12 Older Adults in Rural Communities: Policy and Practice
Bonnie Jeffery and Laurie Schmidt
This chapter will discuss the unique situation of older adults living in rural communities and the specific role that generalist social workers play at different levels of practice. Social workers frequently work with older adults in many different roles; this work can include assisting those who are moving from their homes into settings such as long-term care facilities. However, a large proportion of those over the age of 65 continue to live healthy and productive lives in their own homes and communities. It is the latter group that is the primary focus of this chapter, in which we explore what rural social workers can do to support successful aging in place for community-dwelling older adults.
In order to set the context we first present information on the current profile of rural older adults in Canada and particularly in Saskatchewan. We then discuss the concept of ageism which is fundamental to anti-oppressive social work values and practice with this population. This information helps to highlight the important role that social workers play in supporting the needs of this group with a focus on those who live in rural settings. We conclude with a discussion of social work policies and interventions at levels of rural social work practice: practice that is guided by a person-in-environment approach. We highlight the role of a social ecological framework to address the discussion of interventions at micro, mezzo and macro levels of rural social work practice.
Learning Objectives
By the end of this chapter you will have had the opportunity to:
- Understand the unique context and needs of older adults living in rural areas
- Understand how an anti-oppressive and social justice approach contributes to a person-centered approach in rural social work with older adults
- Identify how a social ecological framework that incorporates levels of social work practice supports successful aging for rural older adults
Profile of Older Adults
Canada’s population is undergoing a significant shift that will bring both opportunities and challenges. Canadians 65 years and older now make up 19% of the country’s population (Statistics Canada, 2022a). It is projected that by 2030 older adults will make up 25% of the Canadian population. Older adults make significant contributions to our society and they play an important role in communities, families, and in the workforce. It is important that we understand the needs of older adults in our country and, as the older adult population increases, that we ensure resources and policies will support these needs.
Older Adults in Canada and Saskatchewan
In 2021, 7,021,430 Canadians were aged 65 or older. This represents an 18.3% increase in the population of this age cohort since 2016: the second-largest increase recorded in the past 75 years, following the increase recorded between 2011 and 2016 (Statistics Canada, 2022a). This rate is also higher than Canada’s 5.2% overall population growth rate between 2016 and 2021 (Statistics Canada, 2022b). The 2016 Census was the first time that Canadians aged 65 and older exceeded the number of children under 15 years old. In 2021, there were just over one million more Canadians aged 65 and older than children under 15. The number of children in Canada grew at a rate six times slower than the number of Canadians 65 and older (Statistics Canada, 2022a).
In 2021, 197,985 Saskatchewan residents were 65 or older. Members of this age cohort increased by 16.2% since 2016 (Statistics Canada, 2022c), significantly above the province’s overall population growth rate of 3.1% during that same time period (Saskatchewan Bureau of Statistics, 2022). Residents 65 and older now make up 17.5% of the Saskatchewan population (Statistics Canada, 2022c).
Older Adults in Rural Areas in Canada and Saskatchewan
In 2021, 6.6 million Canadians resided in rural areas, an increase of 0.4% from 2016 (Statistics Canada, 2022d). Population aging in rural Canada is occurring at a faster rate than aging in small and large urban centres. There was a 3.1% increase in the population of residents aged 65 and older in rural areas between 2016 and 2021, while urban areas saw a 1.9% increase in that cohort during that same time period (Statistics Canada, 2022a).
In 2021, 79,128 residents in rural Saskatchewan were aged 65 and older, an increase of 10.9% since 2016. This age group now accounts for 20% of the rural population in the province. While overall the rural population has been decreasing in Saskatchewan since 2015, the number of rural residents aged 65 and older has been increasing since 2011, when older adults made up just 16.8% of rural residents.
In summary, the Canadian population is aging. The number of people age 65 and older has increased steadily since 2011. The rural population in this age cohort have also been increasing since 2011, particularly in Saskatchewan where 20% of the population is 65 and older. An aging population presents numerous opportunities and challenges that need to be managed effectively to ensure the needs of this population are supported, through allocation of resources and implementation of health and social policies. Older adults contribute significantly to their communities, families, and friends. With the growing number of aging adults, particularly in rural communities where resources are limited, it is essential that we understand the specific circumstances that rural communities are facing.
Fundamentals of Social Work Practice with Older Adults
Social work practice is guided by a commitment to social justice that incorporates an anti-oppressive approach to working with individuals, groups and communities. When working with older adults it is essential that social workers understand and acknowledge the role that ageism plays when providing supports for older adults.
Another fundamental approach that guides generalist practice is to acknowledge the role of the environment; in social work we consider this a person-in-environment approach. We will provide an overview of the person-in-environment approach and then link this approach to a more specific discussion of micro, mezzo and macro social work interventions through the application of the social ecological framework.
Ageism
The concept of ageism was first defined by gerontologist Robert Butler in 1969. Butler considered ageism to be a form of prejudice by one age group against another, typically expressed by middle-aged adults against youth and older persons. He noted that these groups tended to be characterized as “dependent” on the middle-aged, disempowering the old and the young in a way that was comparable to sexism, racism, and other forms of discrimination. Butler viewed the effects of ageism through an intersectional lens, as he believed that its effects often compounded with other forms of discrimination to increase the impact on a marginalized person’s life (Ayalon & Tesch-Römer, 2018). This point has been supported in later research, which showed that ageism is often faced most intensely by women, the poor, people with dementia, racialized people, and people with less education (Ayalon & Tesch-Römer, 2017; Chang et al., 2020). In future work, Butler refined the concept of ageism to be a set of positive or negative attitudes, behaviours, institutional practices, and policies aimed at older adults (Ayalon & Tesch-Römer, 2018). This later definition of ageism is generally what is meant by discussing ageism today, as popular discourse on the topic tends to focus solely on biases against older adults.
Ageism manifests itself at the micro, mezzo, and macro-levels. At the micro level, ageism is developed and maintained by individuals’ thoughts, emotions, and beliefs about a particular age group. At the mezzo level, groups, organizations, and other social entities’ beliefs and actions towards age groups reinforce ageism. Macro-level ageism is created through a culture or society’s values towards specific age groups. Each of these levels assists in the production of self-directed and other-directed ageism (Ayalon & Tesch-Römer, 2018).
Additional research has found that the prevalence of ageism within a society is correlated with an increased prevalence of older adults (Marques et al., 2020; Ng & Lim-So, 2021). Also, other-directed ageism is associated with cultural anxiety related to aging and a fear of death within a society (Marques et al., 2020). The more meaningful contact people have with older adults, such as spending time with older family members, the less likely they are to hold ageist attitudes (Marques et al., 2020).
As previously noted, ageism can be self-directed or directed towards others (Marques et al., 2020). When directed outwards, the effects of ageism are most commonly seen and studied in healthcare and in the workforce. Often, this ageism is implicit, and is therefore difficult to address (São José et al., 2019). Older adults are often characterized as a “drain” on the healthcare system, which may help to propagate ageist attitudes in the system (Ayalon & Tesch-Römer, 2017). Negative stereotypes about older adults may lead medical professionals to believe that their older patients cannot handle the same treatments their younger ones can (São José et al., 2019). Older patients are also more likely to be kept out of their own treatment decisions and spoken to patronizingly or disrespectfully by medical personnel (Ayalon & Tesch-Römer, 2017).
Self-directed ageism is also commonly seen in healthcare, as older adults may refuse treatment because they view themselves as too old, or they may not receive treatment for ailments they believe are simply a part of the aging process (São José et al., 2019). Such attitudes and behaviours tend to lead to poor health, memory, cognitive performance, and work performance outcomes for older adults (Marques et al., 2020). Self-directed ageist attitudes are associated with increased morbidity and mortality (Ayalon & Tesch-Römer, 2017). Even when older adults face “compassionate” ageist attitudes, such as unwanted help or paternalistic treatment, negative health outcomes and inward-focused ageism are likely to be produced (Vervaecke & Meisner, 2021).
Older adults are often faced with ageist attitudes and stereotypes in employment. Older workers are seen as more costly and less productive than their younger counterparts. They are also the most likely to get fired first and have the greatest difficulty finding employment in poor economic conditions (Ayalon & Tesch-Römer, 2017). These phenomena are exacerbated for women, who are seen as reaching their “peak” as workers by age 35, which has negative impacts on their prospects for promotion and employment (Krekula et al., 2018). Workforce ageism also has been shown to predict poor health outcomes, such as depression and long-term illness (Chang et al., 2020).
It seems likely that every person who reaches old age will face ageism; its scope is significantly broader than other forms of discrimination (Ayalon & Tesch-Römer, 2018). This makes ageism a significant policy and practice issue that needs to be addressed in order to support aging populations. Given that the values and practice of social work are based on anti-oppressive approaches, it is critical to address ageist attitudes. By focusing on a person-in-environment perspective social workers can address these attitudes at multiple levels of practice.
Person-in-Environment Approach to Supporting Rural Older Adults
Person-in-environment is a principle that guides social workers in the practice of their profession. This principle focuses on how a person’s environmental context affects their behaviour or self. The environment, understood within the framework of person-in-environment, consists of a person’s social, economic, political, communal, historical, religious, physical, cultural and familial context. The principle also considers how an individual has an impact on their environment (Kondrat, 2013). Thus, in summary, the principle of person-in-environment is that in order to truly understand a person, one must look at the interplay between an individual and their environment.
Person-in-environment was first established as a guiding principle of practice in 1955, when the National Association of Social Workers created a study group to define social work practice (Kondrat, 2013). Following its establishment, it remained the defining feature of social work practice throughout the 20th century (Green & McDermott, 2010). Yet, within that time period up until the modern day, many refinements and advances have been made to the theory and practice of person-in-environment. The 1970s saw the advancement of two leading person-in-environment-adjacent theories: general systems theory and ecological systems theory (Kondrat, 2013).
General Systems Theory
General systems theory was the leading theoretical approach to person-in-environment up until the late 1970s (Kondrat, 2013). It was established from the work of an Austrian theoretical biologist named Ludwig von Bertalanffy, who believed that an element was best understood in relation to its constituent parts (its subsystem) and in relation to the larger or more complex elements that it was a constituent part of. He identified two types of systems or sets of elements: closed systems that are isolated from their environment and open systems that are in constant interaction with their environment. He also highlighted the concept of a subsystem, constituent elements of a larger system placed in hierarchical order, and feedback, the flow of information within an open system that produces change or stability in relation to other systems. Bertalanffy’s concept of a hierarchy of systems was invaluable to the general systems approach to social work. People and systems were seen as influenced by the larger systems of which they were a part. This meant that social work practice should emphasize the transaction between a person and systems in the environment (Kondrat, 2013).
However, some theorists believed that general systems theory was flawed, specifically due to the absence of values and ideology in its model, its implicit acceptance of finding homeostasis for an individual (thus making it less than useful to address larger social change or conflict), its abstract model being distant from real life human phenomena, and its focus on transactions between systems being at odds with social work’s commitment to person-centred work (Kondrat, 2013).
Ecological Systems Theory
Following the decline of general systems theory, ecological systems theory became the leading theoretical approach to person-in-environment. It aimed to create a more cohesive definition of theory and practice for social work (Green & McDermott, 2010). Ecological theory builds upon general systems theory and ecological science, the study of live organisms within their environment. It is most associated with Carel B. Germain and Alex Gitterman (Kondrat, 2013). Germain and Gitterman conceptualized the environment as made up of social, natural, and built features. Social environments are made up of human groupings (e.g. networks, neighbourhoods, societies, etc.), while built and natural environments are made up of physical features of the world around an individual (e.g. buildings, other living organisms, landscapes, the climate, etc.) (Rogge & Cox, 2001). In ecological systems theory, a person cannot be accurately understood apart from their environment, as they are in an interdependent relationship with their environment and the elements that make it up. It is believed that a person’s environment can facilitate or inhibit their well-being, while individuals can also impact their environment in positive or negative ways (Kondrat, 2013).
Ecological systems theory was seen as preferable to general systems theory as its root within the life sciences gave it a more concrete way of theorizing the person-in-environment perspective. It focused on the mutual relationship between persons and their environment more than general systems theory and also viewed the understanding of humans within their environmental context as crucial, rather than simply emphasized as it is under general systems theory (Kondrat, 2013). Yet, ecological systems theory has been critiqued for failing to recognize the unique place of humans as, in ecological systems theory, the individual is portrayed simply as a system among and within other systems. This also means that it fails to pay significant attention to aspects of the personal, cultural, social, physical environments where humans live (Kondrat, 2013).
While these two theories are generally understood to be the main ways in which person-in-environment is conceptualized, there is a broad variety of approaches to understand and practice the perspective across the profession of social work. For instance, what constitutes an environment according to person-in-environment differs depending on one’s theory of preference and over time. Many scholars believe that person-in-environment has been primarily applied to interpersonal and social interactions of clients, or that the natural environment is often left out of person-in-environment in practice (Rogge & Cox, 2001). Some scholars even believe that social workers should not identify just one theory to conceptualize social work practice (Kondrat, 2013).
Person-in-Environment and Rural Older Adults
When the principle of person-in-environment is applied to work with older adults in rural areas, several key themes arise. In line with the definition, the primary theme identified was that the fit of older adults within their rural communities depends upon the resources of the person and their community (Keating & Eales, 2012; Keating et al., 2013). Within this broad theme, two subthemes are highlighted: an individual’s resources to live a healthy life and environmental factors that facilitate an individual’s living a healthy life.
Wealthy individuals are generally found to live healthier lives than their poorer counterparts (Park et al., 2017; Thissen & Droogleever Fortuijn, 2021; Wang et al., 2018). These older adults had the resources they needed to live active lives and access necessary services as well as to engage in the community around them. They also had access to transportation to reach services that were not provided in their communities of residence, something of importance when considering persons living in rural settings. These resources meant that they could devote their time to pursuits that gave them satisfaction, such as community work or building large and strong social networks (Keating et al., 2013). On the other hand, poorer individuals found it more difficult to live healthy lives. This is influenced by the fact that poorer individuals are often marginalized by other facets of their lives; poor individuals are more likely to be older, single, non-white women, who have less education, lower quality of housing and neighbourhood safety, have problems with active daily living, and have a greater number of chronic conditions (Park et al., 2017).
The research identified some environmental factors that mediated older adults’ ability to lead healthy lives; the first is communities with strong social networks (Keating et al., 2013; Urbaniak & Walsh, 2021). When individuals lived in communities with strong social networks, they were more likely to live healthy lives. This factor interacts with the personal features of the individual within the environment. For instance, older adults who had lived in their communities for long periods of time experienced a better fit within their community (Thissen & Droogleever Fortuijn, 2021). This connection helps to mediate some of the issues faced by poor individuals in rural communities, as long-term neighbours can watch out for and assist with problems the individual may be facing (Keating & Eales, 2012). Poor older adults living in communities with fewer resources reported a stronger sense of camaraderie, which meant that citizens would help each other to ensure that their needs were met (Keating et al., 2013). Even rural-dwelling individuals from other marginalized communities, such as LGBTQ+ older adults, reported a strong sense of well-being because of the tight social networks they had built within their community (Rowan et al., 2013).
Alternatively, a community that lacked services needed by many older adults, such as healthcare, had the opposite effect on individuals’ well-being. Some of the communities in the literature surveyed were quite remote from urban centres, which meant that older adults had to travel further to access goods and services (Braimah & Rosenberg, 2021). A lack of services had a pronounced impact on the most vulnerable seniors, as they were less prone to travel outside of their community to fulfill their needs (Keating & Eales, 2012). Older adults are at increased risk of experiencing social isolation when residing in rural communities that have high unemployment rates or are far away from urban centres where their children may be living (Keating & Eales, 2012). A lack of familial supports may mean that an older adult needs to look elsewhere for support with tasks and chores in the home (Braimah & Rosenberg, 2021). These older adults may benefit from living in senior housing, as its supportive environment, in part, compensates for the barriers they face as they age (Park et al., 2017).
The literature also noted the importance of understanding changes in personal and environmental characteristics over time. The older a person became, the poorer their person-environment fit was on aggregate (Thissen & Droogleever Fortuijn, 2021). Neighbourhood characteristics in several of the rural communities studied in the literature changed dramatically as the residents’ demographics changed. Keating et al. (2013) noted that members of a rural Nova Scotia community who had lived there for long periods of time became newly-marginalized as a result of wealthier residents moving in and increasing the cost of living. This is important information to consider when contextualized with Thissen and Droogleever Fortuijn’s (2021) findings that population growth of older adults was most prevalent in key and relatively rich villages due to the housing opportunities and available facilities. They also found that over time, the person-environment fit between wealthy and poor older adults in relatively rich and poor communities changed, as each community type developed to fit a specific group of residents. Changes in an older adult’s life, such as the onset of an illness or becoming a caregiver for a spouse or relative, also had impacts on individuals’ levels of comfort within their community or the ability to manage stressful situations they had previously managed (Gibson et al., 2018).
Ongoing work to assess the person-environment-fit to understand the lived experiences of rural older adults should focus on particular gaps in the existing literature. Longitudinal studies of older adults living in rural communities may expose valuable information about the dynamic nature of people and their environments. Statistical data may be useful to supplement this, particularly focusing on the changing demographics and economic conditions of rural communities where older adults traditionally reside. In and out-migration of youth within these communities is another feature that could expose valuable insights about family networks and supports available to older adults. Qualitative studies that gauge the interactions older adults have within their environments, specifically related to service use, may also be relevant.
In order to highlight the specific role of social work with rural older adults we now turn to the social ecological framework as a way to discuss potential policy and practice issues at various levels of practice.
Social Ecological Model
The social ecological model can be used as a guide for social workers whose rural practice includes older adults. Urie Bronfenbrenner, a Russian-American psychologist, described individual behaviour as a complex system of relationships that is affected by multiple levels of the surrounding environment. In particular, Bronfenbrenner proposed that the environment had a direct influence on the behaviour and development of a child. Bronfenbrenner’s model included five systems: microsystem, mesosystem, exosystem, macrosystem, and the chronosystem.
The microsystem is the closest, direct relationships that surround the individual. It includes relationships and interactions that an individual has with their immediate surroundings such as people in the family, school, neighborhood, or other close settings. The mesosystem is the next closest influence that connects structures such as the connection between home, schools, religious organizations, or neighborhood to the microsystem. The exosystem includes indirect factors in the larger social system, where the individual does not necessarily play a role such as a workplace, industry, media, or government—but that may positively or negatively influence the individual. The macrosystem is the outermost level of the individual’s environment that includes cultural beliefs, values, customs, and laws. The dominant beliefs and ideologies of the individual has an impact on all other systems. The chronosystem is the final level. It reflects the cumulative experiences a person has over the course of their lifetime such as a death or physiological changes such as aging. As people age, they may react differently to environmental changes.
In the 1980’s, Bronfenbrenner’s model, used mainly to explain behaviour, was modified by McLeroy et al. (1988) as the social ecological model, to promote health and prevent disease among the general population. McLeroy et al. adapted the model to five sources of influence: Intrapersonal, Interpersonal, Institutional, Community, and Public Policy (see Figure 1) which were used to guide the development of interventions. The intrapersonal (individual) level includes beliefs, values, education, skills and other individual factors. The interpersonal level includes relationships between individuals. The organizational level pertains to how institutions are organized and managed. The community level includes the networks, associations, neighborhoods, and attitudes among different institutions within communities. The policy level refers to policies and regulations that affect the individual and organizations they function within.
Figure 1
The Social Ecological Model

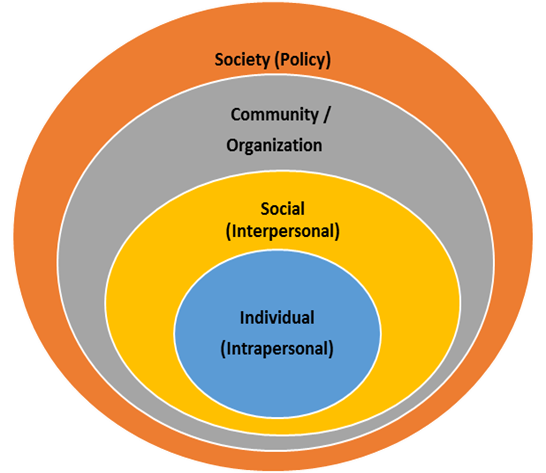
In the 1990’s, Stokols (1996), refined the social ecological model to four levels: individual, interpersonal, community and society (see Figure 2) and identified four assumptions concerning the interrelations among environmental conditions and human behavior.
The first level, the individual or intrapersonal level consists of factors such as knowledge and attitudes, beliefs and perceptions, skills and abilities as well as the individual’s age, sex, level of education, socioeconomic status, employment and self-efficacy. At this level, strategies to affect change in behaviour may include education, counselling and mentoring programs.
The next level in the model is the social or intrapersonal, which has a significant influence on the individual’s behaviour. The social environment that surrounds the individual consists of the relationships, culture, and society in which the individual is part of. For example, factors in this level may include family and social support networks, spouse or partner, peers, organizations such as schools, workplaces or community organizations that the individual is involved in. Also included in this level is the community culture, norms and socioeconomic status. Strategies affecting behaviour change at this level are intended to promote positive community attitudes and raise awareness. These may include community education, support groups, peer programs, workplace wellness initiatives and social media campaigns.
The third level consists of community or organizational factors, sometimes referred to as the physical environment in which the individual lives. The physical environment consists of both the natural environment and the built environment. Factors may include weather, geography, availability and accessibility of facilities and services, safety and aesthetics, community design and connectivity and access to public transportation. Strategies targeting this level should precede the individual and social level. This is a key concept in Stokols’ model as the environment the individual lives in may promote or deter health outcomes.
The final level is the policy or society level. This level consists of laws, legislation, and policies at a national, provincial, or local level that influence behaviour. For example, policies such as community plans, transportation, education, health, environment and workplace policies are often considered at this level.
Figure 2
The Social Ecological Model
Core Assumptions of the Social Ecological Model
In addition to the four levels proposed by Stokols (1996), the social ecological model consists of four assumptions. The first assumption is based on the premise that multiple levels of factors influence behaviour. Therefore, to successfully implement interventions, the interrelationship between levels of the social ecological model must be targeted. This is a key aspect of the social ecological model versus theories that target only one or two levels.
The second assumption of the social ecological model is that interactions occur at various levels of organization such as individual, group, organisational, community or population levels, and among various interacting factors within each level. As interactions are multi-dimensional and complex, dynamic interrelationships between individuals and their environment are regarded as a reciprocal relationship. The individual is influenced by the social, physical and policy environments, while at the same time individual, group, or organisations affect the environment. The challenge becomes identifying which factors are key to change at each level.
The third assumption infers that multi-level interventions are most effective in fostering behaviour change, rather than solely focussing on the individual. Changing the environment can result in a modification of behaviour; however, individual and social levels must also be included to foster change.
The fourth assumption implies that social ecological models need to be tailored to each specific behaviour change, as environment and policy variables are often behaviour-specific. The core principles of the social ecological model are particularly important for rural communities where access to resources are limited and cooperation among community partners becomes imperative for successful intervention.
Social Ecological Model Applied in Rural Practice with Older Adults
With the emergence of social ecological models through the work of Bronfenbrenner (1999), McLeroy et al., (1988), and Stokols (1996), greater recognition of the complex interaction among a number of determinants within the individual, social, environmental and policy domains have been emphasized. The ability for people to engage in health promoting behaviours are influenced by multiple factors within individual, social, environmental, and policy levels (Hill & Hymus, 2019; Nemoto et al., 2021). This is particularly evident in rural communities where people face unique challenges such as lower income, inadequate housing and public transportation, poor access to health care services including specialty services and preventative care, higher functional disability, chronic disability and increased sedentary lifestyle (Bacsu et al., 2014). As a result of changing economic and political forces, rural communities are experiencing more hospital closures, increased financial barriers where lower income makes travel for services difficult, and an out-migration of younger rural residents to urban centres for employment (Malone, 2011; Schmidt et al., 2016). Older adults living in rural communities are often more removed from social supports and services than urban residents (Kaye, 2017). Therefore, to support successful aging among rural older adults, it is imperative to consider the range of factors within each level for effective policy and social work practice.
Individual/Micro Level
The individual or intrapersonal level is at the centre of the social ecological model. It pertains to an individual’s physical and cognitive characteristics and past experiences. This level of the social ecological model is strongly influenced by all other levels.
Individual factors include physical characteristics such as sex, age, genetics, health history, education, economic status, along with cognitive characteristics such as knowledge, skills, attitudes and beliefs about factors related to health and healthy behaviors. People’s knowledge, skills, attitudes and beliefs help them understand how susceptible they are, how serious a health-related issue is, and the overall threat to them personally; while having knowledge alone is often not enough to change behaviour, it may influence attitudes and decisions that an individual is able to make.
When considering factors within the individual level, rural residents are more likely to experience higher rates of smoking, obesity, and hypertension, as well as lower rates of physical activity and fruit and vegetable consumption (Blackford et al., 2016). These factors have a direct impact on the health of the individual. Thus, compared to their urban counterparts, rural older adults generally experience poorer health in terms of increased mortality, lower life expectancy and functional health, and increased risk of diseases, illness, and injury (Jeffery et al., 2014). Many are also at a higher risk of dying prematurely from circulatory diseases, with rural males having the shortest life expectancy and smaller proportion of their life in good health, when compared to urban males.
Among rural older adults, health is perceived as very important (Bacsu et al., 2014). Many older adults who engage in behaviours, such as regular physical activity and a balanced diet, are aware of and acknowledge positive health benefits to changing their behaviours, particularly in environments that do not support healthy living. Addressing risk factors at the individual level alone has a tendency to put the responsibility on the individual to take control of their health; however, the social ecological model asserts that many other factors outside the individual have a strong influence on health and health-related behaviours; therefore, the individual as part of their social and physical environment also needs to be considered for effective intervention. This approach is supported by Meisner et al. (2019), who stated that among rural older adults, programs and services should strive to promote physical and mental health, in addition to social participation and meaningful connection to others.
Some specific social work strategies that target the individual may include counselling and consultation, life skills training, healthy relationship building, and educational and awareness programs. When designing public health interventions, individual level factors are important to consider, as many individual characteristics such as economic status, for instance, influence an individual’s ability to access various services.
Social/Mezzo Level
At a social level, healthy aging is influenced by the opportunity for older adults to participate in social interactions with others (Carver et al., 2018). The social or interpersonal level includes the relationships and social networks an individual takes part in. Factors at this level include families, friends and cultural traditions. These factors have great potential to impact individual behaviors. Rural older adults often report a strong sense of trust and belonging to the community where mutual support is key to healthy aging (Bacsu et al., 2014; Witcher, 2017); therefore, the social environment has an important role in the health of an individual (Stokols, 1996). Social interaction is associated with physical and mental health benefits among older adults, and enhancing opportunities for interaction is a valuable asset in maintaining health and wellness, particularly among older adults in rural communities (Douglas et al., 2017).
Although rural older adults acknowledge that the social interaction while participating in activities with other people is beneficial, many are at increased risk of social isolation and lower social functioning, which is further hindered by the fear of falling and lack of opportunity to interact socially with others in their community (Bacsu et al., 2014; Schmidt et al., 2021). Social workers can initiate programs and interventions that integrate a social component in order to foster increased participation and engagement in health promoting behaviours among rural older adults. For example, physical activity and social interaction generally share a reciprocal relationship in supporting positive health outcomes among older adults. Massie et al. (2021) report that physical activity programs that encourage social connections within the community and a sense of belonging may be more effective in increasing physical activity levels among older adults. Social support is key in physical activity engagement among rural older adults, particularly when a supportive partner is involved; therefore, engaging people in physical and social activities at the community level may help to improve health outcomes among rural older adults (Soto et al., 2019). Hoogland et al. (2019) further add that older adults benefit from engaging in health-promoting activities with younger relatives as a means of social connectedness and mutual health benefits. As such, intergenerational initiatives such as school and senior visiting programs and activities may further support physical and social health. Hebblethwaite et al. (2020), who studied the experiences of family leisure among intergenerational rural families, found that family-based leisure activities played an important role in developing close social bonds. Berg-Weger and Morley (2020) emphasize the importance of social interaction for all ages, especially during the COVID-19 pandemic, where the social environment was greatly impacted by physical distancing protocols. To promote social interaction, Berg-Weger and Morley suggest interventions such as daily telephone calls and virtual visits.
Although research findings support the use of technology to keep rural older adults socially connected (Hajek & König, 2020; Xie et al., 2020), individual level factors need to be considered; according to Padala et al. (2020), older adults in rural areas report less capability and willingness to participate in video telehealth visits. This resistance to telehealth is further reported by Henning-Smith (2020), who report that older adults use technology at lower rates than younger people and often lack access to reliable internet and computer-based devices. With many organizations and services shifting online, this change may pose a serious barrier for rural older adults to connect and communicate with others. Walker et al. (2021) suggest that among rural older adults, particularly those age 85 and older where infrastructure is limited, a telephone call appears to be an effective means of social communication, particularly during the COVID-19 pandemic where in-person restrictions were in place.
Creative solutions are needed to promote and support social interaction among older adults in rural communities, beginning with understanding the specific facilitators of and barriers to social interaction. There are numerous health-related advantages to living in rural communities that are typically characterized by the opportunities for older adults to socially engage with the community through volunteering at local events and organizations, engaging with others in church groups, community centres, and service clubs (Kaye, 2017).
Gaining a better understanding of healthy aging in rural communities requires further exploration into interventions that support aging and create supportive physical and social environments, particularly in rural areas (WHO, 2011). In order to do so, it is essential to build collaborative partnerships between older adults and community decision-makers, healthcare professionals, policy-makers, and municipal leaders to address barriers to supporting healthy behaviours. Collaborations involving healthcare leaders, community and educational administrators, in consultation with older adults and youth in the community, would be beneficial in developing targeted initiatives to combat social isolation or loneliness.
In addition, an environmental scan of opportunities and challenges that rural communities face in terms of internet, technology and, access to equipment needs further investigating. Levasseur et al. (2020) add that personal and environmental factors all need to be considered to promote social interaction among rural older adults.
Environment/Macro Level
The physical environment has an important influence on health and mental health and wellness (Sallis et al., 2008). In the social ecological model, the physical environment is situated within the organization or at the community level. It includes both the natural and built environment. There are notable differences in healthy aging depending on the context in which people live. According to Jeffery et al. (2014), people living in rural communities face unique opportunities and challenges compared to their urban counterparts. Within many rural communities, access to recreation facilities, parks and trails, aesthetics, and safety influence health of the residents (Schmidt et al., 2021). Living in close proximity to services and recreational facilities are important factors in performing daily activities and initiating social interactions with members of the community (Levasseur et al., 2020).
In many rural and remote communities, social, economic and environmental barriers are evident. These include limited funding for infrastructure, lack of technological advances, and aging and reduced rural populations (CPRA, 2015). Barriers in the physical environment influence the opportunity and ability for older adults to engage in both physical and social activity. Other challenges common among older adults in rural communities include lack of public transportation, inadequate access to specialized health care services, limited housing and home-care and economic barriers related to lower income.
Although many rural communities are often at a disadvantage in terms of a decreasing and aging population, limited funding for infrastructure, and challenges in accessible technology and transportation, rural living has notable advantages. These include opportunities to connect with the natural environment and having a strong sense of community belonging. Ensuring that communities are walkable and accessible for older adults may encourage more people to engage in active transportation to conduct errands such as getting the mail and paying bills, adding meaningful activity into daily living.
Initiatives such as creating safe, outdoor walking programs or peer-led exercise classes using the natural environment to engage older adults in physical activity are beneficial. Supporting these initiatives requires working collaboratively across various sectors including municipal leadership, health and social organizations, and community organizations that represent the residents. Social workers can play an important role in facilitating and building these collaborations at the community level.
Strategies at this level are often developed to address the social and physical environment simultaneously. For example, communities can improve health by reducing social isolation, improving economic and housing opportunities, and addressing barriers and facilitators of engagement in the natural and built environment. This may include improving the physical and social environment to create safe places where people live, learn, work, and play by addressing the conditions that impact communities such as poverty, safety, isolation, or access to services. Other examples may include increasing access to fresh fruits and vegetables in local stores, creating farmers’ markets to promote locally grown, affordable foods, or creating accessible walking trails, parks, or access to indoor sites where older adults can be physically active and engaged with others.
Policy/Macro Level
Supporting social policies and advocating for opportunities for rural older adults to remain active and engaged in the community is very important to health and wellness (Novek et al., 2013). Policy level interventions rely on multi-level influences to address health of the population, recognizing that both policy and environment (social and physical) influence individual behaviour. Recently, organizations have demonstrated the use of the social ecological model in frameworks and guidelines for increasing activity, promoting the use of parks and recreation, and proposing interventions to improve health of populations. An example is the Framework for Recreation in Canada, which is an initiative of the Interprovincial Sport and Recreation Council and the Canadian Parks and Recreation Association (CPRA, 2015). This framework was developed in collaboration between community leaders, local and provincial organizations and national associations to assist communities and partners to create more supportive physical and social environments that encourage recreation and outdoor activity among Canadians. Interventions at each level—individual, social, environmental and policy—are outlined in the recommendations for action.
Other examples of policy level interventions that impact older adults in rural communities include zoning codes and bylaws that support active transportation and public access to existing facilities for programs and service delivery. Partnerships among sectors such as education, religious institutions and community organizations are key in advocating for investments in public housing, infrastructure, and transportation to support older adults in rural communities.
There is much to be gained by using a social ecological model to influence behaviour and implement interventions specific to the needs of rural older adults. By engaging multiple sectors in the planning and decision-making, social workers recognize that interventions that consider multiple levels are typically are more successful than those targeting only one or two levels of influence.
Conclusion
Using a social ecological model produces valuable insight into the relationship between individual, social, and environment factors that influence successful aging among rural older adults. There is much to be gained in focusing on the advantages of rural living, including the connection to the natural environment and the inter-relationship between physical activity and social interaction, and working collaboratively with rural community members and organizations to address the existing barriers that many rural communities are facing. Generalist social workers have the professional training and commitment to understand the importance of addressing the issues faced by rural older adults from a social ecological perspective—a perspective which highlights the importance of considering all aspects of an individual’s environment.
Activities and Assignments
- Note your own assumptions and pre-judgments about older adults and aging people in our society and how these relate to the concept of ageism discussed in the chapter. What do you identify as challenges and opportunities for a rural social worker working with this population?
- Vivian is 75 years old and living in a small rural community. She is unable to drive and now lives alone since her husband has moved into a long-term care facility in another community that is 150 km away from where Vivian lives. Vivian’s children do not live close by and she has expressed to the social worker that she often feels very lonely and wishes that she had some activities that she could attend as she is very social and likes to visit with other people. Discuss how components of the social ecological model could guide the social worker to suggest some interventions that might assist Vivian.
- Select a rural community in the area where you live and conduct some research to determine the number of older adults, the resources and services available to them, and any gaps that are evident to support successful aging for older adults in that community.
Additional Resources
- Leader, J., Catherwood, K., & Exner-Pirot, H. (2021). Saskatchewan. In K. Rich, H. Hall & G. Nelson (Eds.), State of rural Canada 2021: Opportunities, recovery and resiliency in changing times (pp. 32-42). Canadian Rural Revitalization Foundation.
- World Health Organization (2021). Global report on ageism: Executive Summary. World Health Organization
References
Ayalon, L., Tesch-Römer, C. (2017). Taking a closer look at ageism: self- and other-directed ageist attitudes and discrimination. European Journal of Ageing 14, 1–4.
Ayalon, L., Tesch-Römer, C. (2018). Introduction to the Section: Ageism—Concept and Origins. In Ayalon, L., Tesch-Römer, C. (Eds) Contemporary Perspectives on Ageism. Springer Cham.
Bacsu, J., Jeffery, B., Abonyi, S., Johnson, S., Novik, N., Martz, D., & Oosman, S. (2014). Healthy aging in place: Perceptions of rural older adults. Educational Gerontology, 40(5), 327-337.
Berg-Weger, M., & Morley, J. E. (2020). Editorial: Loneliness and social isolation in older adults during the COVID-19 pandemic: Implications for gerontological social work. The Journal of Nutrition, Health & Aging, 24(5), 456–458.
Blackford, K., Jancey, J., Lee, A.H. et al. (2016). Effects of a home-based intervention on diet and physical activity behaviors for rural adults with or at risk of metabolic syndrome: A randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity, 13(13).
Braimah, J.A., & Rosenberg, M.W. (2021). “They do not care about us anymore”: Understanding the situation of older people in Ghana. International Journal of Environmental Research and Public Health 18, 2337.
Bronfenbrenner, U. (1999). Environments in developmental perspective: Theoretical and operational models. In S. L. Friedman & T. D. Wachs (Eds.), Measuring environment across the life span: Emerging methods and concepts (pp. 3–28). American Psychological Association.
Canadian Parks and Recreation Association (CPRA). (2015). A framework for recreation in Canada 2015. Pathways to wellbeing. A joint initiative of the interprovincial sport and recreation council and the Canadian parks and recreation association. Retrieved from https://cpra.ca/wp-content/uploads/2021/04/FrameworkForRecreationInCanada_2016wcitation.pdf
Carver, L.F., Beamish, R., Phillips, S.P. & Villeneuve, M. (2018). A scoping review: Social participation as a cornerstone of successful aging in place among rural older adults. Geriatrics, 3(75).
Chang, E. S., Kannoth, S., Levy, S., Wang, S. Y., Lee, J. E., & Levy, B. R. (2020). Global reach of ageism on older persons’ health: A systematic review. PloS one, 15 (1).
Douglas, H., Georgiou, A., & Westbrook, J. (2017). Social participation as an indicator of successful aging: An overview of concepts and their associations with health. Australian Health Review: A Publication of the Australian Hospital Association, 41(4), 455–462.
Gibson, A., Walsh, J., & Brown, L.M. (2018). A perfect storm: Challenges encountered by family caregivers of persons with Alzheimer’s disease during natural disasters. Journal of Gerontological Social Work 61(7), 775-789.
Green, D., & McDermott, F. (2010). Social work from inside and between complex systems: Perspectives on person-in-environment for today’s social work. The British Journal of Social Work 40(8), 2414-2430.
Hajek, A., & König, H. H. (2021). Social isolation and loneliness of older adults in times of the COVID-19 pandemic: Can use of online social media sites and video chats assist in mitigating social isolation and loneliness? Gerontology, 67(1), 121–124.
Hebblethwaite, S., Young, L., & Martin Rubio, T. (2020). Pandemic precarity: Aging and social engagement. Leisure Sciences, 43, 170 – 176.
Henning-Smith, C. (2020). The unique impact of COVID-19 on older adults in rural areas. Journal of Aging & Social Policy, 32(4-5), 396–402.
Hill, T. & Hymus, B. (2019). Promoting physical activity among community dwelling older adults in rural Hastings & Prince Edward counties. Retrieved from https://hpepublichealth.ca/wp-content/uploads/2020/10/Judys-Older-Adult-SA-Report_AUG_2019-FINAL.pdf
Hoogland, A. I., Hoogland, C. E., Bardach, S. H., Tarasenko, Y. N., & Schoenberg, N. E. (2019). Health behaviors in rural Appalachia. Southern Medical Journal, 112(8), 444–449.
Jeffery, B., Bacsu, J., Abonyi, S., Johnson, S., Martz, D., & Novik, N. (2014). Rural Seniors. In: Michalos A.C. (Eds.) Encyclopedia of Quality of Life and Well-Being Research. Springer, Dordrecht.
Kaye, L.W. (2017). Older adults, rural living, and the escalating risk of social isolation. Public Policy & Aging Report, 27(4).
Keating, N., & Eales, J. (2012). Diversity among older adults in rural Canada: Health in context. In J.C. Kulig & A.M. Williams (Eds.), Health in Rural Canada (pp. 427-446). UBC Press.
Keating, N., Eales, J., & Phillips J.E. (2013). Age-friendly rural communities: Conceptualizing ‘best fit’. Canadian Journal on Aging 32(4), 319-332.
Kondrat, M. (2013). Person-in-Environment. Encyclopedia of Social Work.
Krekula, C., Nikander, P., Wilińska, M. (2018). Multiple marginalizations based on age: Gendered ageism and beyond. In Ayalon, L., Tesch-Römer, C. (Eds.) Contemporary Perspectives on Ageism. Springer Cham.
Levasseur, M., Routhier, S., Clapperton, I. (2020). Social participation needs of older adults living in a rural regional county municipality: Toward reducing situations of isolation and vulnerability. BMC Geriatrics 20, 456.
Malone, J. L. (2011). Professional practice out of the urban context: Defining Canadian rural psychology. Canadian Psychology / Psychologie canadienne, 52(4), 289-295.
Marques, S., Mariano, J., Mendonça, J., De Tavernier, W., Hess, M., Naegele, L., Peixeiro, F., & Martins, D. (2020). Determinants of ageism against older adults: A systematic review. International journal of environmental research and public health, 17(7), 2560.
Massie, A. S., Johnston, H., Sibley, D., & Meisner, B. A. (2021). Factors associated with the intention to begin physical activity among inactive middle-aged and older adults. Health Education & Behavior.
McLeroy, D., Bibeau, D. Steckler, A. & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4). 351-377.
Meisner, B. A., Hutchinson, S. L., Gallant, K. A., Lauckner, H., & Stilwell, C. L. (2019). Taking ‘steps to connect’ to later life: Exploring leisure program participation among older adults in rural communities. Society and Leisure, 42(1), 69–90.
Nemoto, Y., Sakurai, R., Matsunaga, H., Murayama, Y., Hasebe, M., Nishi, M., Narita, M., & Fujiwara, Y. (2021). Social contact with family and non-family members differentially affects physical activity: A parallel latent growth curve modeling approach. International Journal of Environmental Research and Public Health, 18(5), 2313.
Ng, R. & Lim-Soh, J.W. (2021). Ageism linked to culture, not demographics: Evidence from an 8-billion-word corpus across 20 countries. The Journals of Gerontology: Series B 76 (9), 1791–1798.
Novek, S., Menec, V., Tran, T., & Bell, S. (2013). Exploring the impacts of senior centres on older adults. Centre on Aging. Retrieved from https://www.gov.mb.ca/seniors/publications/docs/senior_centre_report.pdf
Padala, K. P., Wilson, K. B., Gauss, C. H., Stovall, J. D., & Padala, P. R. (2020). VA video connect for clinical care in older adults in a rural state during the COVID-19 pandemic: Cross-sectional study. Journal of Medical Internet Research, 22(9), e21561.
Park, S., Han, Y., Kim, B., & Dunkle, R.E. (2017). Aging in place of vulnerable older adults: Person-environment fit perspective. Journal of Applied Gerontology 36(11), 1327-1350.
Rogge, M.E., & Cox, M.E. (2001). The person-in-environment perspective in social work journals. Journal of Social Service Research 28(2), 47-68.
Rowan, N.L., Giunta, N., Grudowski, E.S., & Anderson, K.A. (2013). Aging well and gay in rural America: A case study. Journal of Gerontological Social Work 56(3), 185-200.
Sallis, J. F., Owen, N., & Fisher, E. B. (2008). Ecological models of health behavior. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behavior and health education: Theory, research, and practice. 465–485. Jossey-Bass.
São José, J., Amado, C., Ilinca, S., Buttigieg, S. C., & Taghizadeh Larsson, A. (2019). Ageism in health care: A systematic review of operational definitions and inductive conceptualizations. The Gerontologist, 59(2), e98–e108.
Saskatchewan Bureau of Statistics. (2022). 2021 Saskatchewan Census Population Report. https://www.saskatchewan.ca/government/government-data/bureau-of-statistics/population-and-census.
Schmidt, L., Johnson, S., Genoe, M. R., Jeffery, B & Crawford, J. (2021). Social interaction and physical activity among rural older adults: A scoping review. Journal of Aging and Physical Activity. Pre-print.
Schmidt, L., Rempel, G., Murray, T. C., McHugh, T.L., & Vallance, J. K. (2016). Exploring beliefs around physical activity among older adults in rural Canada. International Journal of Qualitative Studies on Health and Well-Being, 11,
Soto, S. H., Callahan, L. F., Bahorski, S., Altpeter, M., Hales, D. P., Phillips, A., Carthron, D., & Rini, C. (2019). The role of cohabitating partner and relationship characteristics on physical activity among individuals with osteoarthritis. International Journal of Behavioral Medicine, 26(5), 522–530.
Statistics Canada. (2022a). In the midst of high job vacancies and historically low unemployment, Canada faces record retirements from an aging labour force: number of seniors aged 65 and older grows six times faster than children 0-14 (no. 11-001-X). https://www150.statcan.gc.ca/n1/en/daily-quotidien/220427/dq220427a-eng.pdf?st=XGF1hDY8.
Statistics Canada. (2022b). A portrait of Canada’s growing population aged 85 and older from the 2021 Census (no. 98-200-X).
Statistics Canada. (2022c). Focus on Geography Series, 2021 Census of Population: Saskatchewan [Data visualization tool]. https://www12.statcan.gc.ca/census-recensement/2021/as-sa/fogs-spg/Page.cfm?Lang=E&Dguid=2021A000247&topic=2.
Statistics Canada. (2022d). Population growth in Canada’s rural areas, 2016 to 2021 (no. 98-200-X).
Stokols D. (1996). Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion: AJHP, 10(4), 282–298.
Thissen, F., & Droogleever Fortujin, J. (2021). ‘The village as a coat’; changes in the person-environment fit for older people in a rural area in The Netherlands. Journal of Rural Studies 87, 431-447.
Urbaniak, A., & Walsh, K. (2021). Policy and practise perspectives on older adult critical life-course transitions and place in Ireland. Health and Social Care in the Community 29(5), 97-106.
Vervaecke, D. & Meisner, B.A. (2021). Caremongering and assumptions of need: The spread of compassionate ageism During COVID-19. The Gerontologist 61 (2), 159–165,
Walker, R. B., Grome, M., Rollyson, W., & Baus, A. D. (2021). Ensuring contact: calling rural Appalachian older adults during the COVID-19 epidemic. Rural and Remote Health, 21(1), 6122.
Wang, Y., Chen. Y., Shen, H., & Morrow-Howell, N. (2018). Neighbourhood and depressive symptoms: A comparison of rural and urban Chinese older adults. Gerontologist 58(1), 68-78.
Witcher, C. S. G. (2017). Rural older adult physical activity promotion: Past, present, and future. Topics in Geriatric Rehabilitation, 33(3), 162-169.
World Health Organization [WHO]. (2011). Global recommendations on physical activity for health. 65 years and above.
Xie, B., Charness, N., Fingerman, K., Kaye, J., Kim, M. T., & Khurshid, A. (2020). When going digital becomes a necessity: Ensuring older adults’ needs for information, services, and social inclusion during COVID-19. Journal of Aging & Social Policy, 32(4-5), 460–470.

