Axonal Injury in the PNS and the CNS
The previous chapter dealt with the impact that micro-organisms had on the health of neurons. This chapter outlines the differing roles of the PNS and CNS following injury and during recovery. It has long been known that following damage to axons, that the neurons within the PNS can undergo outgrowth and can recover (i.e. undergo regeneration) while neurons within the CNS do not seem capable of doing so.
What are the key differences?
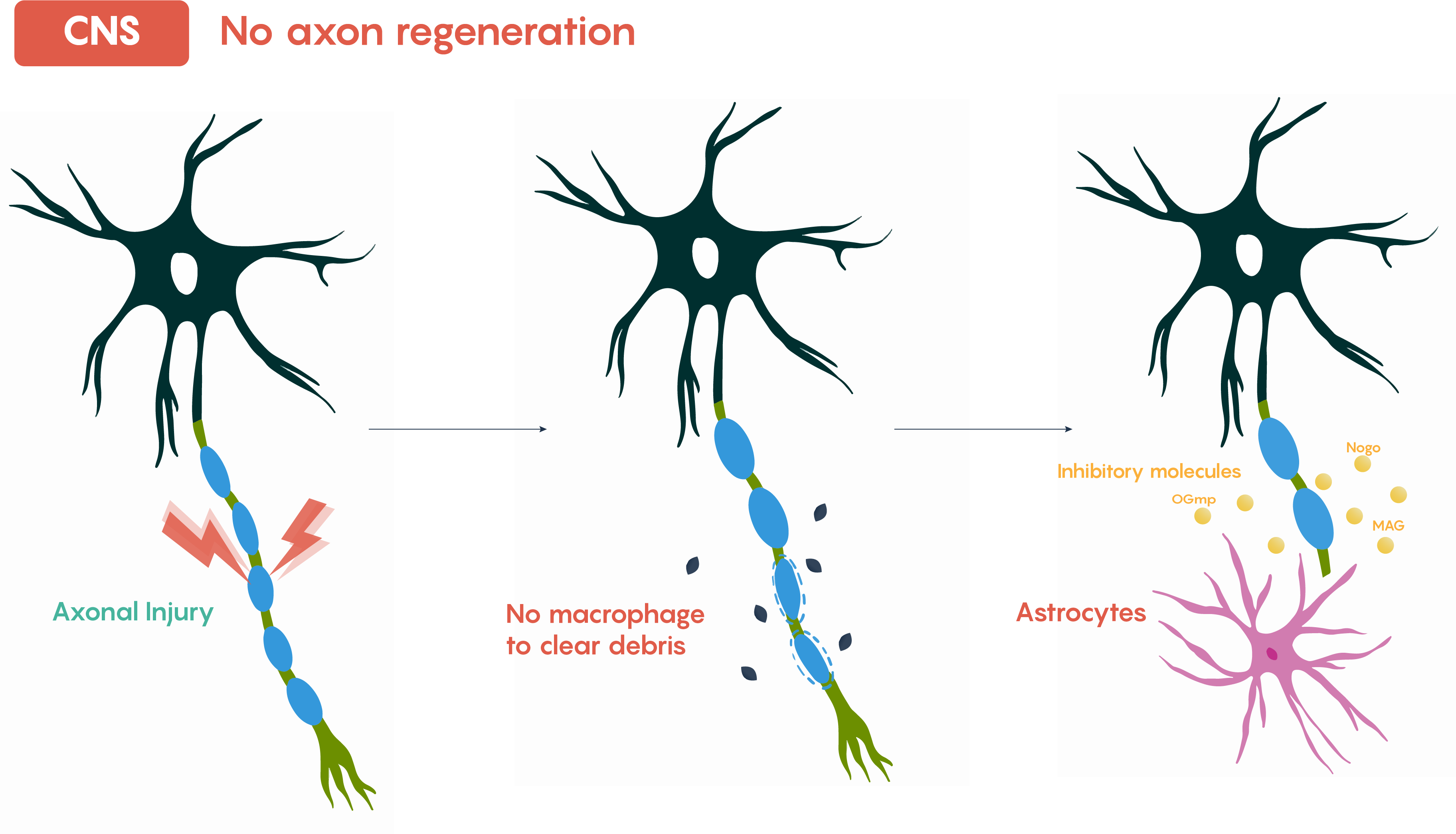
Although it is possible that there are inherent properties that make neurons in the CNS somehow different from those in the PNS, it is more likely that external factors and cells account for the differences in their abilities to regenerate following damage. As shown in Figure 1. above, within the CNS, following axonal injury, the site of damage distal to injury (i.e. further away from damage) often undergoes degeneration and the distal axon degenerates and eventually disappears. Although there are several reasons that this is thought to occur, most notably this is believed to involve a lack of macrophage clearing of damaged myelin as well as the formation of a glial scar via activated astrocytes that cause a physical barrier to their re-growth. Additionally, molecules that are unique to the CNS (see the chapter in this Unit on Multiple Sclerosis) also are believed to be up-regulated within the CNS following damage that prevents regeneration. These molecules are associated with the CNS specific glial cells, oligodendrocytes that provide myelination, and these cells increase the production of Nogo, MAG (Myelin Associated Glycoprotein) and OGmp (Oligodendroctye myelin glycoprotein) among others.
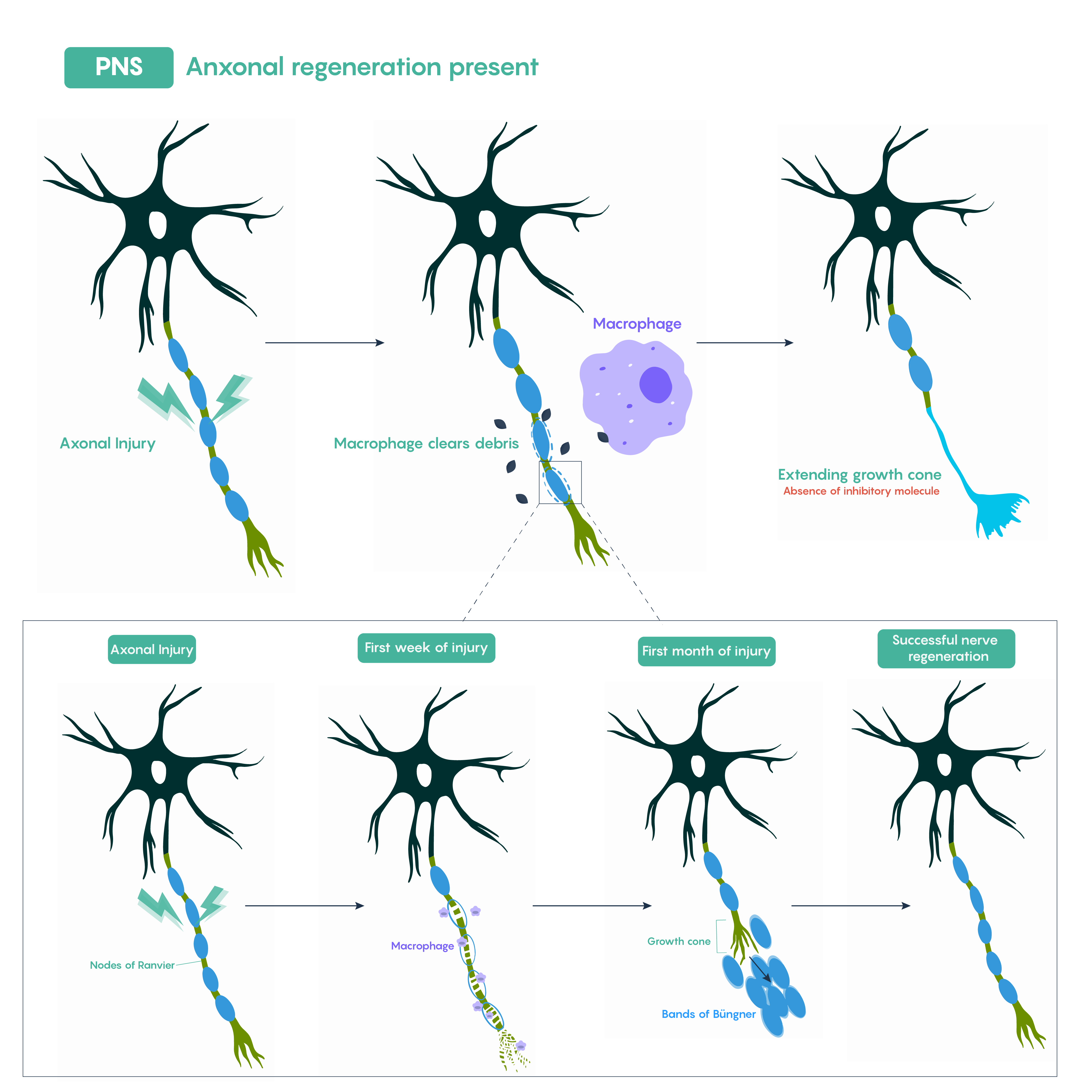
In contrast, PNS neurons (bottom panel of figure 1) show significant clearing of damaged axons via macrophages (not observed in the CNS) and then axonal outgrowth and repair across the bridge of Schwann cells that occurs following a process known as Wallerian degeneration (the loss of the axon distal to the injury).
Pathophysiological implications – TBI (Traumatic Brain Injury)
You might be asking yourself, where do these types of axonal injuries occur with the brain and CNS? Increasingly researchers and clinicians are finding that there is a specific axonal injury that could occur following traumatic brain injury (TBI) or concussion-related injuries. One of the ways in which axons within the brain become damaged includes the process of coup/contrecoup where the brain (and its neurons) are first compressed (coup) and then stretched (contrecoup). The mechanical forces on the neuron on the brain may result in varying degrees of damage to the neurons (Figure 2.).
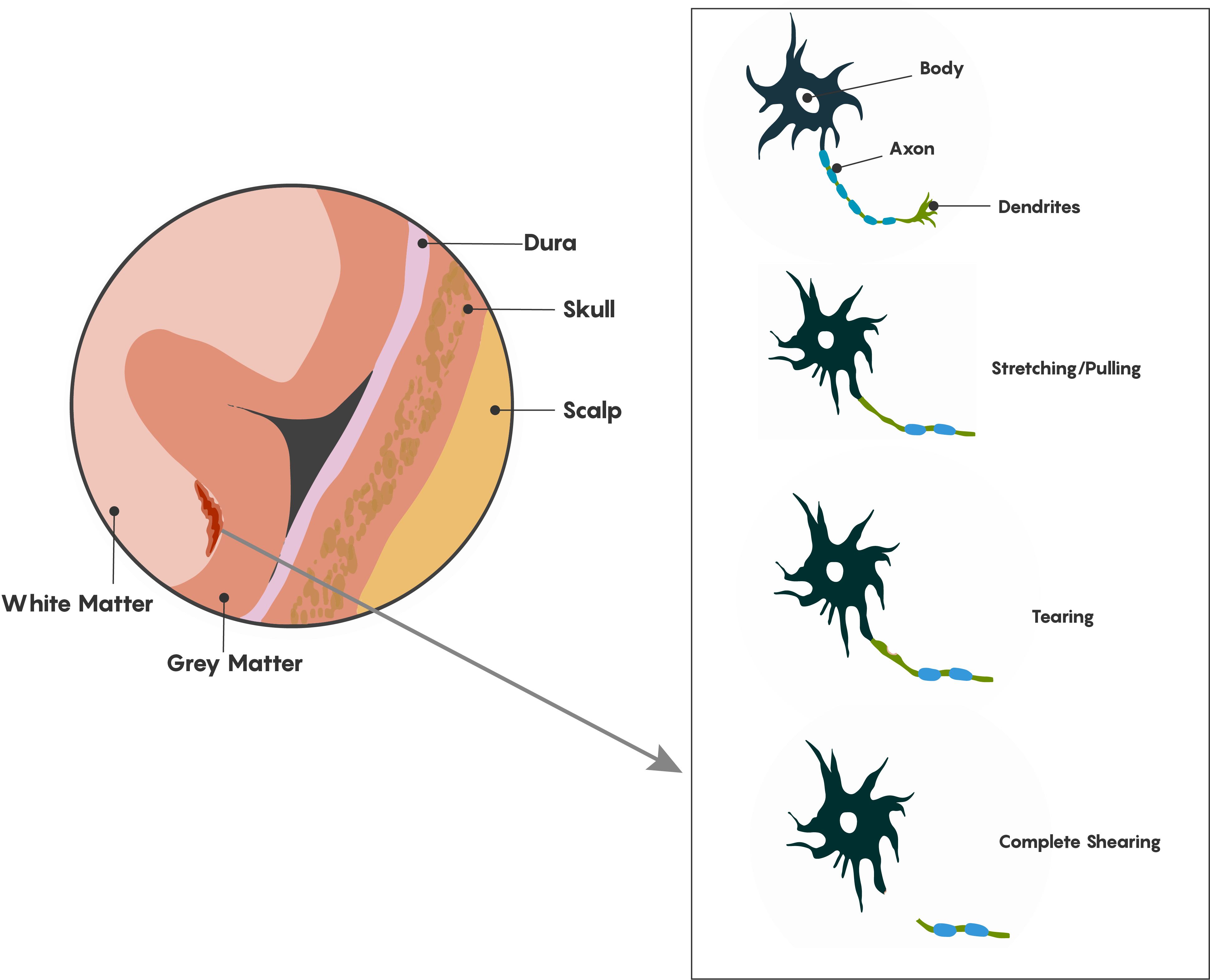
As illustrated in Figure 2., depending on the area of the brain is impacted, a number of different types of damage can occur along the length of the axon including stretching/pulling of axons which may affect myelination and localization of axonal channel proteins, and both tearing and shearing which will cause loss of axonal integrity. This type of diffuse axonal injury will have effects on both the structure of the grey matter of the brain and the white matter axonal tracts. Ultimately these types of injuries often go undetected and the most common methods used are clinical assessments using variations of the Glasgow Coma Scale (GCS) that examine the severity of the loss of consciousness as these injuries, although structural are undetectable by either MRI or CT-scans.
Did you know?
Did you know that there is still controversy between TBI/concussions and the development of a neurodegenerative disorder known as Chronic Traumatic Encephalopahty (CTE) which is thought to cause behavioural changes in athletes in sports with contact/impact?
Although there are likely structural changes as indicated above, most often the diagnosis of post-concussion or TBI related disturbances occurs because of functional changes in cognitive function and possible mood disorder changes (depression etc.). Although there are likely structural changes as indicated above, most often the diagnosis of post-concussion or TBI related disturbances occurs because of functional changes in cognitive function and possible mood disorder changes (depression etc.).
Did you know that one of the chief complaints following TBI/concussions is the inability to concentrate and focus on computer/TV screens? Individuals with concussion injuries require not just physical rest but cognitive rest, and typical LCD screens refresh at a 60 Hz rate. Most individuals are capable of processing and fusing these high-frequency images without a cognitive load, but following concussions, individuals will have higher critical flicker frequencies such that staring at a screen will increase cognitive fatigue and eyestrain. We don’t understand why this happens yet but perhaps there is a Nobel Prize in it for an aspiring neurobiologist!
Chapter Checkpoint: Complete the following quiz

