faceted and complex, requiring a coordination of support and collaboration at all three levels of social work practice (micro, mezzo and macro) beginning when the individual seeks ongoing support, and continuing as they enter into the recovery and long-term support process. Most often in the literature, those with chronic mental illness are identified as individuals with Serious Mental Illness (SMI) (Steele et al., 2014), and this is the term that will be used in this discussion. Individuals with SMI fall at the extreme right side of the mental health continuum and may require a greater level of tertiary care in order to stabilize their mental illness and avoid further deterioration. Those with SMI usually require long-term medication and support, and this can include schizophrenia and schizophrenic‐like disorders, but can also refer to any reoccurring mental illness that produces serious functional impairment and interferes with the person’s quality of life including psychosis and bipolar disorders (Steele et al., 2014). Individuals with SMI typically experience gaps in services and these gaps are more pronounced in rural and remote locations that lack community resources and in-patient capacity.
Individuals with SMI tend to socially isolate themselves and this can have compounding effects on the course of their recovery. A supportive and resourced community can have significant and positive influence on the lives of people living with SMI. Protective factors increase when the social capital of the community is more robust. Social capital includes friends, social norms, networks of support and employment opportunities for the individual with Serious Mental Illness in the community (Dykxhoorn et al., 2019), and can play an important role in the person’s overall mental health and physical wellbeing. Social capital also includes the infrastructure of a community such as parks, libraries and other pro-social activities like volunteering opportunities. In their research, Kitchen et al. (2012) found a very strong association between health (mental health in particular) and a sense of belonging, especially in rural areas of Canada.
Peer support can have a positive impact on the person with SMI, as well as the family who may struggle with their own perceptions of mental illness. Peer support can include group activities, mentoring, and a system of mutual giving and receiving where individuals with SMI can offer hope, companionship, and encouragement to others facing similar challenges (Naslund et al., 2014). Peer support lays primarily in the mezzo-level of support provided by social workers, and can have a significant impact on the micro-level as the social capital increases and the person’s sense of inclusion and community belonging also increase. Individuals with SMI often turn to social media to seek information and create communities to share their experience, and to obtain information from others with a similar diagnosis. This network building can significantly reduce personal and social stigma and normalize experiences as they increase insight about their diagnosis, develop on online community where potentially none exists in their home community, and gain support from others in similar circumstances including gender, age, culture and other demographics that may be important to the individual. However, vulnerability is a potential risk that needs to be considered when entering the online platform.
Individuals with Serious Mental Illness represent 30% to 40% of the homeless population and as many as 25% of those same individuals have a substance dependence (Kirby & Keon, 2006). Although rural and remote homelessness in Canada remains a hidden issue, there is mounting evidence that homelessness is as prevalent in rural communities as it is in urban settings (NAERRH, 2021). As the individual with SMI moves between recovery and maintenance, the importance of housing in the stabilization of psychiatric symptoms is highlighted as a significant factor in their recovery. Stable housing is especially important for social workers to keep in mind when working in rural and remote locations where the interplay between the mezzo- and macro-levels can have a significant impact on the quality of life of the individual. This issue highlights the importance of developing a coordinated and collaborative approach encompassing all three levels of support and intervention (micro, mezzo, and macro). Social workers can provide individual support, as well as sessions for couples and families. The role of social workers in working with individuals with SMI also includes conducting psychosocial, cognitive and mental health assessments, and working as part of an interdisciplinary team to develop and support individualized treatment plans. As social workers, our work helps to reduce stigma and promote evidence-based treatment for all persons in need of support. This support may include advocacy work at the mezzo- and macro-levels to address some of the basic human needs of individuals with SMI at the municipal, provincial, and federal levels.
Maternal Mental Health
Having a baby can be an exciting and life affirming experience; however, this is not the experience of all families. The perinatal period is often an overwhelming, stressful and anxiety-inducing time that can affect every aspect of life for the woman, partner and family unit. As a social worker, working in rural and remote locations with families during the perinatal period is recognized as practice that is potentially impacted by great risk, as well as opportunity for the greatest outcomes.
In Canada, one family experiencing PMADs (Perinatal mood and anxiety disorders) is estimated to cost the healthcare system over $150,000. However, by utilizing a simple screening tool and providing access to treatment, the cost is estimated at $5000 (Bauer et al., 2014). As social workers, we also consider the hidden costs that include the impact on the child, mother, family and community. Suicide is the leading cause of death during the perinatal period for women (Bauer et al., 2014; Grigoriadis et al., 2017).
Maternal mental health is defined as “a state of well-being in which a mother realizes her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her community” (McCauley et al., 2019, p. 2). The term perinatal refers to the period of conception up to and including 12 months after a birth. Perinatal mood and anxiety disorders (PMADs) refer to a variety of mental health issues that fall within the mental health continuum. They include Depression, Bipolar Disorder, Anxiety, Panic Disorder and Obsessive-Compulsive Disorder. In extreme situations, Psychosis can also be included, but this would be classified as a rare medical emergency.
Understanding perinatal mood and anxiety disorders (PMADs) and their origins is as complicated and unique as is the woman and family unit. As a social worker working with new or expecting families, you need to familiarize yourself with the signs and symptoms of PMADs. Risk factors increase or decrease depending on a number of factors that may include social, psychological, environmental, and hormonal issues. Families that are marginalized and experience lower socio-economic status, food insecurity, family violence, adverse life experiences, historical trauma, and are 2SLGBTQ+, are at increased risk of developing PMADs. First Nations women are 20% more likely to have post-partum depression than Caucasian women (Dharma et al., 2019). It’s important to note that not all families who share these particular factors are destined to have PMADs. However, every family is at risk of developing PMADs; for instance, even fathers/partners may experience symptoms of depression after the birth of the baby at a rate of 10% (Paulson & Bazemore, 2010).
The short- and long-term consequences of untreated perinatal mood and anxiety disorders (PMADs) can be detrimental to the woman, baby, family and community. Depression and anxiety can present distinctly for each woman, though some common features include feelings of sadness, lethargy, anger and worry. These are unlike “baby blues” that are shorter in duration and lack physical and emotional intensity. Other outcomes include impact on the partner relationship, attachment issues, as well as social, emotional and cognitive development in the baby (Letourneau et al. 2012).
When reviewing how Canada is doing with respect to maternal mental health (Hippman et al., 2022), research identified numerous gaps and regional differences, and advocates for a national perinatal mental health strategy that would target prevention and triaging into treatment and support. From a social work perspective, this advocacy work is best coordinated at all three service levels (micro, mezzo, and macro).
Parents residing in rural and remote locations are often burdened with travel costs and face the reality of having to leave their other children behind to be tended to by members of the community when they have to access labor and delivery services in larger urban centres. Some rural and remote locations may have a health centre, but due to physician shortages and the lack of locum doctors, families may be directed to another community to access care. Parents experiencing high risk pregnancies are usually directed to leave their home community at 38 weeks gestation or earlier, which can create financial barriers requiring travel and a hotel stay; the parent would then also be in an unfamiliar community without any informal supports (family and friends) to rely upon.
Building maternal mental health capacity in rural and remote locations requires a multi-faceted approach that considers the local culture, community strengths, and opportunities for development. Many remote communities have a long history of childbirth and mental wellness, and each geographic area will have its own ceremonies, traditions and protocols that honour the significance of taking care of the family in a holistic manner. The use and training of doulas and midwives who are connected to the community would be an example of building capacity at the community level, as would training of maternal mental health providers (including social workers) in a manner that is respectful of the traditions and culture of the region. Key social work competencies when working with families during the perinatal period include:
- Treating the family with respect, and honouring their specific cultural needs and requests;
- Providing education on positive mental health and appropriate screening tools;
- Sharing knowledge of both formal and informal supports available in the community to support the family unit; and
- Enhancing the attachment between baby and caregivers.
Violence
Social workers engage with vulnerable populations that are experiencing various challenges, and this includes working with survivors and perpetrators of violence. Regardless of the geographic setting, violence is a multifaceted issue and it has detrimental effects on the individual, family and community. In providing mental health supports, prevention initiatives and intervention services must consider individual, community, and societal factors and how they affect individuals and families experiencing violence. Social workers work collaboratively to initiate life-changing interventions and support mental health on a daily basis, and in rural and remote communities there is always the potential for social workers to find themselves alone in a dangerous situation during such interventions.
The World Health Organization Violence Prevention Alliance divides violence into three sub-types according to the victim-perpetrator relationship: self-directed violence (suicide, suicide attempts and self-abuse), interpersonal violence (youth violence, intimate partner violence, sexual violence, gender-based violence, child maltreatment, and elder abuse), and collective violence (violence committed by larger groups of individuals and can be subdivided into social, political and economic violence) (WHO, 2010). The World Health Organization (2010) also states that violence represents a “major health, criminal justice, human rights, and development challenge” (p. 2). It over-burdens health and mental health systems, undermines communities, and slows economic and social development (WHO, 2010).
Regardless of the type of violence that is impacting communities and mental health, social workers need to be familiar with risk assessment, risk management and safety planning. Conducting a thorough risk assessment of every client is critical, and should always include efforts to determine a prior history of violence, mental illness or other mental health-related challenges, drug and alcohol use, and weapon use. There is no doubt that information and knowledge is powerful when trying to prevent violence, and to mitigate the effects of violence.
When working in remote and rural areas, it is important to build relationships and understand the uniqueness of the community. This includes building knowledge of available resources and programs to support good mental health, and understanding cultural norms that can serve as risk factors or protective factors. Rural and remote communities do not have access to the same formal mental health supports and services as do urban centres.
Geographic isolation can contribute to barriers for those seeking services, such as a lack of transportation and limited access to appropriate resources. Other challenges for individuals who have experienced mental illness, addictions, and violence living in rural and remote areas include greater distances between homes, being less visible to neighbors or other potential witnesses, and being further away from emergency services. In many rural and remote areas there are an abundance of weapons, as well as situations where the justice system allows the return of weapons for hunting season to those charged and convicted with violent offences. Access to e-mail and the Internet, as well as adequate and consistent cell phone coverage, is not available in many areas outside of large urban centres (Kasdorff & Erb, 2010).
Rural communities have unique resources and capacities for mental health resilience such as a tightly knit network of support and a strong relationship to the natural environment (Hirsch & Cukrowicz, 2014). These can be protective factors when one fits in, and they can create a sense of belonging within close, tight-knit communities. However, these same unique resources and capacities can also contribute to a heightened risk of conflict and violence.
As a social worker delivering mental health services in areas outside of large urban centres, you will need to take proactive steps to mitigate violent encounters. First, all practicing social workers must have adequate and responsible supervision and support from a supervisor. This supervision should support ethical considerations and best practice, while instilling a culture of safety and risk reduction. Secondly, social workers should have access to relevant safety training and technology, including GPS tracking. In recent years, there have emerged a number of innovations in mental health service delivery that have the potential to be particularly helpful in rural, remote, and northern environments by creating safe options for clients and social workers outside of large urban settings.
Innovations in Mental Health Service Delivery
Telehealth is an innovation that originally emerged to help bridge the distance for residents living in rural and remote areas in order to access health care. Telehealth is defined as the use of digital information and communication technologies, such as computers and mobile devices, to access personal health care services remotely (Mayo Clinic, 2022). More specific to mental health interventions, telepsychiatry facilitates staff education and specialty consultation; reduces rural practitioners’ sense of isolation; better protects patient anonymity, potentially reduces stigma; generates reliable diagnoses; and yields high patient and provider satisfaction (Hubley et al., 2016).
In addition to more traditional telepsychiatry services, there are other options that have emerged in response to limited accessibility and resources such as telephone helplines, telephone counselling, video counselling, Internet Cognitive Behavioral Therapy (ICBT), walk-in (rapid access) counselling services, mobile apps, and other digital health platforms. The next sections will focus on mobile apps and digital health platforms, as well as walk-in counselling (rapid access) service options.
Mobile Apps and Digital Mental Health Platforms
Mental wellness/health apps and digital mental health platforms have continued to increase in popularity, and are seeing further development and growth as users download them with the hopes of managing and addressing mental health challenges and mental illness such as anxiety and depression (Marshall et al., 2020). Increasingly, governments and service providers are endorsing these options as viable alternatives to face-to-face support due to low cost, convenience, and accessibility (Parker et al., 2019). A number of treatment approaches including cognitive behaviour therapy (CBT), dialectical behaviour therapy (DBT), and prolonged exposure therapy are being assimilated into apps that can stand alone or supplement the face-to-face therapy process (East & Havard 2015).
Mental health apps and digital platforms have the potential to reach people who would otherwise not receive help by removing the barriers to access. These apps and digital platforms may reduce cost, eliminate wait-times, and may also reduce the stigma that can exist for those receiving support for mental health challenges. These support options can promote user autonomy by facilitating self-awareness and self-efficacy, which fits within the realm of social work values. For those outside of large urban centres, mental health apps may also be applied for real-time monitoring of users who are in crisis without available in-person supports (Robillard et al., 2019). Barriers to accessibility of mental health apps and digital platforms, however, exist due to connectivity issues in rural and remote locations, computer and technological literacy issues, as well as costs associated with the purchase of cell phones and computers. There is also a cost associated with accessing the apps themselves.
A lack of privacy can also pose challenges for some who do not have a private place to talk due to others in the home and/or concerns around safety. For some individuals, seeking help can risk their safety and wellbeing. As a result, there are some mental health websites and apps that have a quick exit feature to increase safety for people at risk of, or are experiencing, violence.
Finally, because there are no regulations nor standards in place for mental health apps and digital platforms, they may provide inaccurate information and resources and services that are not evidence-based; which poses ethical concerns from a social work perspective. However, these options continue to be developed and made widely available. The research and literature regarding efficacy of these approaches to support mental health and wellness is limited, but data suggests that this technology is being well-utilized by subscribed users (Marshall et al., 2020; Robillard et al., 2019).
Walk in Counselling (Rapid Access)
Walk in counselling clinics have been operating throughout Canada for over 25 years, and this approach to service delivery is more established in Canada than anywhere else in the world (Hoyt & Talmon, 2014). The rapid access model of counselling is typically implemented to help reduce barriers for individuals seeking support and as a response to diminishing resources (Harper-Jaques & Foucault, 2014). Within rural and remote communities, few affordable counselling services are often available, which can result in people not receiving help when they are seeking it. Again, this may be due to factors such as lack of transportation, length of travel time, lack of child care and/or the stigma related to seeking help. Walk in counselling services have emerged as a creative means to reduce barriers and offer individuals and families help when they need it.
Conclusion
Accessibility is one of the five pillars of the Canada Health Act (Health Canada, 2015), yet many Canadians continue to experience barriers to accessing the care that they need. This is especially true for individuals living in rural, remote, and northern areas in Canada who are seeking mental health supports and treatment options for mental illness. As service providers living and practicing in these communities outside of large urban centres, social workers are well-positioned to provide information, assessments, interventions and ongoing supports to individuals struggling with mental illness and addictions.
This chapter discussed mental health and mental illness, with a particular emphasis on the mental health continuum [MHC] model as a tool to be utilized by social workers in rural and remote settings. An exploration of enablers and barriers to accessing mental health supports was provided, and select mental health issues and challenges that social workers address in rural and remote settings was examined. In particular, suicide prevention and intervention, substance use and addictions, chronic mental illness, maternal mental health, and violence were discussed.
There continues to be stigma associated with mental illness and for those experiencing issues with their mental health. The Mental Health Commission of Canada reports that one in every five Canadians experiences a challenge to their mental health within a given year (MHCC, 2022a). While we often have a good understanding of physical illness, there tends to be less knowledge available about mental illness or substance use issues. As discussed in this chapter, a lack of understanding leads to fear and negative attitudes towards individuals living with mental illness and addictions, and it prevents people from seeking help for themselves and from providing appropriate support to people around them. These issues are even more apparent in rural and remote communities.
Just as social workers provide information, supports, and care to those in rural and remote communities who struggle with challenges to their mental health; social workers who practice in rural and remote settings must also work to maintain their own mental health and wellness. Having the support of colleagues and supervisors can be essential to avoiding burnout for any social worker. However, social workers practicing outside of large urban centres often do not find those connections easy to build. As a result, they must create supportive networks with allied professionals and social workers in different regions in order to access the feedback and collaboration that is needed for their own mental health and wellness. Maintaining good mental health is essential for good social work practice.
Activities and Assignments
- Think about the various stereotypes that you have heard about people experiencing mental illness over your lifetime. Have those stereotypes changed over the years? Which of those stereotypes do you believe are still prevalent for you, or for your family, or in your community? How might these stereotypes affect you as a social worker supporting individuals and families living with mental illness in rural or remote communities?
- What are some of the barriers that individuals seeking help in order to address suicidal thoughts in rural and remote locations might encounter? What are some of the enablers that might support a suicidal individual in seeking mental health support?
- Online peer support can be beneficial for the person with serious mental illness (SMI) living outside of an urban centre. As the social worker supporting this individual utilizing online peer support, what factors would you need to consider to mitigate potential risk to the individual?
- Identify a rural or northern community that you are familiar with, and list the services that are available there to support maternal mental health. What barriers to good mental health for a family with a newborn might be present in that same community?
Additional Resources
- Mental Health Commission of Canada [MHCC]. (2021). Answering the call: Strategic plan 2021/2030. Available on the Mental Health Commission of Canada website.
References
Allport, G.W. (1937). Personality: A psychological interpretation. Holt.
American Psychiatric Association [APA]. (2021). Diagnostic and statistical manual of mental disorders (DSM-5), fifth edition. Author.
American Society of Addiction Medicine. (2019). Definition of addiction. https://www.asam.org/quality-care/definition-of-addiction
Baxter, L., Burton, A., & Fancourt, D. (2022). Community and cultural engagement for people with lived experience of mental health conditions: What are the barriers and enablers? BMC Psychology, 10(71).
Bauer, A., Parsonage, M., Knapp, M., Iemmi, V., & Adelaja, B. (2014). The costs of perinatal mental health problems. Centre for Mental Health and London School of Economics.
Brands, B., Di Ciano, P., & Mann, R.E. (2021). Cannabis, impaired driving and road safety: An overview of key questions and issues. Frontiers in Psychiatry, 12, 641549.
Canadian Association of Social Workers [CASW]. (n.d.). The role of social work in mental health.
Canadian Centre on Substance Use and Addiction [CCSA]. (2019). Canadian drug summary: Summer 2019. Author. ISBN 978-1-77178-583-9
Canadian Mental Health Association [CMHA]. (2021). Mental health and mental illness: What’s the difference? https://cmha.ca/brochure/fast-facts-about-mental-illness/
Canadian Mental Health Association [CMHA] Ontario. (2009). Backgrounder: Rural and northern community issues in mental health. https://ontario.cmha.ca/wp-content/uploads/2009/09/cmha_on_rural_northern_mental_health_issues_20090827.pdf
Canadian Mental Health Association [CMHA] Ontario. (2022). Stigma and discrimination. https://ontario.cmha.ca/documents/stigma-and-discrimination/
Chen, S.P., Chang, W.P., & Stuart, H. (2020). Self-reflection and screening mental health on Canadian campuses: Validation of the mental health continuum model. BMC Psychology, 8(76).
Chowdhury, M.R. (2021). What is the mental health continuum model? https://positivepsychology.com/mental-health-continuum-model/
Cleary, A. (2012). Suicidal action, emotional expression, and the performance of masculinities. Social Science & Medicine, 74(4), 498-505.
Creighton, G., Oliffe, J., Ogrodniczuk, J., & Frank, B. (2017). “You’ve gotta be that tough crust exterior man”: Depression and suicide in rural-based men. Qualitative Health Research, 27(12), 1882-1891.
Dharma, C., Lefebvre, D.L., Lu, Z., Lou, W., Becker, A.B., Mandhane, P.J., Turvey, S.E., Moraes, T.J., Azad, M.B., Chen, E., Elliott, S.J., Kozyrskyj, A.L., Sears, M.R., & Subbarao, P. (2019). Risk for maternal depressive symptoms and perceived stress by ethnicities in Canada: From pregnancy through the preschool years. Canadian Journal of Psychiatry, 64(3), 190–198.
Dudley, J.R. (2000). Confronting stigma within the services system. Social Work, 45, 449-455.
Dykxhoorn, J., Hollander, A.C., Lewis, G., Dalman, C., & Kirkbride, J.B. (2019). Family networks during migration and risk of non-affective psychosis: A population-based cohort study. Schizophr Res, 208, 268-275.
East, M., & Havard, B. (2015). Mental health mobile apps: From infusion to diffusion in the mental health social system. JMIR Mental Health, 2(1).
Franken, K., Lamers, S.M.A., Ten Klooster, P.M., Bohlmeijer, E.T., & Westerhof, G.J. (2018). Validation of the Mental Health Continuum-Short Form and the dual continua model of well-being and psychopathology in an adult mental health setting. Journal of Clinical Psychology, 74, 2187–2202.
Frederick, L. (2020). Barriers to help-seeking in men for mental health issues: The impact of gender role socialization and masculine ideologies. [Master’s thesis, The City University of Seattle]. Digital Archive.
Friesen, E. (2019). The landscape of mental health services in rural Canada. UTMJ, 96(2), 47-52.
Goffman E. (1963). Stigma: Notes on the management of spoiled identity. Simon & Schuster.
Greene, K.M., Murphy, S.T., & Rossheim, M.E. (2018). Context and culture: Reasons young adults drink and drive in rural America. Accident Analysis and Prevention, 121, 194-201.
Grigoriadis, S., Wilton, A.S., Kurdyak, P.A., Rhodes, A.E., Vonder Porten E.H., Levitt, A., Cheung, A., & Vigod, S.N. (2017). Perinatal suicide in Ontario, Canada: A 15-year population-based study. CMAJ, 189(34), E1085-E1092.
Harper-Jaques, S., & Foucault, D. (2014). Walk-in single-session therapy: Client satisfaction and clinical outcomes. Journal of Systemic Therapies, 33, 29-49.
Health Canada. (2015). Canada Health Act: Annual Report (2014-2015). HC Pub: 150140.
Herek, G.M. (2002). Thinking about AIDS and stigma: A psychologist’s perspective. The Journal of Law, Medicine & Ethics, 30, 594–607.
Hippman, C.L., Adham, M., Zlobin, C., & Wong, G. (2022). An environmental scan of perinatal mental health infrastructure across Canada. Journal of obstetrics and gynaecology Canada, 44(7), 745-746.
Hirsch, J., & Cukrowicz, K. (2014). Suicide in rural areas: An updated review of the literature. Rural Mental Health, 38(2).
Hoyt, M.F., & Talmon, M. (Eds.). (2014). Capturing the moment: Single session therapy and walk-in services. Crown House Publishing Limited.
Hubley, S., Lynch. S.B., Schneck, C., Thomas, M., & Shore J. (2016). Review of key telepsychiatry outcomes. World J Psychiatry, 6(2), 269-82.
Irvine, J., & Quinn, B., (2017). Northern Saskatchewan health indicators, health status: Mortality. Athabasca Health Authority, Keewatin Yatthé Health Region and Mamawetan Churchill River Health Region. Population Health Unit, La Ronge, SK.
Jones, M.K., & Quinn, M.A. (2021). Buprenorphine–naloxone induction in the north. Can J Rural Med, 26, 35-7.
Kasdorff, D., & Erb, B. (2010). Serving victims of violence in rural communities: Challenges and best practices. Victim/Witness Assistance Program, East Region, Ontario.
Kirby, M.J., & Keon, W.J. (2006). Out of the shadows at last: Transforming mental health, mental illness and addiction services in Canada. Report of the Standing Senate Committee on Social Affairs, Science and Technology, Government of Canada.
Kitchen, P., Williams, A., & Chowhan, J. (2012). Sense of community belonging and health in Canada: A regional analysis. Social Indicators Research, 107, 103-126.
Letourneau, N.L., Dennis, C.L., Benzies, K., Duffett-Leger, L., Stewart, M., Tryphonopoulos, P.D., Este, D., & Watson, W. (2012). Postpartum depression is a family affair: Addressing the impact on mothers, fathers, and children. Issues in Mental Health Nursing, 33(7), 445-457.
Lister, K., Seale, J., & Douce, C. (2021). Mental health in distance learning: A taxonomy of barriers and enablers to student mental wellbeing. The Journal of Open, Distance and e- Learning,
MacLeod, M.L.P., Penz, K.L., Banner, D., Jahner, S., Koren, I., Thomlinson, A., Moffitt, P., & Labreque, M.L. (2022). Mental health nursing practice in rural and remote Canada: Insights from a national survey. International Journal of Mental Health Nursing, 31, 128-141.
Marshall, J.M., Dunstan, D.A., & Bartik, W. (2020). Effectiveness of using mental health mobile apps as digital antidepressants for reducing anxiety and depression: Protocol for a multiple baseline across-individuals design. JMIR Research Protocols, 9(7), e17159.
Mate, G. (2011). Close encounters with addiction. Central Recovery Press.
Mayo Clinic. (2022). Telehealth: Technology meets healthcare. Health Information. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/telehealth/art-20044878
McCauley, M., Brown, A., Ofosu, B., & van den Broek, N. (2019). “I just wish it becomes part of routine care”: Healthcare providers’ knowledge, attitudes and perceptions of screening for maternal mental health during and after pregnancy: A qualitative study. BMC Psychiatry, 19(279), 1-8.
Mental Health Commission of Canada [MHCC]. (2022a). Mental Health First Aid: Program history. https://mentalhealthcommission.ca/training/mhfa/program-history/
Mental Health Commission of Canada [MHCC]. (2022b). How alcohol and suicide are connected – a fact sheet. https://mentalhealthcommission.ca/resource/alcohol-use-and-suicide-fact-sheet/
Naslund, J., Grande, S., Aschbrenner, K., & Elwyn, G. (2014). Naturally occurring peer support through social media: The experiences of individuals with Severe Mental Illness using YouTube. PLoS ONE, 9(10), e110171.
National Alliance to End Rural and Remote Homelessness [NAERRH]. (2021). Rural & remote homelessness: A call for strategic investments in rural and remote communities across Canada.
National Institute on Drug Abuse [NIDA] (2021). Opioid overdose crisis. https://nida.nih.gov/drug-topics/opioids/opioid-overdose-crisis
NSCAD (2021). Peer mentors: Self monitoring with the mental health continuum tool. NS: NSCAD University. https://navigator.nscad.ca/wordpress/wp-content/uploads/2021/10/Mental-Health-Continuum-Tool-PDF-EDIT.pdf
Park, J., Tjepkema, M., Goedhuis, N., & Pennock, J. (2015). Avoidable mortality among First Nations adults in Canada: A cohort analysis. Health Reports, 26(8), 10-6.
Parker, L., Halter, V., Karliychuk, T., & Grundy, Q. (2019). How private is your mental health app data? An empirical study of mental health app privacy policies and practices. International Journal of Law and Psychiatry, 64, 198-204.
Paulson, J., & Bazemore, S. (2010). Prenatal and postnatal depression in fathers’ and its association with mental depression: A meta-analysis. Journal of the American Medical Association, 303(19), 1961-1969.
Perreault, S. (2019). Police-reported crime in rural and urban areas in the Canadian provinces, 2017. Juristat, Canadian Centre for Justice Statistics, 1, 3-37.
Persson, L. Dobson, K.S., & Frampton, N.M.A. (2021). Evaluation of a mental health continuum model in two samples. Canadian Journal of Behavioural Science, 54(3), 206–212.
Pijl, E.M., Alraja, A., Duff, E., Cooke, C., Dash, S., Nayak, N., Lamoureaux, J., Poulin, G., Knight, E., & Fry, B. (2022). Barriers and facilitators to opioid agonist therapy in rural and remote communities in Canada: An integrative review. Substance Abuse Treatment, Prevention, and Policy 17, 62 (2022).
Reccord, C., Power, N., Hatfield, K., Karaivanov, Y., Mulay, S., Wilson, M., & Pollock, N. (2021). Rural–urban differences in suicide mortality: An observational study in Newfoundland and Labrador, Canada. The Canadian Journal of Psychiatry, 1-11.
Robillard, J.M., Feng, T.L., Sporn, A.B., Lai, J., Lo, C., Ta, M., & Nadler, R. (2019). Availability, readability, and content of privacy policies and terms of agreements of mental health apps. Internet Interventions: The Application of Information Technology in Mental and Behavioural Health, 17, 1-8.
Schmidt, G. (2008). Professional work in remote, northern communities: A social work perspective. UNBC Community Development Institute.
Slaunwhite, A.K., & MacDonald, S. (2015). Alcohol, isolation, and access to treatment: Family physician experiences of alcohol consumption and access to health care in rural British Columbia. The Journal of Rural Health, 31(4), 335-345.
Smith, T., McNeil, K., Mitchell, R., Boyle, B., & Ries, N. (2019). A study of macro-, mezzo- and micro- barriers and enablers affecting extended scopes of practice: The case of rural nurse practitioners in Australia. BMC Nursing, 18(14), 1-12.
Statistics Canada. (2019). Health fact sheets: Heavy drinking, 2018. Author.
Steele, L.S., Durbin, A., Lin, E., Victor, J.C., Klein-Geltink, J., & Glazier, R.H. (2014). Primary care reform and service use by people with serious mental illness in Ontario. Healthcare Policy, 10(1), 31- 45.
Vakharia, S.P., & Little, J. (2017). Starting where the client is: Harm reduction guidelines for clinical social work practice. Clinical Social Work Journal, 45, 65–76.
Wang, Y., Feng, Y., Han, M., Duan, Z., Wilson, A., Fish, J., Sun, S., & Chen, R. (2021). Methods of attempted suicide and risk factors in LGBTQ+ youth. Child Abuse & Neglect, 122.
Westhues, A., Lafrance, J., & Schmidt, G. (2001). A SWOT analysis of social work education in Canada, Social Work Education, 20(1), 35-56.
World Health Organization [WHO]. (2021). WHO urges more investments, services for mental health.
World Health Organization [WHO]. (2017). Depression and other common mental disorders: Global health estimates.
World Health Organization [WHO]. (2010). Violence Prevention Alliance: Conceptual framework – November 2010. Geneva, Switzerland.
World Health Organization [WHO] (2001). World Health Report 2001. Mental health: New understanding, new hope. Geneva, Switzerland.

