4
Learning Objectives
- Examine the anatomy of the sensory systems
- Determine the main functions of the sensory systems
- Differentiate the medical terms of the sensory systems and common abbreviations
- Discover the medical specialties associated with the sensory systems
- Recognize common diseases, disorders, and procedures related to the sensory systems
Sensory Systems Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Sensory Systems.
Introduction to the Sensory Systems
Ask anyone what the senses are, and they are likely to list the five major senses as taste, smell, touch, hearing, and sight. However, these are not all of the senses. The most obvious omission from this list is balance. Touch can be further subdivided into pressure, vibration, stretch, and hair-follicle position based on the type of mechanoreceptors that perceive these touch sensations. Other overlooked senses include temperature perception by thermoreceptors and pain perception by nociceptors.
Within the realm of physiology, senses can be classified as either general or special. A general sense is one that is distributed throughout the body and has receptor cells within the structures of other organs. Mechanoreceptors in the skin, muscles, or walls of blood vessels are examples of this type. General senses often contribute to the sense of touch, as described above, or to proprioception and kinesthesia, or to a visceral sense, which is most important to autonomic functions. A special sense is one that has a specific organ devoted to it, namely the eye, inner ear, tongue, or nose.
Gustation (Taste) and Olfaction (Smell)
Watch this video:
Media 4.1 Taste & Smell: Crash Course A&P #16 [Online video]. Copyright 2015 from CrashCourse.
Practice Medical Terms Related to the Sensory Systems
Gustation (Taste)
Gustation is the special sense associated with the tongue. The surface of the tongue, along with the rest of the oral cavity, is lined by a stratified squamous epithelium. Raised bumps called papillae contain the structures for gustatory transduction. There are four types of papillae, based on their appearance:
- circumvallate
- foliate
- filiform
- fungiform
Within the structure of the papillae are taste buds that contain specialized gustatory receptor cells for the transduction of taste stimuli. These receptor cells are sensitive to the chemicals contained within foods that are ingested, and they release neurotransmitters based on the amount of the chemical in the food. Neurotransmitters from the gustatory cells can activate sensory neurons in the facial, glossopharyngeal, and vagus cranial nerves.
Only a few recognized submodalities exist within the sense of taste, or gustation. Until recently, only four tastes were recognized: sweet, salty, sour, and bitter. Research at the turn of the 20th century led to the recognition of the fifth taste, umami, during the mid-1980s. Very recent research has suggested that there may also be a sixth taste for fats, or lipids.
Olfaction (Smell).
Did you know?
The human body can detect over 10,000 odors.
Concept Check
- Which parts of the brain are active with recording and associating scents with memories and emotions?
- Recall and list the four types of papillae (taste buds) found on the tongue.
Audition (Hearing), Equilibrium (Balance), and Somatosensation (Touch)
Watch this video:
Media 4.2 Hearing & Balance: Crash Course A&P #17 [Online video]. Copyright 2015 by CrashCourse.
Audition (Hearing)
Hearing, or audition, is the transduction of sound waves into a neural signal that is made possible by the structures of the ear (see Figure 4.1).
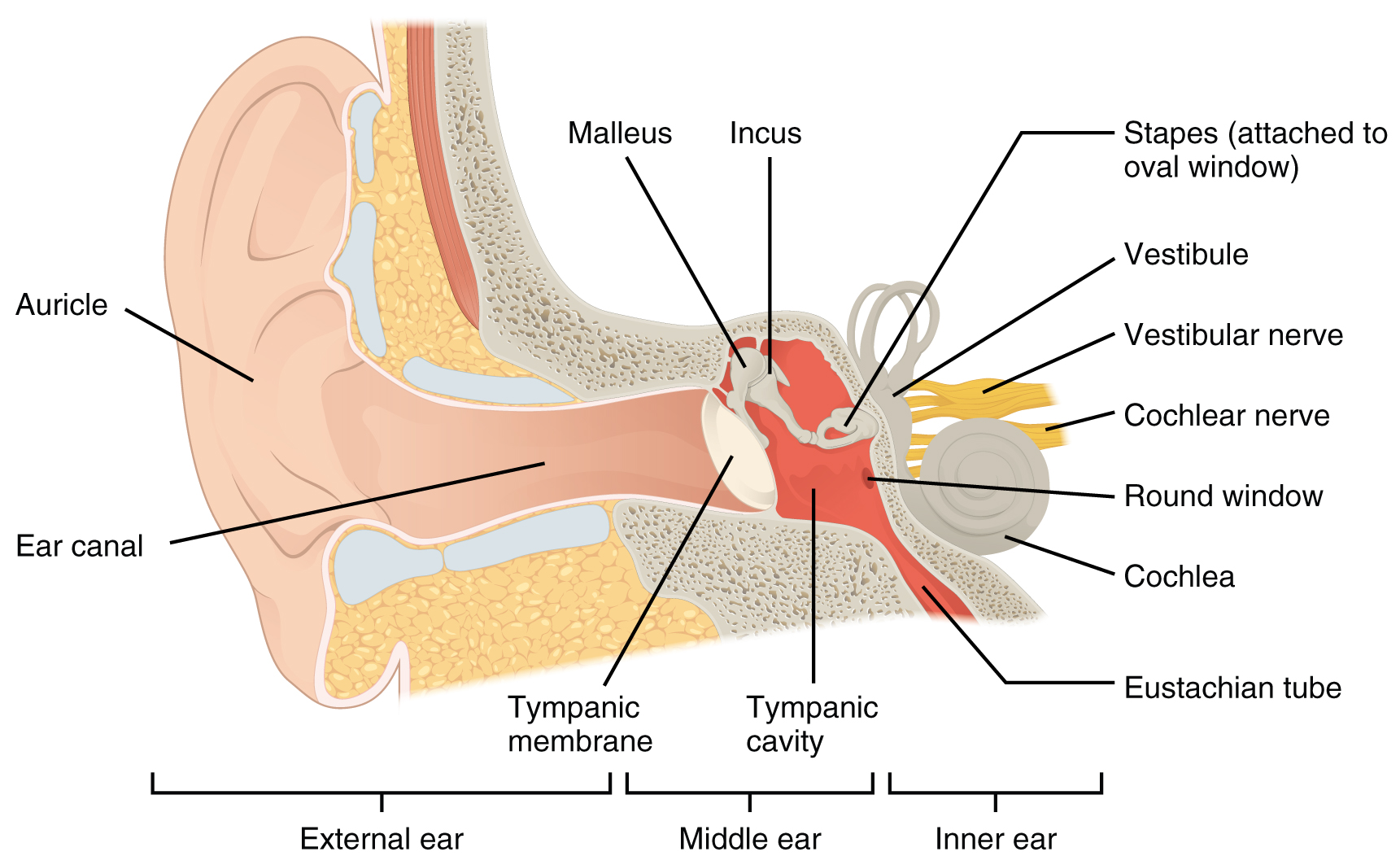
- The external ear consists of the auricle, sometimes referred to as the pinna, ear canal, and tympanic membrane.
- The C-shaped curves of the auricle direct sound waves toward the auditory canal. The canal enters the skull through the external auditory meatus of the temporal bone. At the end of the auditory canal is the tympanic membrane, which vibrates after it is struck by sound waves.
- The middle ear consists of the ossicles, oval window, and tympanic membrane.
- The three ossicles are the malleus, incus, and stapes, which are Latin names that roughly translate to hammer, anvil, and stirrup. The malleus is attached to the tympanic membrane and articulates with the incus. The incus, in turn, articulates with the stapes. The stapes is then attached to the inner ear, where the sound waves will be transduced into a neural signal. Vibrations of the ossicles travel through the oval window, moving fluid in a wave-like motion. The frequency of the fluid waves matches the frequencies of the sound waves. The middle ear is connected to the pharynx through the Eustachian tube, which helps equilibrate air pressure across the tympanic membrane. The tube is normally closed but will pop open when the muscles of the pharynx contract during swallowing or yawning.
- The inner ear is often described as a bony labyrinth, as it is composed of a series of canals embedded within the temporal bone.
- It consists of the cochlea that is responsible for hearing and the vestibule that is responsible for balance. The neural signals from these two regions are relayed to the brain stem through separate fiber bundles. However, these two distinct bundles travel together from the inner ear to the brain stem as the vestibulocochlear nerve. Sound is transduced into neural signals within the cochlear region of the inner ear, which contains the sensory neurons of the spiral ganglia. These ganglia are located within the spiral-shaped cochlea of the inner ear. The cochlea is attached to the stapes through the oval window.
The image below is a cross-sectional view of the cochlea that shows the scala vestibuli and scala tympani run along both sides of the cochlear duct (Figure 4.2). The cochlear duct contains several organs of Corti, which transduce the wave motion of the two scalas into neural signals. The organs of Corti lie on top of the basilar membrane, which is the side of the cochlear duct located between the organs of Corti and the scala tympani. As the fluid waves move through the scala vestibuli and scala tympani, the basilar membrane moves at a specific spot, depending on the frequency of the waves. Higher frequency waves move the region of the basilar membrane that is close to the base of the cochlea. Lower frequency waves move the region of the basilar membrane that is near the tip of the cochlea.
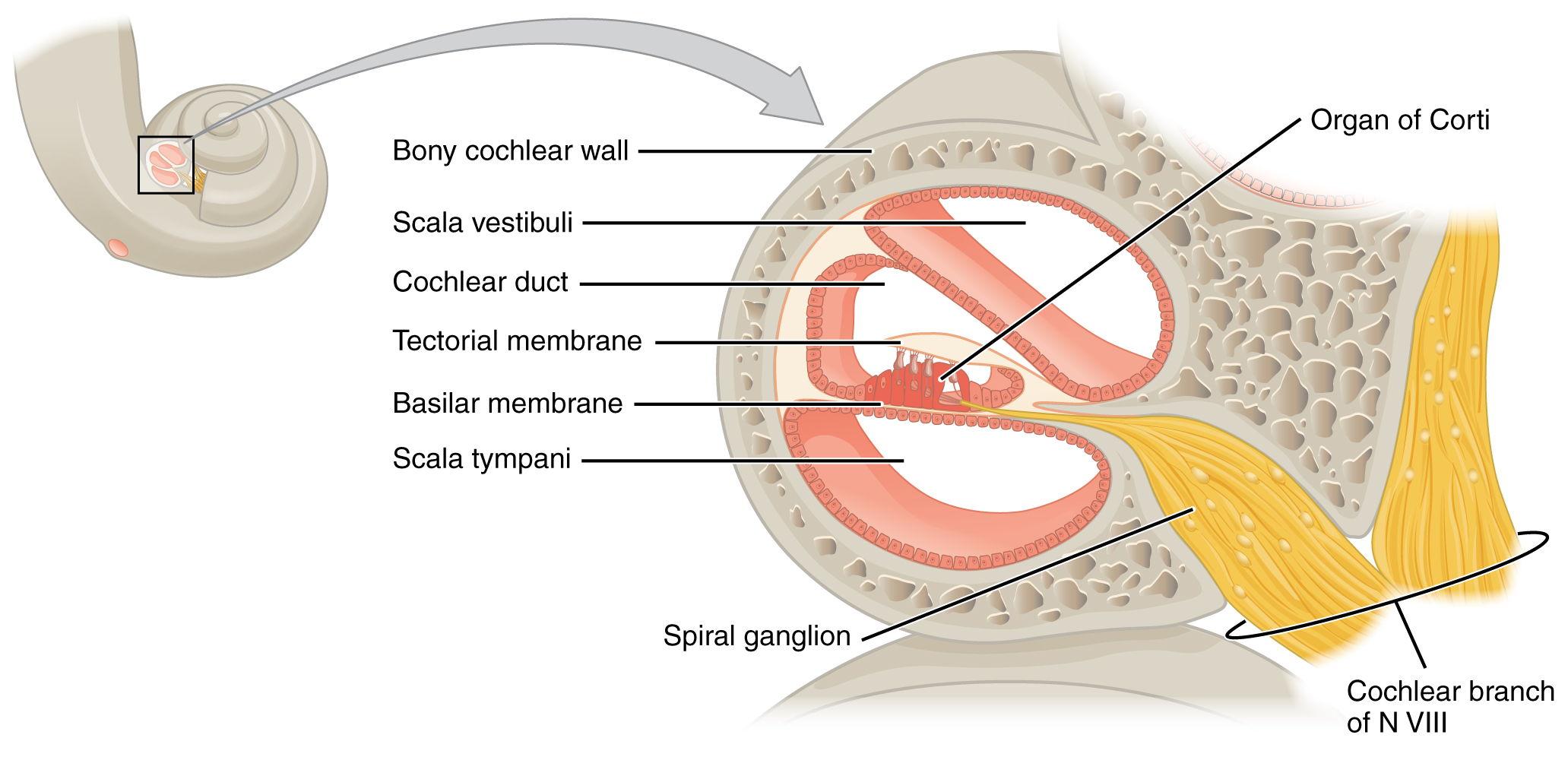
The cochlea encodes auditory stimuli for frequencies between 20 and 20,000 hertz (Hz), which is the range of sound that human ears can detect. The unit of Hz measures the frequency of sound waves in terms of cycles produced per second. Frequencies as low as 20 Hz are detected by hair cells at the apex, or tip, of the cochlea. Frequencies in the higher ranges of 20 kHz are encoded by hair cells at the base of the cochlea, close to the round and oval windows. Most auditory stimuli contain a mixture of sounds at a variety of frequencies and intensities (represented by the amplitude of the sound wave). The hair cells along the length of the cochlear duct, which are each sensitive to a particular frequency, allow the cochlea to separate auditory stimuli by frequency, just as a prism separates visible light into its component colors.
Did you know?
Sound travels at a speed of 1,130 feet per second.
Equilibrium (Balance)
Somatosensation (Touch)
Somatosensation is considered a general sense, as opposed to the special senses discussed in this section. Somatosensation is the group of sensory modalities that are associated with touch, proprioception, and interoception. These modalities include pressure, vibration, light touch, tickle, itch, temperature, pain, proprioception, and kinesthesia. This means that its receptors are not associated with a specialized organ, but are instead spread throughout the body in a variety of organs. Many of the somatosensory receptors are located in the skin, but receptors are also found in muscles, tendons, joint capsules, ligaments, and in the walls of visceral organs.
The two types of somatosensory signals that are transduced by free nerve endings are pain and temperature. Temperature receptors are stimulated when local temperatures differ from body temperature. Some thermoreceptors are sensitive to just cold and others to just heat. Nociception is the sensation of potentially damaging stimuli. Mechanical, chemical, or thermal stimuli beyond a set threshold will elicit painful sensations. Stressed or damaged tissues release chemicals that activate receptor proteins in the nociceptors.
For example, the sensation of heat associated with spicy foods involves capsaicin, the active molecule in hot peppers. Capsaicin molecules bind to a transmembrane ion channel in nociceptors that is sensitive to temperatures above 37°C (98.6°F). The dynamics of capsaicin binding with this transmembrane ion channel are unusual in that the molecule remains bound for a long time. Because of this, it will decrease the ability of other stimuli to elicit pain sensations through the activated nociceptor. For this reason, capsaicin can be used as a topical analgesic, such as in products such as Icy Hot™.
Did you know?
With the aging process, humans lose sensory receptors cells, including cells that detect pain and temperature changes.
Concept Check
- What structure exists within the ear to assist with maintaining equilibrium?
- What are the medical terms used to describe the sense of taste and touch?
Ear Anatomy Labeling Activity
Vision (Sight)
Watch this video:
Media 4.3 Vision: Crash Course A&P #18 [Online video]. Copyright 2015 by CrashCourse.
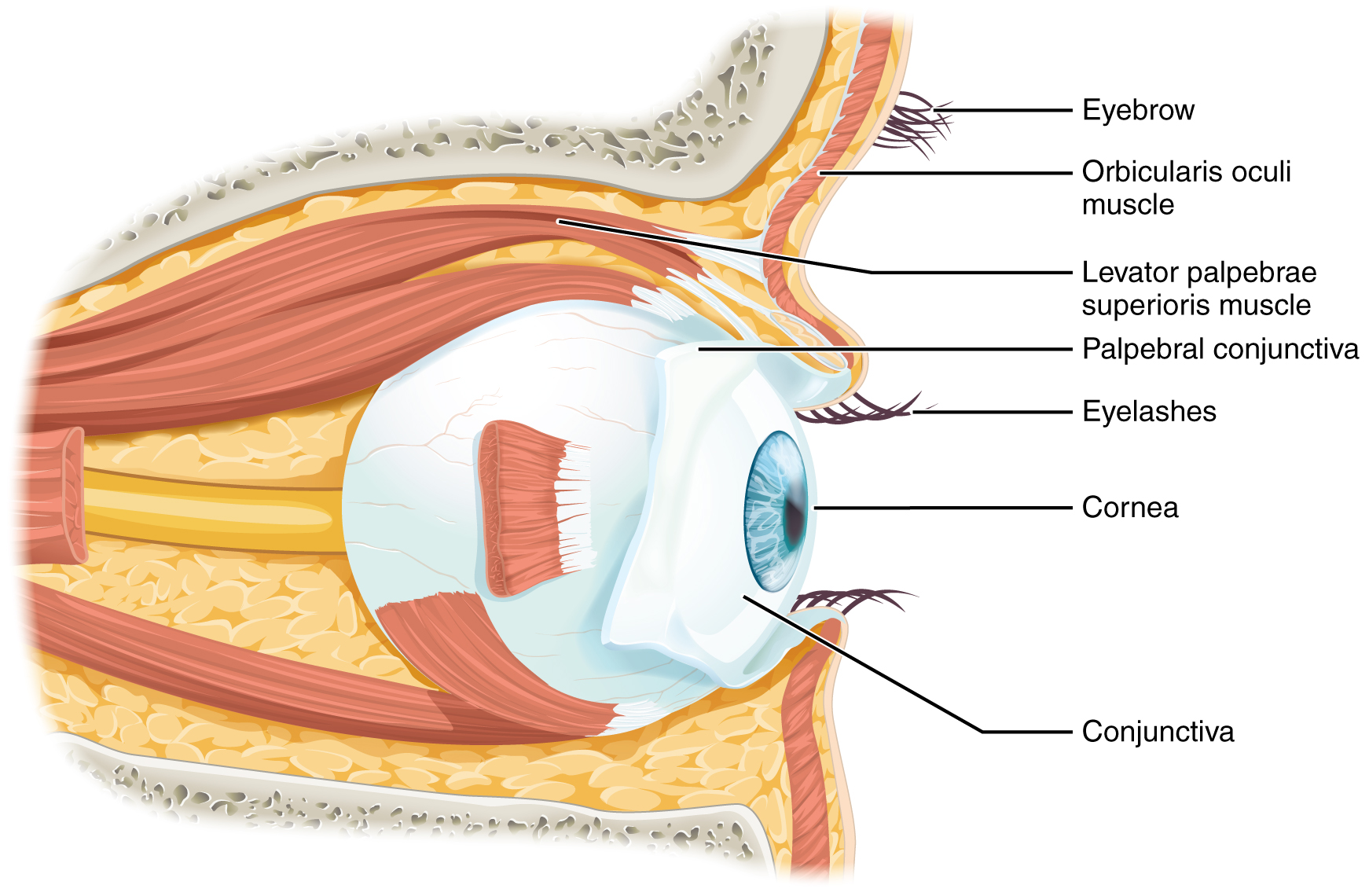
Vision is the special sense of sight that is based on the transduction of light stimuli received through the eyes. The eyes are located within either orbit in the skull. The bony orbits surround the eyeballs, protecting them and anchoring the soft tissues of the eye (see Figure 4.4). The eyelids, with lashes at their leading edges, help to protect the eye from abrasions by blocking particles that may land on the surface of the eye.
The inner surface of each lid is a thin membrane known as the palpebral conjunctiva. The conjunctiva extends over the sclera, connecting the eyelids to the eyeball. Tears are produced by the lacrimal gland, located beneath the lateral edges of the nose. Tears produced by this gland flow through the lacrimal duct to the medial corner of the eye where the tears flow over the conjunctiva, washing away foreign particles.
Movement of the eye within the orbit is accomplished by the contraction of six extraocular muscles that originate from the bones of the orbit and insert into the surface of the eyeball. Four of the muscles are arranged at the cardinal points around the eye and are named for those locations. They are the:
- superior rectus
- medial rectus
- inferior rectus
- lateral rectus.
When each of these muscles contracts, the eye moves toward the contracting muscle. For example, when the superior rectus contracts, the eye rotates to look up.
The eye itself is a hollow sphere composed of three layers of tissue:
- The outermost layer is the fibrous tunic, which includes the white sclera and clear cornea. The sclera accounts for five-sixths of the surface of the eye, most of which is not visible, though humans are unique compared with many other species in having so much of the “white of the eye” visible (see Figure 4.5). The transparent cornea covers the anterior tip of the eye and allows light to enter the eye.
- The middle layer of the eye is the vascular tunic, which is mostly composed of the choroid, ciliary body, and iris. The choroid is a layer of highly vascularized connective tissue that provides a blood supply to the eyeball. The choroid is posterior to the ciliary body, a muscular structure that is attached to the lens by zonule fibers. These two structures bend the lens, allowing it to focus light on the back of the eye. Overlaying the ciliary body, and visible in the anterior eye, is the iris—the colored part of the eye. The iris is a smooth muscle that opens or closes the pupil, which is the hole at the center of the eye that allows light to enter. The iris constricts the pupil in response to bright light and dilates the pupil in response to dim light.
- The innermost layer of the eye is the neural tunic, or retina, which contains the nervous tissue responsible for photoreception.
The eye is also divided into two cavities:
- The anterior cavity
- The anterior cavity is the space between the cornea and lens, including the iris and ciliary body. It is filled with a watery fluid called the aqueous humor.
- The posterior cavity
- The posterior cavity is the space behind the lens that extends to the posterior side of the interior eyeball, where the retina is located. The posterior cavity is filled with a more viscous fluid called the vitreous humor.
The retina is composed of several layers and contains specialized cells for the initial processing of visual stimuli. The photoreceptors (rods and cones) change their membrane potential when stimulated by light energy. The change in membrane potential alters the number of neurotransmitters that the photoreceptor cells release onto bipolar cells in the outer synaptic layer. It is the bipolar cell in the retina that connects a photoreceptor to a retinal ganglion cell (RGC) in the inner synaptic layer. There, amacrine cells additionally contribute to retinal processing before an action potential is produced by the RGC. The axons of RGCs, which lie at the innermost layer of the retina, collect at the optic disc and leave the eye at the optic nerve (see Figure 4.5). Because these axons pass through the retina, there are no photoreceptors at the very back of the eye where the optic nerve begins. This creates a “blind spot” in the retina and a corresponding blind spot in our visual field.
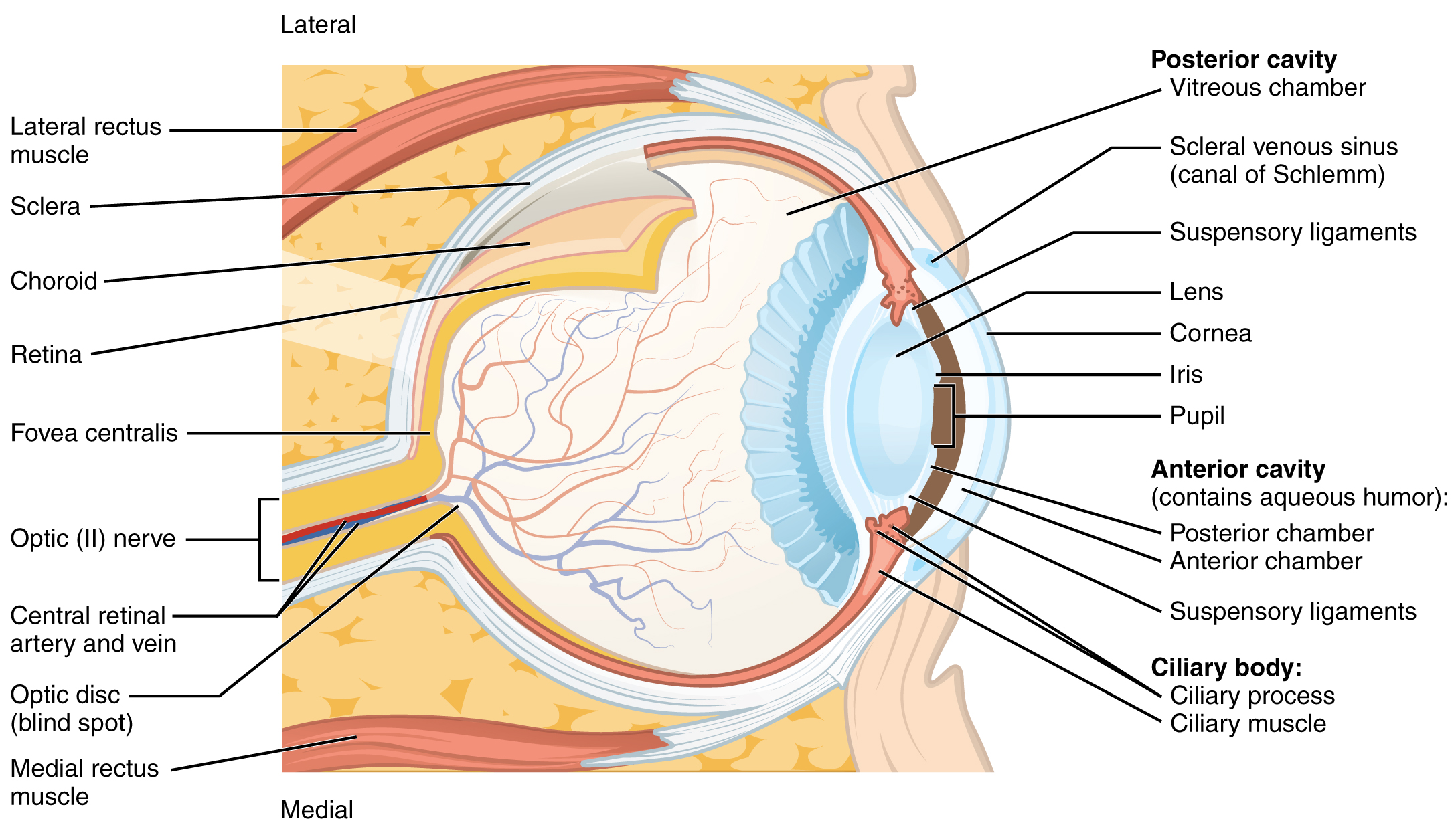
Photoreceptors in the retina (rods and cones) are located behind the axons, RGCs, bipolar cells, and retinal blood vessels. A significant amount of light is absorbed by these structures before the light reaches the photoreceptor cells. At the exact center of the retina is a small area known as the fovea. At the fovea, the retina lacks the supporting cells and blood vessels, and only contains photoreceptors. Therefore, visual acuity is greatest at the fovea. This is because the fovea is where the least amount of incoming light is absorbed by other retinal structures (see Figure 4.5). As one moves in either direction from this central point of the retina, visual acuity drops significantly.
Example: Visual Acuity (VA) between the fovea and peripheral retina.
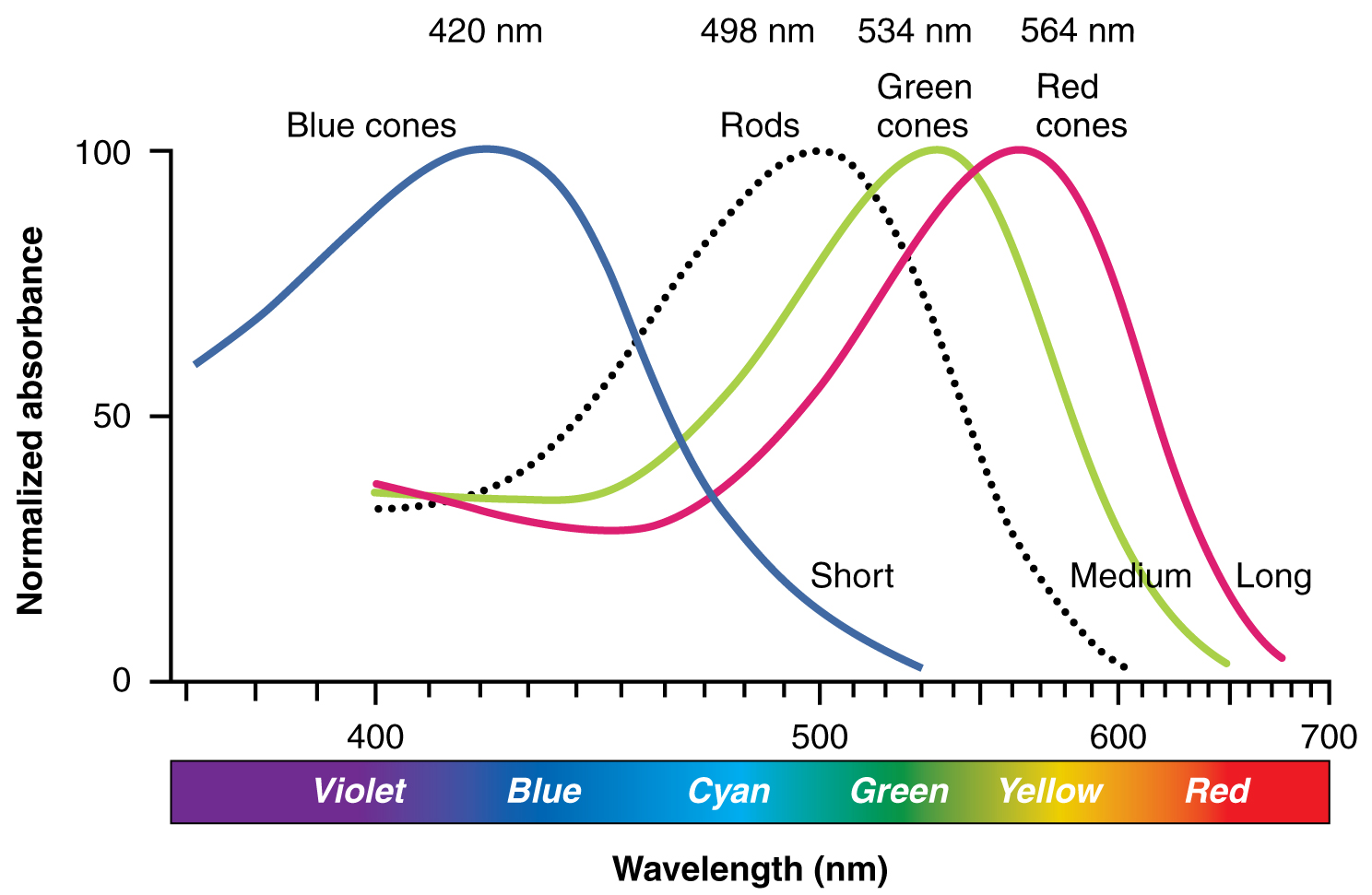
There are three types of cone opsins that are sensitive to different wavelengths of light and provide us with color vision. By comparing the activity of the three different cones, the brain can extract color information from visual stimuli (see Figure 4.6). For example, a bright blue light that has a wavelength of approximately 450 nm would activate the “red” cones minimally, the “green” cones marginally, and the “blue” cones predominantly. The relative activation of the three different cones is calculated by the brain, which perceives the color as blue. However, cones cannot react to low-intensity light, and rods do not sense the color of light. Therefore, our low-light vision is, in essence, in grayscale. In other words, in a dark room, everything appears as a shade of gray. If you think that you can see colors in the dark, it is most likely because your brain knows what color something is and is relying on that memory.
Anatomy Labeling Activity
Practice Terms Related to the Sensory Systems
Common Abbreviations for the Sensory Systems
Many terms and phrases related to the sensory systems are abbreviated. Learn these common abbreviations by expanding the list below.
Diseases and Disorders of the Sensory Systems
Olfactory Diseases and Disorders
Anosmia
Blunt force trauma to the face, such as that common in many car accidents, can lead to the loss of the olfactory nerve, and subsequently, loss of the sense of smell. This condition is known as anosmia. When the frontal lobe of the brain moves relative to the ethmoid bone, the olfactory tract axons may be sheared apart. Professional fighters often experience anosmia because of repeated trauma to the face and head. In addition, certain pharmaceuticals, such as antibiotics, can cause anosmia by killing all the olfactory neurons at once. If no axons are in place within the olfactory nerve, then the axons from newly formed olfactory neurons have no guide to lead them to their connections within the olfactory bulb. There are temporary causes of anosmia, as well, such as those caused by inflammatory responses related to respiratory infections or allergies.
Loss of the sense of smell can result in food tasting bland. A person with an impaired sense of smell may require additional spice and seasoning levels for food to be tasted. Anosmia may also be related to some presentations of mild depression, because the loss of enjoyment of food may lead to a general sense of despair. The ability of olfactory neurons to replace themselves decreases with age, leading to age-related anosmia. This explains why some older adults salt their food more than younger people do. However, this increased sodium intake can increase blood volume and blood pressure, increasing the risk of cardiovascular diseases in older adults.
Ears, Nose, and Throat Diseases and Disorders
Otitis Media
Otitis Media is known as inflammation of the middle ear canal that involves the eardrum. It is commonly seen in younger children due to bacterial and viral infections. Signs and symptoms include fever, cough and cold symptoms, hearing loss, irritability, and otalgia. Treatment involves symptomatic control as well as antibiotic (amoxicillin) use if necessary (Centers for Disease Control and Prevention, n.d.-a; MedlinePlus, 2021).
Otitis Externa
Otitis Externa is inflammation of the external ear canal. It is known as swimmer’s ear because it is associated with its exposure to water. Its clinical presentation and management are the same as otitis media (Centers for Disease Control and Prevention, n.d.-b).
Conductive Hearing Loss
Conductive hearing loss occurs when something disrupts sound through the mid and outer ear, such as physical damage to the eardrum (perforation). Hearing loss can be managed with pharmacotherapy, surgery, or a combination of the two (National Institute on Aging, n.d.).
Sensorineural Hearing Loss
Sensorineural hearing loss results from damage to the neural structures. This type of hearing loss is usually permanent (National Institute on Aging, n.d.).
Tinnitus
Tinnitus is a condition in which a person hears ringing, roaring, or buzzing in their ears. It may be a symptom of earwax blocking the ear canal, hearing loss, hormonal changes in women, or a brain tumor. Although there is no cure, several treatments are available (National Institute on Deafness and Other Communication Disorders, 2017).
Otosclerosis
Otosclerosis is the hardening of the ear due to new bone formation of the inner ear ossicles. Its etiology may be related to prior measles infection, stress fractures to the tissue surrounding the inner ear, or immune disorders. Mild otosclerosis can be surgically treated (National Institute on Deafness and Other Communication Disorders, 2018).
Rhinitis
Rhinitis is inflammation of the nasal cavity mucosal lining which can lead to congestion and rhinorrhea. Potential causes include allergy, bacterial or viral infection, and exposure to chemicals. Treatment regimens include symptom management, saline sprays, and oral antihistamines (Akhouri & House, 2021).
Dacryostenosis
Dacryostenosis, also known as nasolacrimal obstruction, is an obstruction of the nasolacrimal duct. It prevents tears from draining from the eyes into the ducts and, thus, individuals have excessive tearing. Its etiology is congenital and the result of the duct not forming properly. This condition is managed via observation, as it resolves over time (usually within 1 year) (Pezzoli & Patel, 2021).
Eye Diseases and Disorders
Blindness
The term “blindness” may cover a broad spectrum of visual disability, from limited visibility to total blindness. The parameters for legal blindness are visual field is 20 degrees or narrower and/or visual acuity is 20/200 or less in both eyes even after correction (Lee & Mesfin, 2021). Many of the conditions described below lead to visual disability, low vision, and legal blindness.
Cataract
A cataract is a clouding of the normally clear lens of your eye. For people who have cataracts, it is like seeing through cloudy lenses or windows. Age-related cataracts are the most common type, although cataracts can develop as a result of a congenital condition or due to trauma. Treatment usually involves surgery to remove the clouding of the lens (Nizami & Gulani, 2021).
Conjunctivitis
Conjunctivitis is a condition involving inflammation of the conjunctiva. Common causes include allergens and bacterial and viral pathogens. The cause of conjunctivitis determines if it is transmissible from one individual to another; conjunctivitis caused by the adenovirus, for example, is highly contagious, whereas conjunctivitis caused by pollen is not. Management involves treating the underlying cause of conjunctivitis (Ryder & Benson, 2021).
Diabetic Retinopathy
Diabetic retinopathy is a disease of the retina caused by diabetes mellitus. The retinal veins dilate, leading to swelling as fluid leaks from blood vessels into the retina. It is estimated that 77% of patients with type 1 diabetes and 25% of patients with type 2 diabetes have diabetic retinopathy. Management involves controlling the patient’s diabetes (Shukla & Tripathy, 2021).
Glaucoma
Glaucoma is a condition in which increased pressure in the eye leads to progressive vision loss. It is the second most common cause of permanent blindness in the United States. The most common form of glaucoma is primary open-angle glaucoma. This form is associated with elevated pressure caused by a backup of fluid in the eye. Management depends on the type of glaucoma and the severity of the case. Glaucoma-related vision loss cannot be reversed (Dietze et al., 2021).
Macular Degeneration/ Age-related Macular Degeneration (AMD)
Macular degeneration is the progressive damage of a portion of the retina known as the macula. Severe central vision is lost with peripheral vision retained. Macular degeneration is the leading cause of blindness in people over the age of 60 years (Ruia & Kaufman, 2021).
Nystagmus
Nystagmus is a condition whereby involuntary repetitive movements of one or both eyes make it impossible to fixate on a single object (Sekhon et al., 2020).
Retinal Detachment
Retinal detachment occurs when the retina gets pulled away or separated from its normal position. Signs and symptoms include flashing lights, floaters, and vision loss. Treatment generally involves surgery. If left untreated, a retinal detachment can lead to blindness (Blair & Czyz, 2021).
Strabismus
Strabismus is a condition where the affected eye rotates due to mismatched eye coordination. Each eye is focused differently as described below:
- Esotropia: the convergence of one or both eyes medially.
- Exotropia: the deviation of one eye laterally.
- Hypertropia: the deviation of one eye superiorly.
- Hypotropia: the deviation of one eye inferiorly.
If not managed, the brain may reject input from one eye, resulting in amblyopia. Also known as lazy eye, amblyopia is caused when there is an imbalance of stimuli from the brain to the eyes (one eye receives more than the other). It usually occurs in childhood and requires early intervention to rectify this condition (New York State Department of Health, 2012).
Medical Terms in Context
Medical Specialties and Procedures Related to the Sensory Systems
Several medical specialties support the sensory systems. An optometrist is an eye specialist that examines and evaluates for ocular pathology and prescribes corrective lenses. An ophthalmologist evaluates and manages eye pathology as well as performs surgery. An otorhinolaryngologist (ENT) is a physician that specializes in ears, nose, and throat treatment and conditions. An audiologist evaluates and manages individuals with hearing loss.
Sensory Systems Vocabulary
Acoustic neuroma
A benign tumor of the vestibular nerve in the internal auditory canal.
Anisocoria
Condition of unequal pupil size.
Anosmia
Loss of the sense of smell.
Aphakia
Condition of no lens.
Audiologist
Specialist who studies, diagnoses, and treats hearing-related issues.
Audiology
Medical specialty that studies hearing and hearing impairment.
Audiometry
The testing of the acuity of the sense of hearing.
Binocular
The use of both eyes to create one composite image.
Blepharitis
Inflammation of eyelids.
Blepharoplasty
Surgical repair of the eyelid.
Blepharoptosis
Drooping of the upper eyelid.
Cataract
A condition in which the lens of the eye becomes cloudy.
Conjunctivitis
Inflammation or infection of the conjunctiva; also called pinkeye.
Dacryocystitis
Inflammation of the tear (lacrimal) sac.
Dacryocystorhinostomy
Creation of an artificial opening between the lacrimal sac and the nose (to restore drainage).
Diplopia
Double vision.
Endophthalmitis
Inflammation within the eye.
Epistaxis
Nosebleed.
Hyperopia
Farsightedness.
Iridectomy
Excision of part of the iris.
Iritis
Inflammation of the iris.
Keratitis
Inflammation of the cornea.
Keratomalacia
Degeneration of the cornea.
Keratoplasty
Surgical replacement of the cornea.
Kinesthesia
Sense of body movement based on sensation in the skeletal muscles, tendons, joints, and the skin.
Labyrinthitis
Inflammation of the inner ear (labyrinth).
Mastoidectomy
Excision of the mastoid bone.
Mastoiditis
Inflammation of the mastoid bone.
Mechanoreceptor
A sensory neuron that responds to mechanical pressure.
Myopia
Nearsightedness.
Myringoplasty
Surgical repair of the tympanic membrane.
Nasopharyngeal
Pertaining to the nose and pharynx (throat).
Nociceptors
Sensory neurons that respond to pain.
Ophthalmia neonatorum
Conjunctivitis in newborns (severe).
Ophthalmologist
A doctor who has special training in diagnosing and treating eye problems.
Ophthalmology
A surgical specialty focused on the structure, function, and surgery of the eye.
Ophthalmopathy
Disease of the eye.
Ophthalmoplegia
Paralysis of one or more eye muscles.
Ophthalmoscope
Instrument used to view the inside of the eye.
Ophthalmoscopy
An exam of the fundus of the eye using a magnifying lens and light.
Optometrist
A specialist who diagnoses, treats, and manages diseases and disorders of the eye.
Optometry
The professional practice of eye and vision care that involves measuring vision.
Otalgia
Pain in the ear.
Otolaryngologist.
A doctor who has special training in diagnosing and treating diseases of the ear, nose, and throat.
Otomycosis
Fungal infection of the external ear.
Otosclerosis
Hardening of the ear.
Otoscope
Instrument used to view the ear.
Otoscopy
Process of viewing the ear canal and eardrum.
Pharyngitis
Inflammation of the pharynx.
Photophobia
A condition in which the eyes are more sensitive than normal to light.
Proprioception
Sense of position and movement of the body.
Retinoblastoma
Cancer that forms in the tissues of the retina.
Retinopathy
Disease of the retina.
Retinoscopy
Process of determining the refractive state of the eye.
Rhinitis
Inflammation of the mucous membranes of the nose.
Rhinorrhea
Excess nasal drainage; also called a “runny nose.”
Sinusitis
Inflammation of the sinuses.
Stapedectomy
Excision of the stapes.
Stye
Infection of an oil gland of the eyelid (hordeolum).
Thermoreceptors
Specialized neurons that respond to changes in temperature.
Tonometer
Instrument used to measure pressure (within the eye).
Tonometry
Process of measuring pressure (within the eye).
Tonsillitis
Inflammation of the tonsils.
Tympanic membrane
Ear drum.
Tympanoplasty
Surgical repair of the tympanic membrane.
Visceral (sense)
Sense associated with the internal organs.
Visual acuity
Sharpness of vision.
Xerophthalmia
Condition of dry eye.
Test Yourself
References
Akhouri, S., & House, S. A. (2021). Allergic rhinitis. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK538186/
Blair, K., & Czyz, C. N. (2021). Retinal detachment. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK551502/
Centers for Disease Control and Prevention. (n.d.-a). Ear infection. https://www.cdc.gov/antibiotic-use/ear-infection.html
Centers for Disease Control and Prevention. (n.d.-b). Swimming and ear infections. https://www.cdc.gov/healthywater/swimming/swimmers/rwi/ear-infections.html
CrashCourse. (2015, May 11). Vision: Crash course A&P #18 [Video]. YouTube. https://www.youtube.com/watch?v=o0DYP-u1rNM
CrashCourse. (2015, April 27). Taste & smell: Crash course A&P #16 [Video]. YouTube. https://www.youtube.com/watch?v=mFm3yA1nslE
CrashCourse. (2015, May 4). Hearing & balance: Crash course A&P #17 [Video]. YouTube. https://www.youtube.com/watch?v=Ie2j7GpC4JU
Dietze, J., Blair, K., Havens, S. J. (2021). Glaucoma. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK538217/
Lee, S. Y., & Mesfin, F. B. (2021). Blindness. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK448182/
MedlinePlus. (2021). Ear infections. National Institutes of Health, U.S. Department of Health and Human Services. https://medlineplus.gov/earinfections.html
National Institute on Aging. (n.d.). Hearing loss: A common problem for older adults. National Institutes of Health, U.S. Department of Health and Human Services. https://www.nia.nih.gov/health/hearing-loss-common-problem-older-adults
National Institute on Deafness and Other Communication Disorders. (2017). Tinnitus. National Institutes of Health, U.S. Department of Health and Human Services. https://www.nidcd.nih.gov/health/tinnitus
National Institute on Deafness and Other Communication Disorders. (2018). Otosclerosis. National Institutes of Health, U.S. Department of Health and Human Services. https://www.nidcd.nih.gov/health/otosclerosis
New York State Department of Health. (2012). Types of vision problems. https://www.health.ny.gov/diseases/conditions/vision_and_eye_health/types_of_vision_problems.htm
Nizami, A. A., & Gulani, A. C. (2021). Cataract. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK539699/
Pezzoli, M., & Patel, B. C. (2021). Dacryostenosis. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK563132/
Ruia, S., & Kaufman, E. J. (2021). Macular degeneration. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK560778/
Ryder, E. C., & Benson, S. (2021). Conjunctivitis. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK541034/
Sekhon, R. K., Rocha Cabrero, F., & Deibel, J. P. (2020). Nystagmus types. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK539711/
Shukla, U. V., & Tripathy, K. (2021). Diabetic retinopathy. In StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK560805/
Image Descriptions
Figure 4.1 image description: This image shows the structure of the ear with the major parts labeled. The ear is divided up into 3 parts from left to right: external ear, middle ear, and inner ear. Labels for each part read: external ear (auricle, ear canal), middle ear (tympanic membrane, malleus, incus, tympanic cavity), inner ear (stapes, vestibule, vestibular nerve, cochlear nerve, cochlea, round window, eustachian tube). [Return to Figure 4.1].
Figure 4.2 image description: This diagram shows the structure of the cochlea in the inner ear. Labels read (from top, counterclockwise): bony cochlear wall, scala vestibuli, cochlear duct, tectorial membrane, basilar membrane, scala tympani, spiral ganglion, cochlear branch of N VIII, organ of Corti. [Return to Figure 4.2].
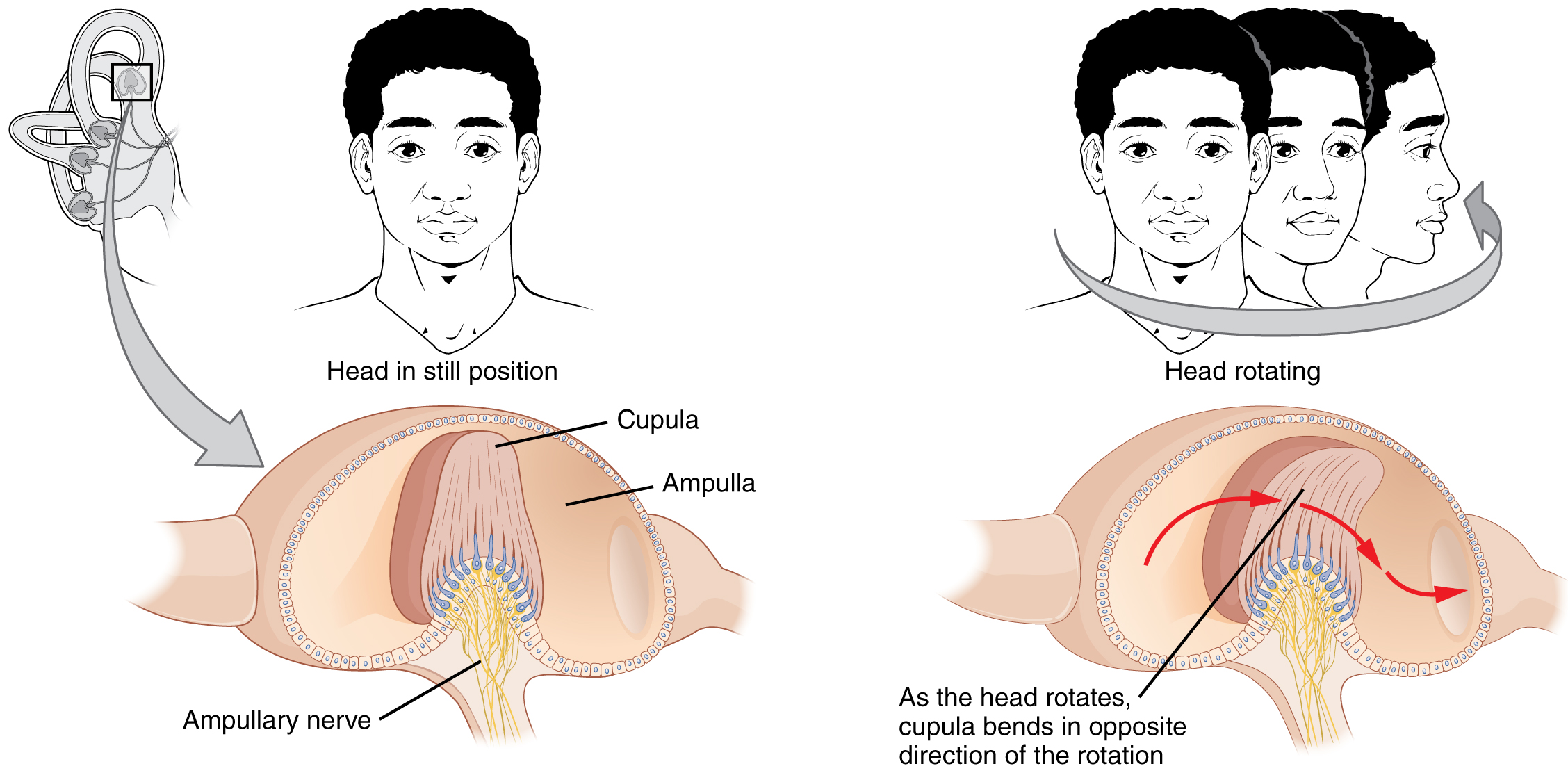
Figure 4.3 image description: The left panel of this image shows a person’s head in a still position. Underneath this, the ampullary nerve is shown. Labels read: cupula, ampulla, ampullary nerve). The right panel shows a person rotating his head, and below that, the direction of movement of the cupula is shown. Label reads: as the head rotates, cupula bends in opposite direction of the rotation. [Return to Figure 4.3].
Figure 4.4 image description: This diagram shows the lateral view of the eye. The major parts are labeled. Labels read (from top): eyebrow, orbicularis oculi muscle, levator palpebrae superioris muscle, palpebral conjunctiva, eyelashes, cornea, conjunctiva. [Return to Figure 4.4].
Figure 4.5 image description: This diagram shows a lateral and medial view of the eyeball. The major parts are labeled. Labels read (from top, clockwise): posterior cavity (vitreous chamber, scleral venous sinus (canal of Schlemm), suspensory ligaments, lens, cornea, iris, pupil); anterior cavity (contains aqueous humor, posterior chamber, anterior chamber, suspensory ligaments); Ciliary body (ciliary process and muscle), medial rectus muscle, optic disc (blind spot), central retinal artery and vein, fovea centralis, retina, choroid, sclera, lateral rectus muscle. [Return to Figure 4.5].
Figure 4.6 image description: This graph shows the normalized absorbance versus wavelength for different cell types in the eye. The Y-axis is normalized absorbance, and the X-axis is the wavelength (nm) with the colors violet, blue, cyan, green, yellow, and red across the bottom. The lines in the graph indicate blue cones which peak at 420 nm, rods that peak at 498 nm, green cones which peak at 534 nm, and red cones which peak at 564 nm. Blue cones line is labeled as short, green cones as medium, and red cones as long. [Return to Figure 4.6].

