12
Learning Objectives
- Examine the anatomy of the respiratory system
- Determine the main functions of the respiratory system
- Differentiate respiratory system medical terms and common abbreviations
- Recognize the medical specialties associated with the respiratory system
- Discover common diseases, disorders, and procedures related to the respiratory system
Respiratory System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Respiratory System.
Introduction to the Respiratory System
How long you can hold your breath as you continue reading… How long can you do it? Chances are you are feeling uncomfortable already. A typical human cannot survive without breathing for more than three minutes, and even if you wanted to hold your breath longer, your autonomic nervous system would take control. Although oxygen is critical for cells, it is the accumulation of carbon dioxide that primarily drives your need to breathe.
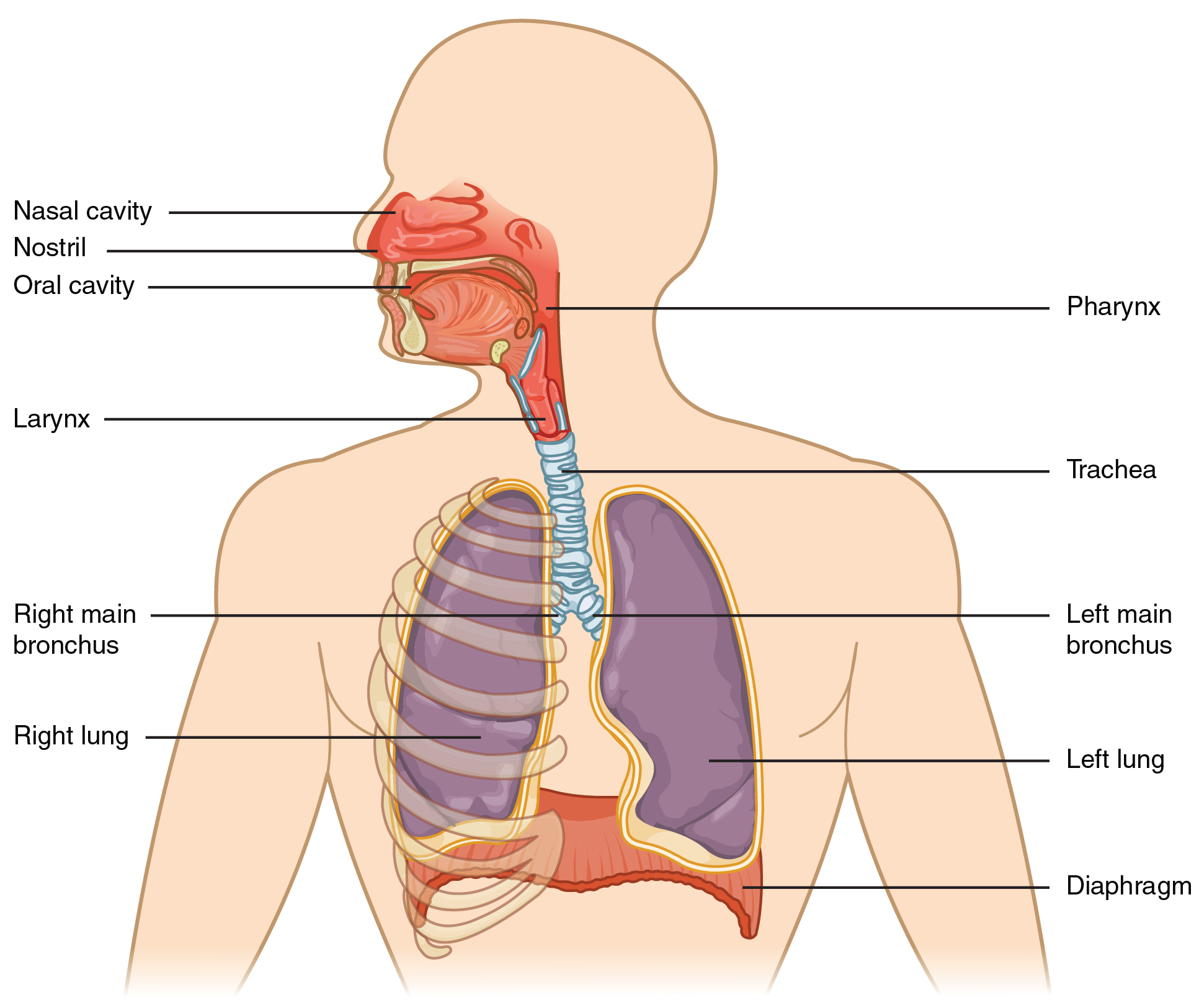
The major structures of the respiratory system function primarily to provide oxygen to body tissues for cellular respiration, remove the waste product carbon dioxide, and help to maintain acid-base balance. Portions of the respiratory system are also used for non-vital functions, such as sensing odors, speech production, and for straining, such as coughing.
Did you know?
If you hold your breath for longer than 3 minutes, your autonomic nervous system will take control.
Watch this video:
Media 12.1. Respiratory System, Part 1: Crash Course A&P #31 [Online video]. Copyright 2015 by CrashCourse.
Practice Medical Terms Related to the Respiratory System
Anatomy (Structures) of the Respiratory System
The Nose and its Adjacent Structures
The major entrance and exit for the respiratory system is through the nose. When discussing the nose, it is helpful to divide it into two major sections:
- external nose
- internal nose
The nares open into the nasal cavity, which is separated into left and right sections by the nasal septum (Figure 12.2). The nasal septum is formed anteriorly by a portion of the septal cartilage and posteriorly by the perpendicular plate of the ethmoid bone and the thin vomer bones.
Each lateral wall of the nasal cavity has three bony projections: the inferior conchae are separate bones, and the superior and middle conchae are portions of the ethmoid bone. Conchae increase the surface area of the nasal cavity, disrupting the flow of air as it enters the nose and causing air to bounce along the epithelium, where it is cleaned and warmed. The conchae and meatuses trap water during exhalation preventing dehydration.
The floor of the nasal cavity is composed of the hard palate and the soft palate. Air exits the nasal cavities via the internal nares and moves into the pharynx.
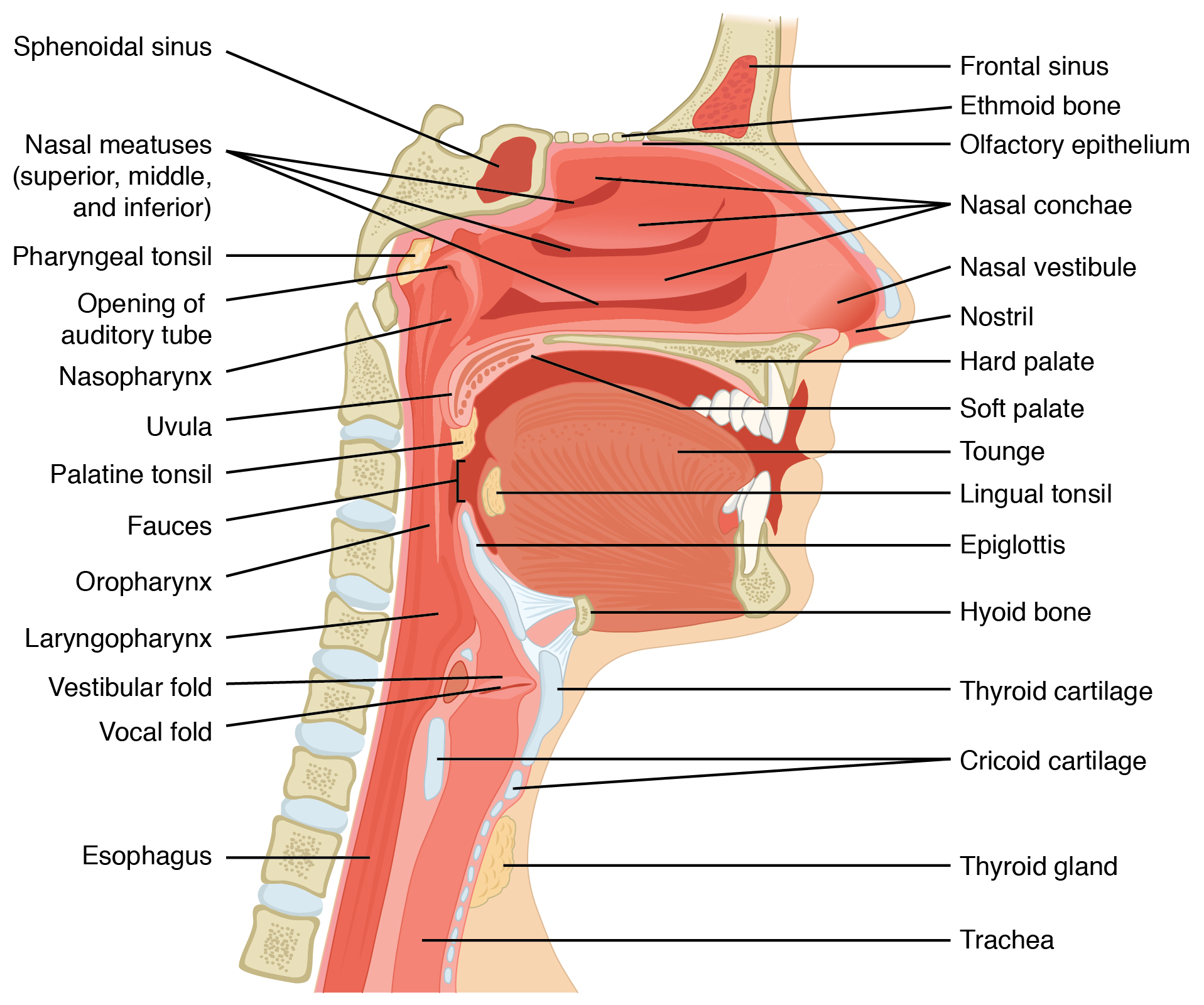
Paranasal sinuses serve to warm and humidify incoming air and are lined with a mucosa which produces mucus. Paranasal sinuses are named for their associated bone:
- frontal sinus
- maxillary sinus
- sphenoidal sinus
- ethmoidal sinus
The nares and anterior portion of the nasal cavities are lined with mucous membranes, containing sebaceous glands and hair follicles that serve to prevent the passage of large debris, such as dirt, through the nasal cavity. An olfactory epithelium used to detect odors is found deeper in the nasal cavity.
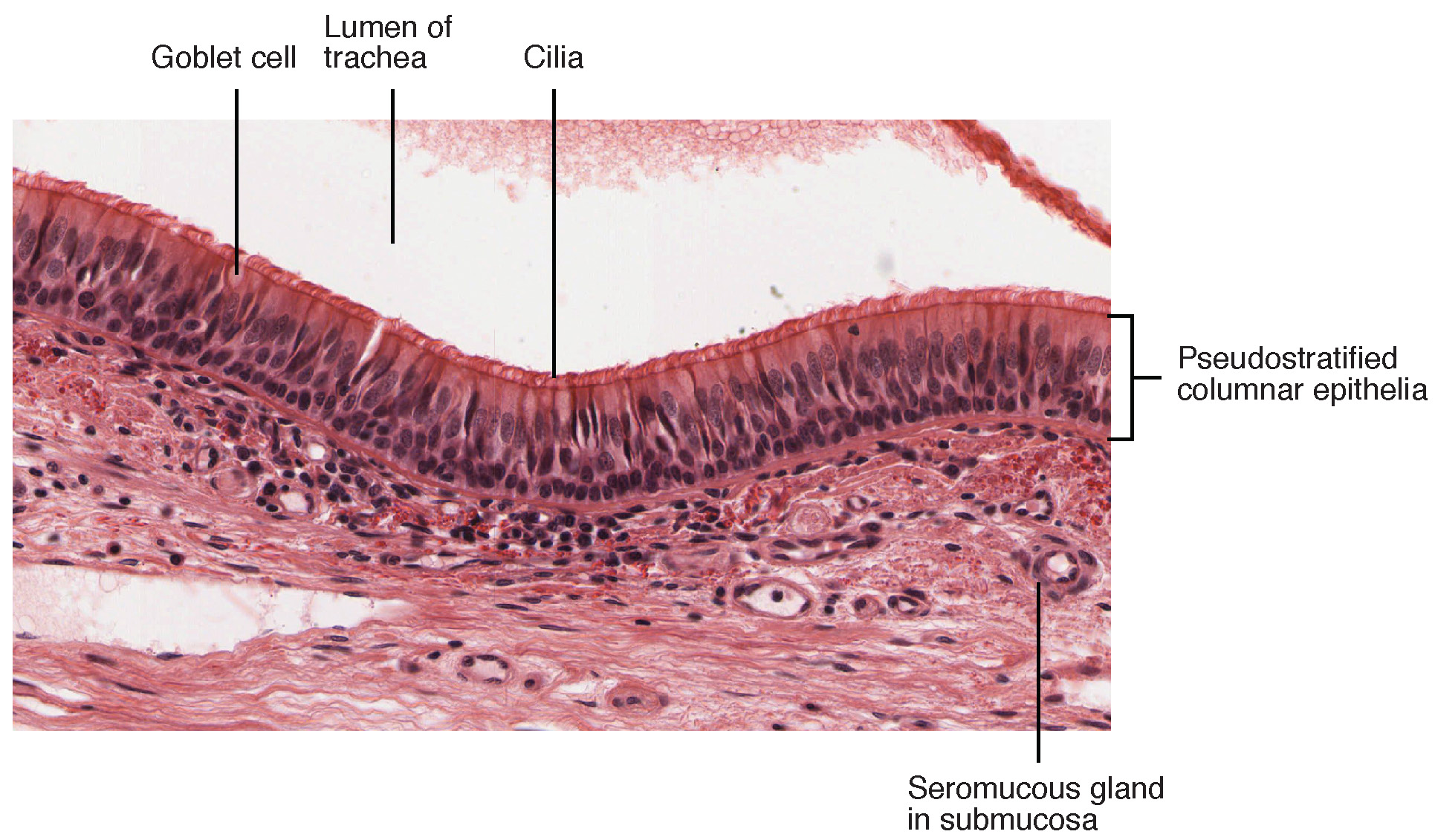
The conchae, meatuses, and paranasal sinuses are lined by respiratory epithelium composed of pseudostratified ciliated columnar epithelium (Figure 12.3). The epithelium contains specialized epithelial cells that produce mucus to trap debris. The cilia of the respiratory epithelium help to remove mucus and debris with a constant beating motion, sweeping materials towards the throat to be swallowed.
This moist epithelium functions to warm and humidify incoming air. Capillaries located just beneath the nasal epithelium warm the air by convection. Serous and mucus-producing cells also secrete defensins, or immune cells that patrol the connective tissue providing additional protection.
Did you know?
Cold air slows the movement of cilia that may result in the accumulation of mucus, leading to rhinorrhea during cold weather.
Pharynx
The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx (see Figure 12.4).
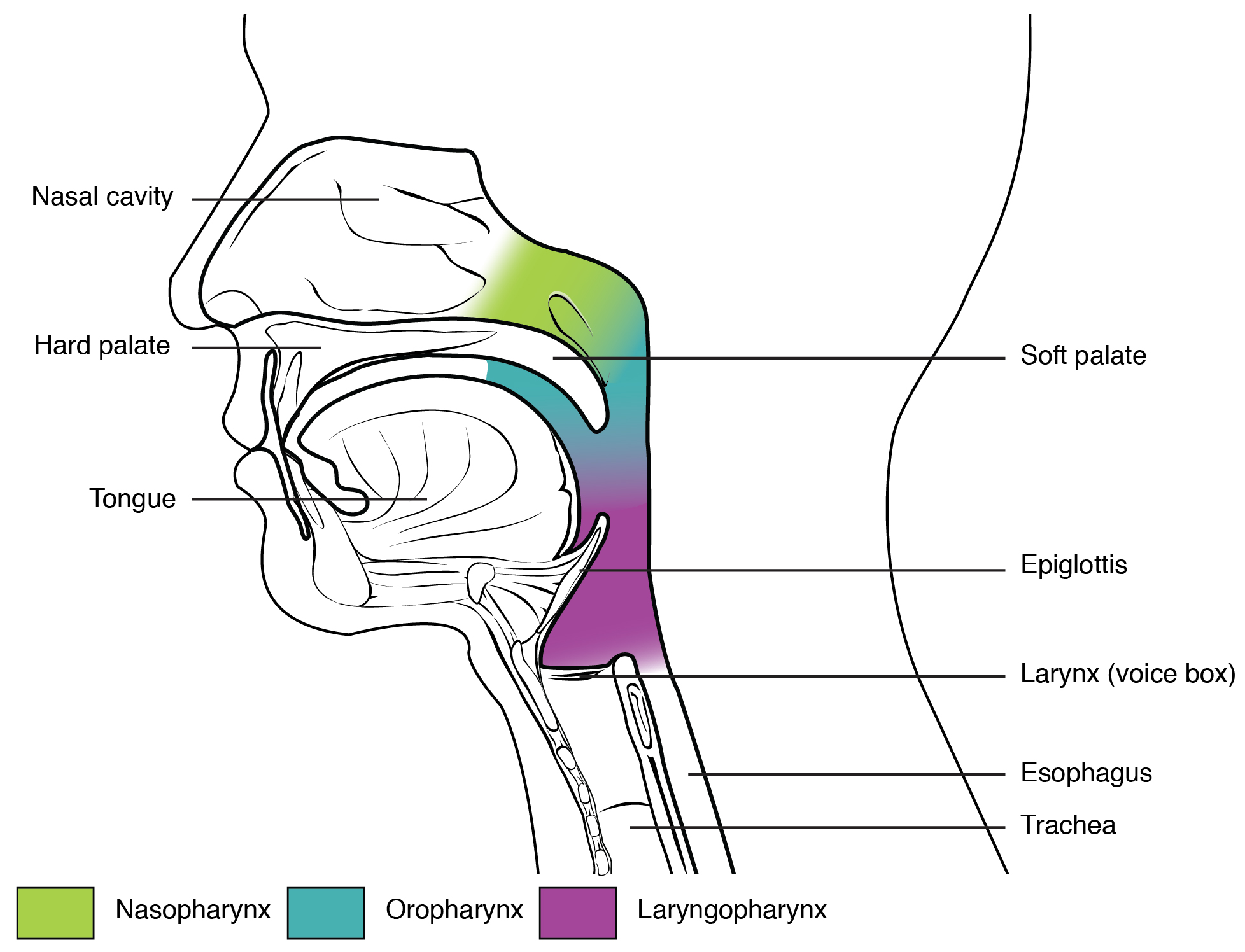
At the top of the nasopharynx are the pharyngeal tonsils. The function of the pharyngeal tonsil is not well understood, but it contains a rich supply of lymphocytes and is covered with ciliated epithelium that traps and destroys invading pathogens that enter during inhalation. The pharyngeal tonsils are large in children but tend to regress with age and may even disappear. The uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. Auditory (Eustachian) tubes that connect to each middle ear cavity open into the nasopharynx. This connection is why colds often lead to ear infections.
The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The oropharynx contains two distinct sets of tonsils:
- The palatine tonsils.
- A palatine tonsil is one of a pair of structures located laterally in the oropharynx in the area of the fauces.
- The lingual tonsils.
- The lingual tonsil is located at the base of the tongue.
Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue, and trap and destroy pathogens entering the body through the oral or nasal cavities.
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end, where the digestive and respiratory systems diverge. The stratified squamous epithelium of the oropharynx is continuous with the laryngopharynx. Anteriorly, the laryngopharynx opens into the larynx, whereas posteriorly, it enters the esophagus.
Larynx
The structure of the larynx is formed by several pieces of cartilage. Three large cartilage pieces form the major structure of the larynx.
- Thyroid cartilage (anterior):
- The thyroid cartilage is the largest piece of cartilage that makes up the larynx. The thyroid cartilage consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males.
- Epiglottis (superior):
- Three smaller, paired cartilages—the arytenoids, corniculates, and cuneiforms—attach to the epiglottis and the vocal cords and muscle that help move the vocal cords to produce speech.
- Cricoid cartilage (inferior):
- The thick cricoid cartilage forms a ring, with a wide posterior region and a thinner anterior region.
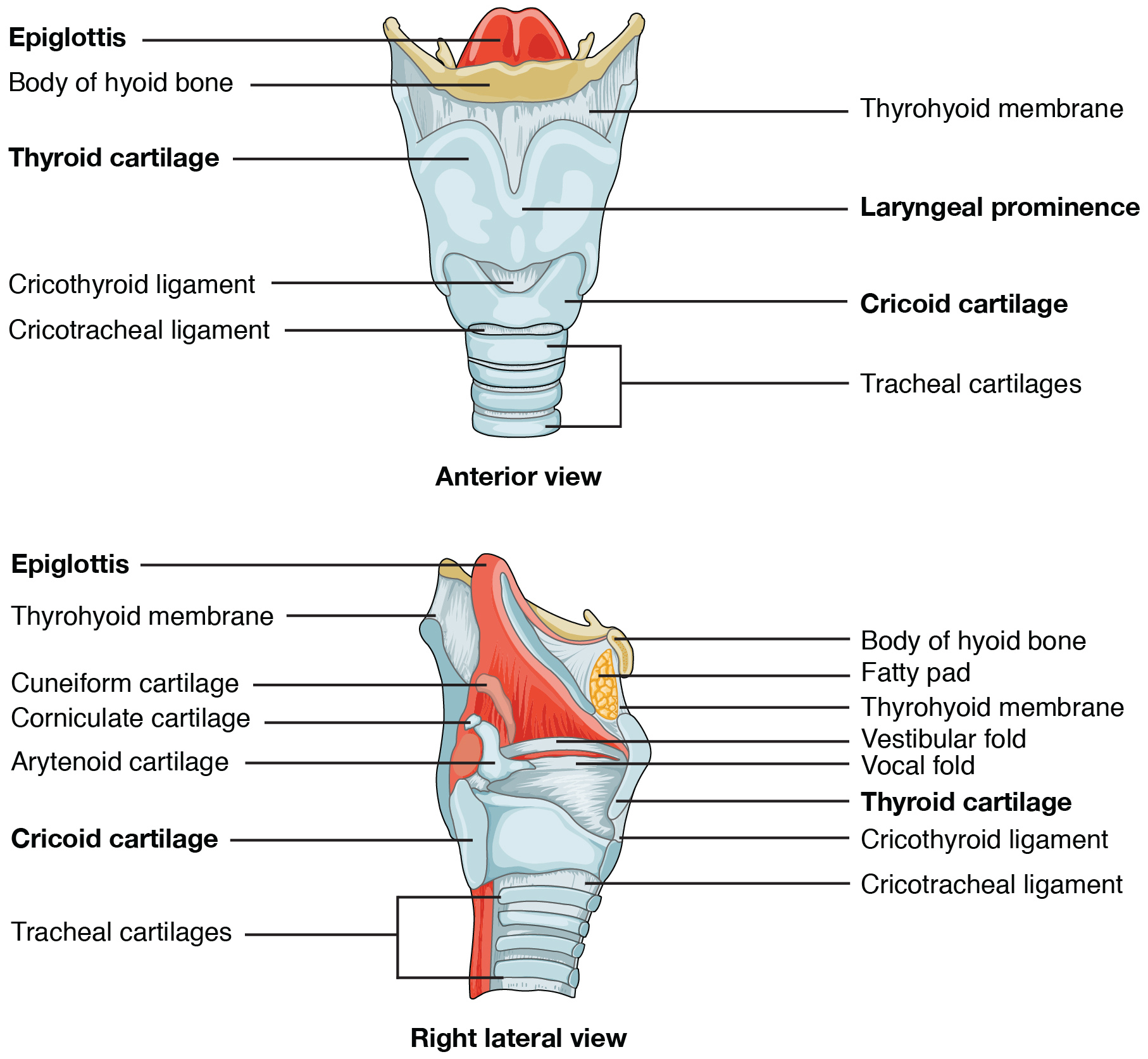
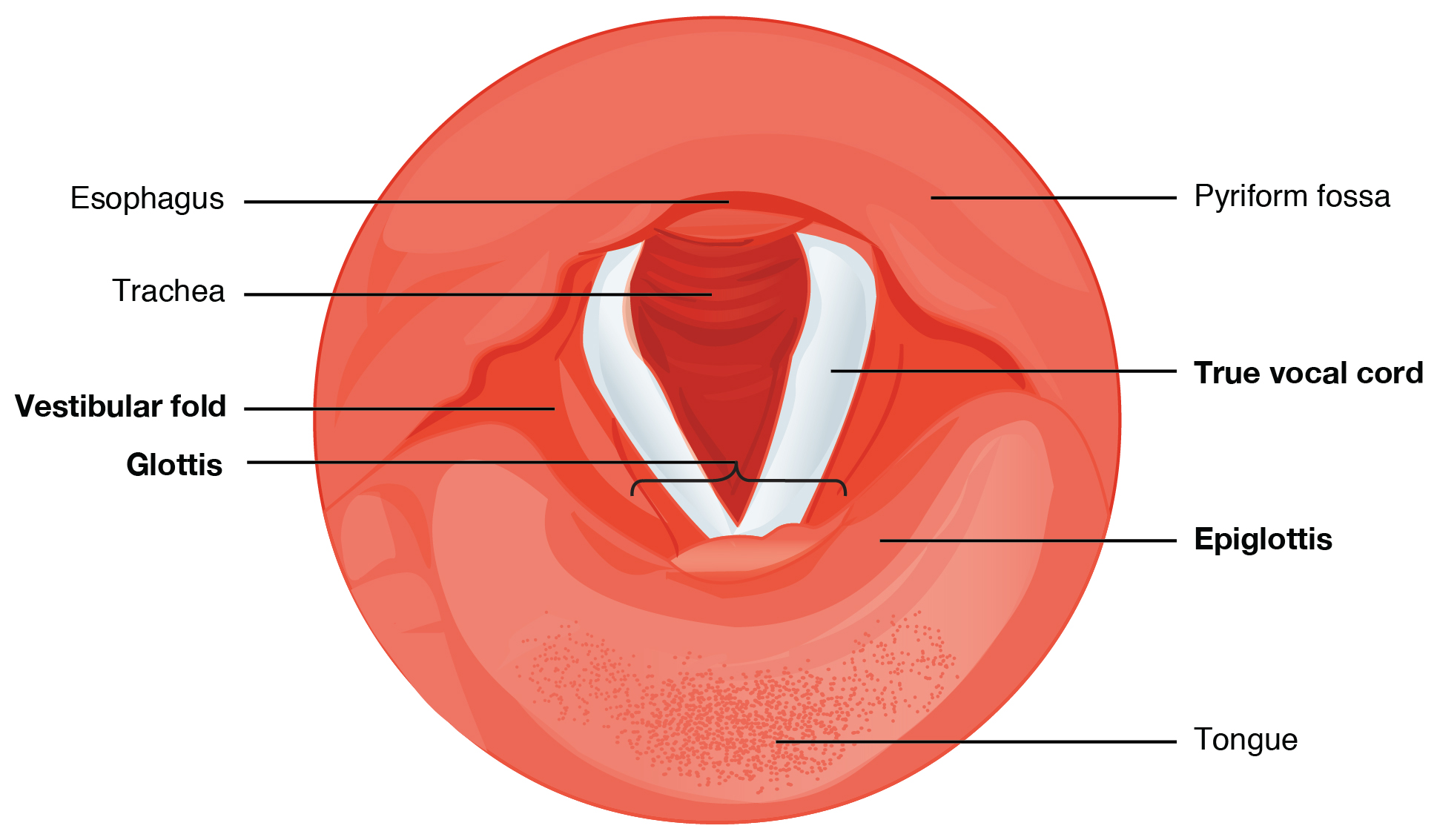
When the epiglottis is in the “closed” position, the unattached end of the epiglottis rests on the glottis. A vestibular fold, or false vocal cord, is one of a pair of folded sections of mucous membrane. A true vocal cord is one of the white, membranous folds attached by muscle to the thyroid and arytenoid cartilages of the larynx on their outer edges. The inner edges of the true vocal cords are free, allowing oscillation to produce sound.
The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea. These movements produce a larger area for food to pass through, while preventing food and beverages from entering the trachea.
Similar to the nasal cavity and nasopharynx, this specialized epithelium produces mucus to trap debris and pathogens as they enter the trachea. The cilia beat the mucus upward towards the laryngopharynx, where it can be swallowed down the esophagus.
Did you know?
Folds of the true vocal cords differ between individuals resulting in voices with different pitches.
Trachea
The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue. The trachealis muscle and elastic connective tissue together form the fibroelastic membrane. The fibroelastic membrane allows the trachea to stretch and expand slightly during inhalation and exhalation, whereas the rings of cartilage provide structural support and prevent the trachea from collapsing. The trachealis muscle can be contracted to force air through the trachea during exhalation. The trachea is lined with pseudostratified ciliated columnar epithelium, which is continuous with the larynx. The esophagus borders the trachea posteriorly.
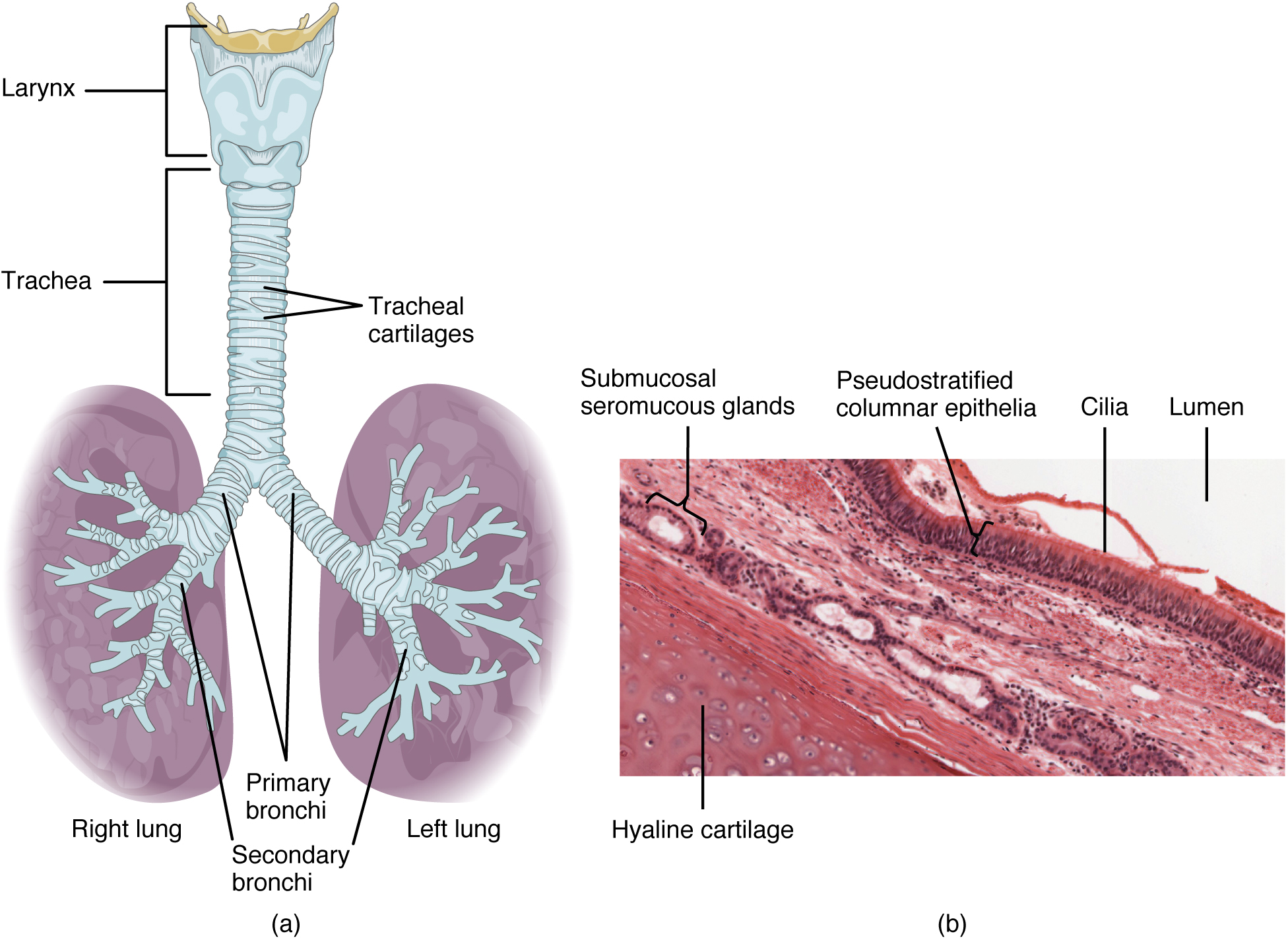
Bronchial Tree
The trachea branches into the right and left primary bronchi at the carina. These bronchi are also lined by pseudostratified ciliated columnar epithelium containing mucus-producing goblet cells (Figure 12.7b). The carina is a raised structure that contains specialized nervous tissue that induces violent coughing if a foreign body, such as food, is present. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse. The primary bronchi enter the lungs at the hilum. The bronchi continue to branch into a bronchial tree. A bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchi. The main function of the bronchi, like other conducting zone structures, is to provide a passageway for air to move into and out of each lung. The mucous membrane traps debris and pathogens.
A bronchiole branches from the tertiary bronchi. Bronchioles, which are about 1 mm in diameter, further branch until they become the tiny terminal bronchioles, which lead to the structures of gas exchange. There are more than 1,000 terminal bronchioles in each lung. The muscular walls of the bronchioles do not contain cartilage like those of the bronchi. This muscular wall can change the size of the tubing to increase or decrease airflow through the tube.
Respiratory Zone
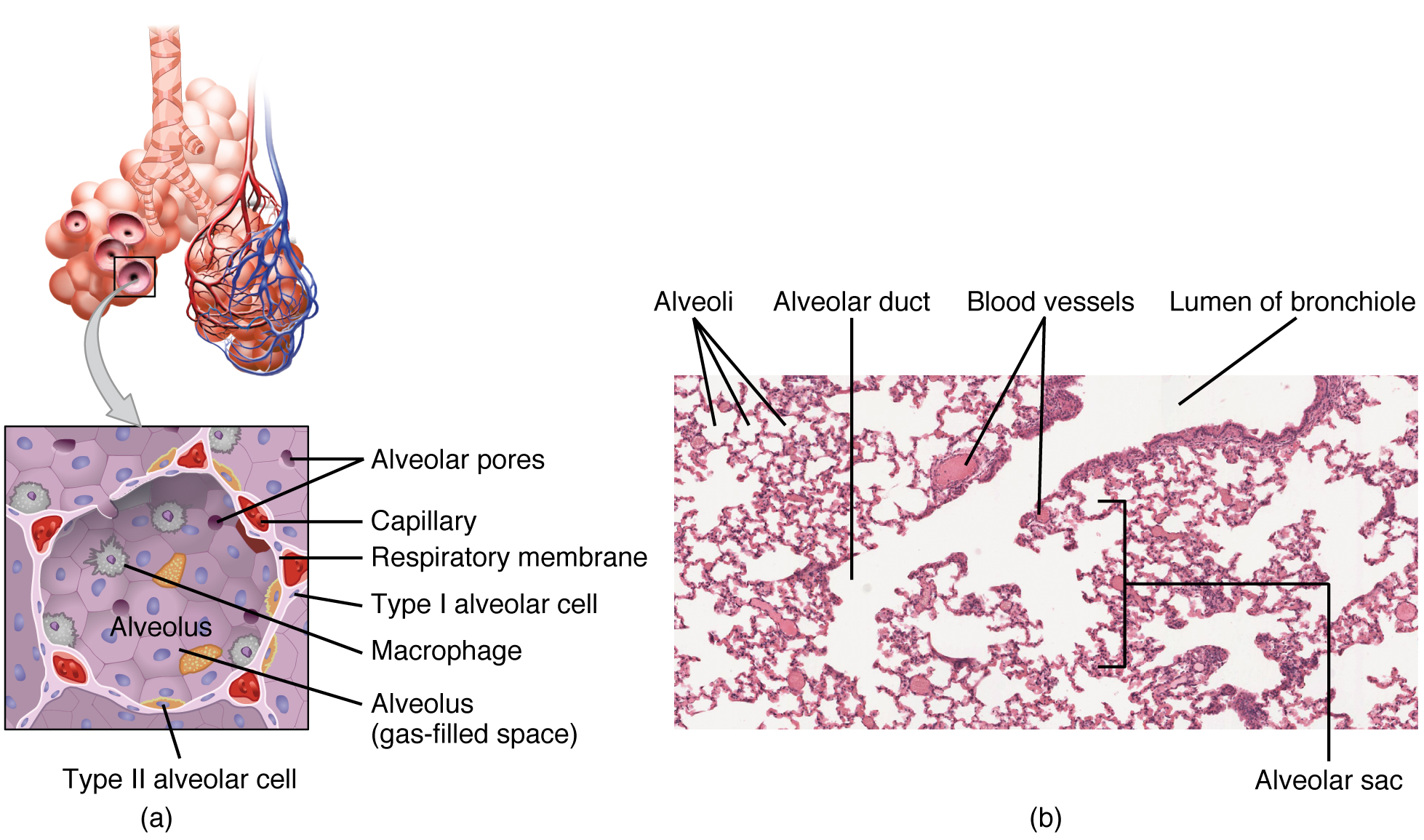
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole (see Figure 12.8), which then leads to an alveolar duct, opening into a cluster of alveoli.
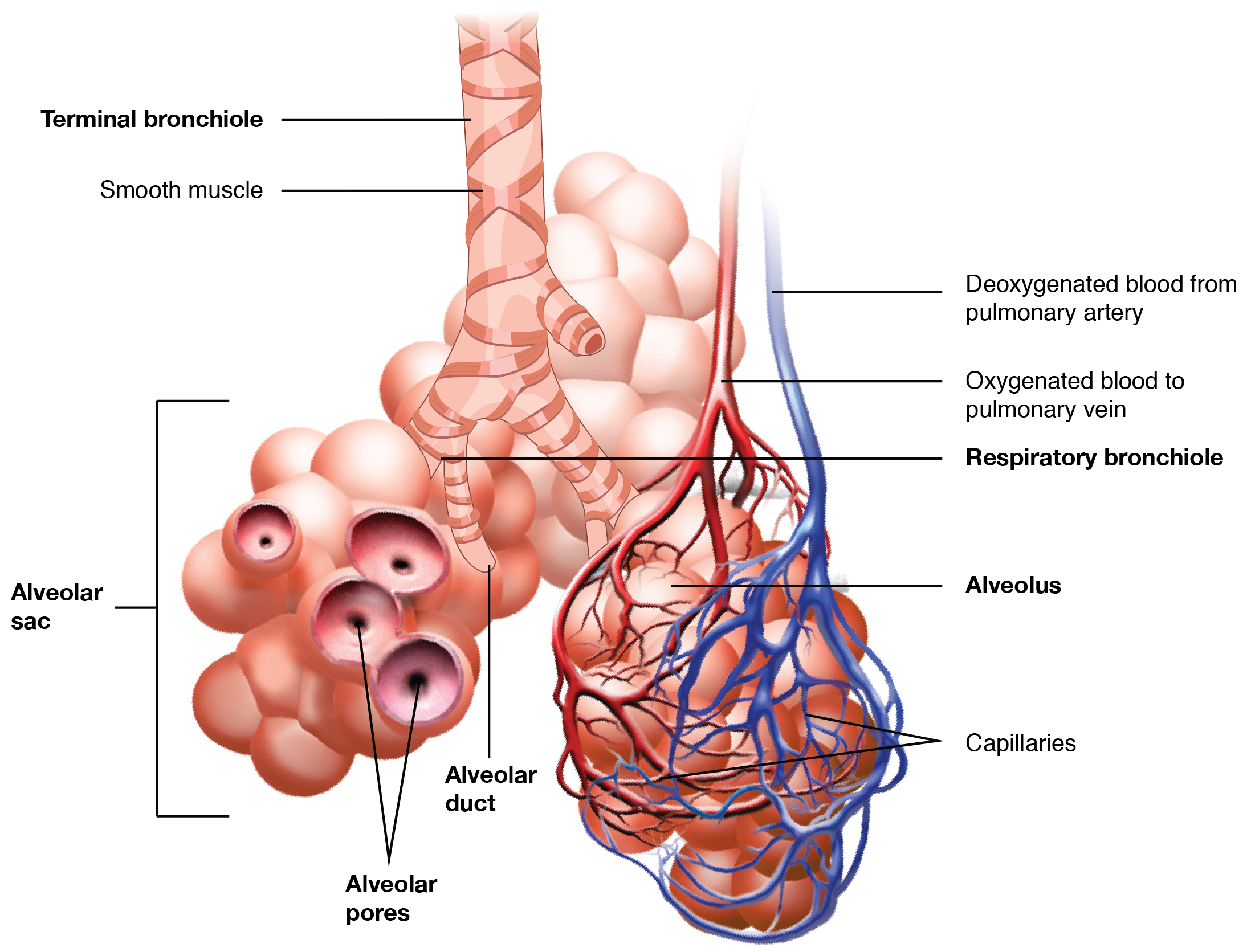
Alveoli
An alveolar duct opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts. An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange. An alveolus is approximately 200 μm in diameter with elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli are connected to their neighbors by alveolar pores, which help maintain equal air pressure throughout the alveoli and lung (see Figure 12.9).
Concept Check
- What are the components of the bronchial tree?
- What is the purpose of cilia?
- Where does gas exchange take place?
Gross Anatomy of the Lungs
The lungs are pyramid-shaped, paired organs that are connected to the trachea by the right and left bronchi; on the inferior surface, the lungs are bordered by the diaphragm. The lungs are enclosed by the pleurae, which are attached to the mediastinum. The right lung is shorter and wider than the left lung, and the left lung occupies a smaller volume than the right. The cardiac notch allows space for the heart (see Figure 12.10). The apex of the lung is the superior region, whereas the base is the opposite region near the diaphragm. The costal surface of the lung borders the ribs. The mediastinal surface faces the midline.

Each lung is composed of smaller units called lobes. Fissures separate these lobes from each other. The right lung consists of three lobes: the superior, middle, and inferior lobes. The left lung consists of two lobes: the superior and inferior lobes. A pulmonary lobule is a subdivision formed as the bronchi branch into bronchioles. Each lobule receives its own large bronchiole that has multiple branches. An interlobular septum is a wall, composed of connective tissue, which separates lobules from one another.
Can you correctly label the respiratory system structures?
Physiology (Function) of the Respiratory System
Blood Supply
The major function of the lungs is to perform gas exchange, which requires blood from the pulmonary circulation.
- This blood supply contains deoxygenated blood and travels to the lungs where erythrocytes pick up oxygen to be transported to tissues throughout the body.
- The pulmonary artery carries deoxygenated, arterial blood to the alveoli.
- The pulmonary artery branches multiple times as it follows the bronchi, and each branch becomes progressively smaller in diameter.
- One arteriole and an accompanying venule supply and drain one pulmonary lobule. As they near the alveoli, the pulmonary arteries become the pulmonary capillary network.
- The pulmonary capillary network consists of tiny vessels with very thin walls that lack smooth muscle fibers.
- The capillaries branch and follow the bronchioles and structure of the alveoli. It is at this point that the capillary wall meets the alveolar wall, creating the respiratory membrane.
- Once the blood is oxygenated, it drains from the alveoli by way of multiple pulmonary veins, which exit the lungs through the hilum.
Nervous Innervation
The blood supply of the lungs plays an important role in gas exchange and serves as a transport system for gases throughout the body. Innervation by both the parasympathetic and sympathetic nervous systems provides an important level of control through dilation and constriction of the airway.
- The parasympathetic system causes bronchoconstriction.
- The sympathetic nervous system stimulates bronchodilation.
Reflexes such as coughing, and the ability of the lungs to regulate oxygen and carbon dioxide levels, also result from autonomic nervous system control. Sensory nerve fibers arise from the vagus nerve, and from the second to fifth thoracic ganglia. The pulmonary plexus is a region on the lung root formed by the entrance of the nerves at the hilum. The nerves then follow the bronchi in the lungs and branch to innervate muscle fibers, glands, and blood vessels.
Pleura of the Lungs
Each lung is enclosed within a cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a serous membrane that surrounds the lung. The right and left pleurae, which enclose the right and left lungs, respectively, are separated by the mediastinum.
The pleurae consist of two layers:
- The visceral pleura is the layer that is superficial to the lungs and extends into and lines the lung fissures (see Figure 12.11).
- The parietal pleura is the outer layer that connects to the thoracic wall, the mediastinum, and the diaphragm.
The visceral and parietal pleurae connect to each other at the hilum. The pleural cavity is the space between the visceral and parietal layers.
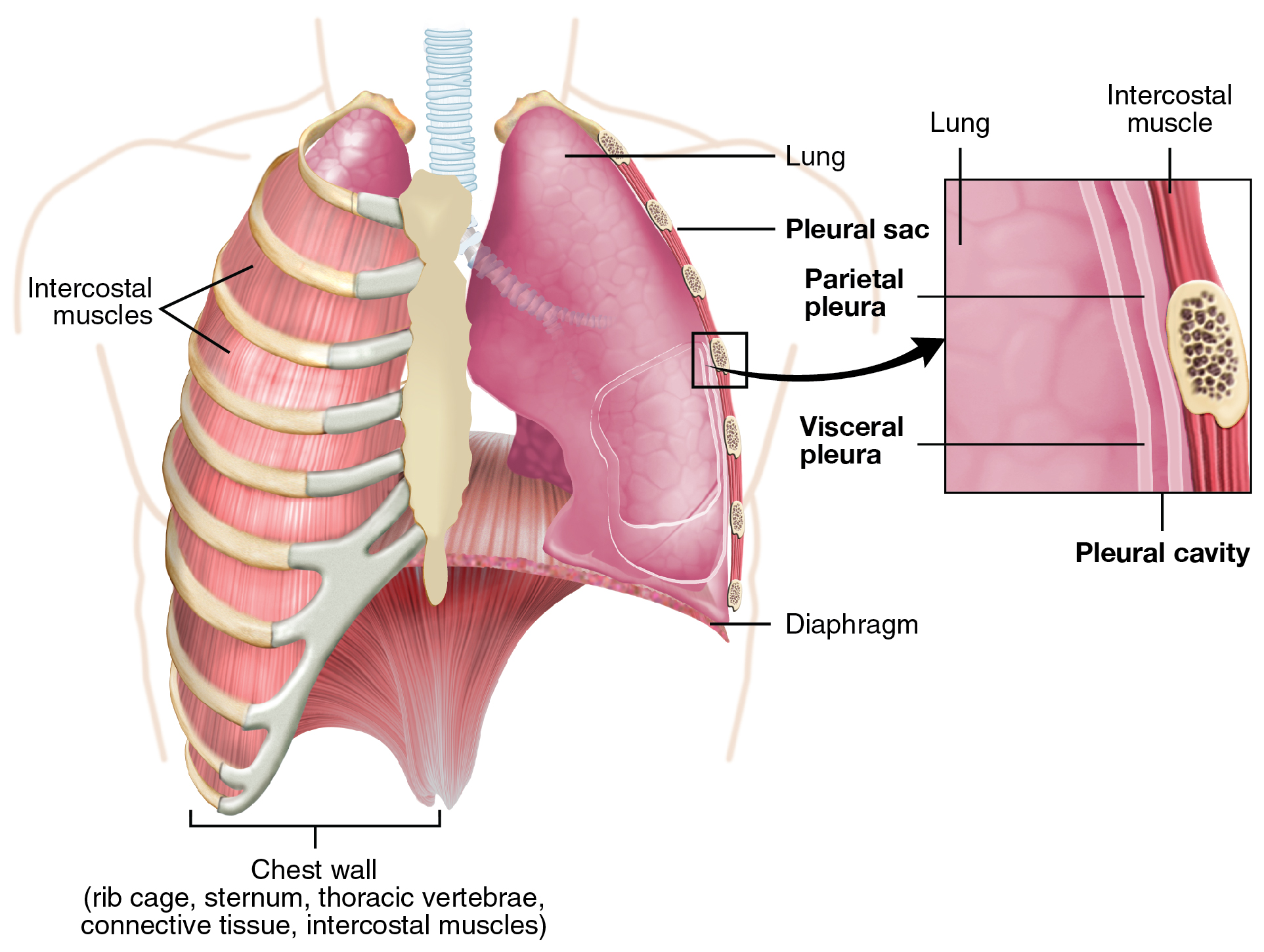
The pleurae perform two major functions:
- Produce pleural fluid that lubricates surfaces, reduces friction to prevent trauma during breathing, and creates surface tension that helps maintain the position of the lungs against the thoracic wall. This adhesive characteristic of the pleural fluid causes the lungs to enlarge when the thoracic wall expands during ventilation, allowing the lungs to fill with air.
- The pleurae also create a division between major organs that prevents interference due to the movement of the organs, while preventing the spread of infection.
Pulmonary Ventilation
The difference in pressures drives pulmonary ventilation because air flows down a pressure gradient, that is, air flows from an area of higher pressure to an area of lower pressure.
- Air flows into the lungs largely due to a difference in pressure; atmospheric pressure is greater than intra-alveolar pressure, and intra-alveolar pressure is greater than intrapleural pressure.
- Air flows out of the lungs during expiration based on the same principle; pressure within the lungs becomes greater than the atmospheric pressure.
Pulmonary ventilation comprises two major steps: inspiration and expiration. Inspiration is the process of having air enter the lungs and expiration is the process of expelling air from the lungs (Figure 12.12). A respiratory cycle is one sequence of inspiration and expiration.
Two muscle groups are used during normal inspiration: the diaphragm and the external intercostal muscles. Additional muscles can be used if a bigger breath is required.
- The diaphragm contracts, it moves inferiorly toward the abdominal cavity, creating a larger thoracic cavity and more space for the lungs.
- The external intercostal muscles contract and move the ribs upward and outward, causing the rib cage to expand, which increases the volume of the thoracic cavity.
Due to the adhesive force of the pleural fluid, the expansion of the thoracic cavity forces the lungs to stretch and expand as well. This increase in volume leads to a decrease in intra-alveolar pressure, creating a pressure lower than atmospheric pressure. As a result, a pressure gradient is created that drives air into the lungs.
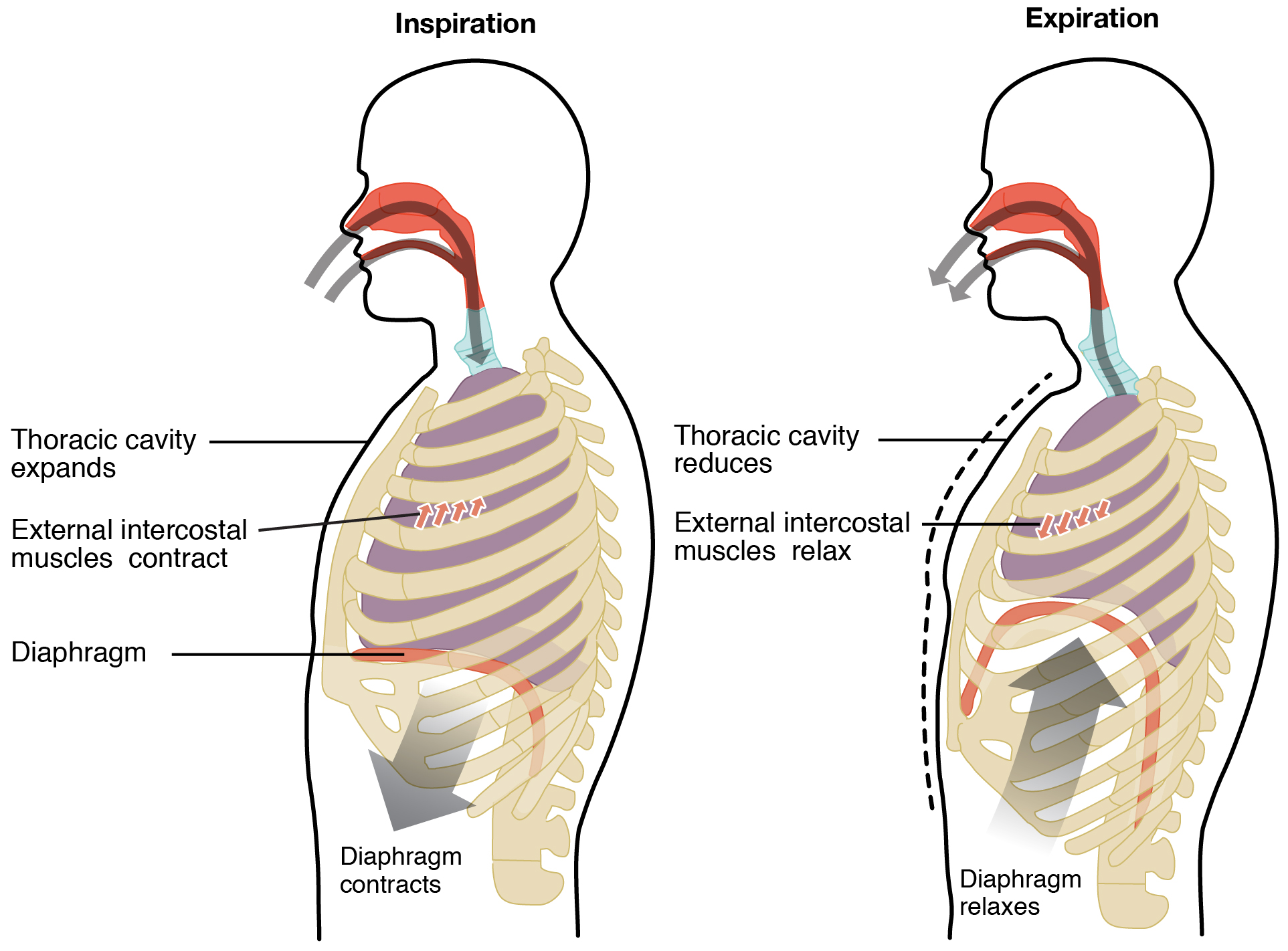
The process of normal expiration is passive, meaning that energy is not required to push air out of the lungs.
- The elasticity of the lung tissue causes the lung to recoil, as the diaphragm and intercostal muscles relax following inspiration.
- The thoracic cavity and lungs decrease in volume, causing an increase in intrapulmonary pressure. The intrapulmonary pressure rises above atmospheric pressure, creating a pressure gradient that causes air to leave the lungs.
There are different types, or modes, of breathing that require a slightly different process to allow inspiration and expiration:
- Quiet breathing, also known as eupnea, is a mode of breathing that occurs at rest and does not require the cognitive thought of the individual. During quiet breathing, the diaphragm and external intercostals must contract.
- Diaphragmatic breathing, also known as deep breathing, requires the diaphragm to contract. As the diaphragm relaxes, air passively leaves the lungs.
- Costal breathing, also known as a shallow breath, requires contraction of the intercostal muscles. As the intercostal muscles relax, air passively leaves the lungs.
- Forced breathing, also known as hyperpnea, is a mode of breathing that can occur during exercise or actions that require the active manipulation of breathing, such as singing.
- During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract.
- During forced inspiration, muscles of the neck contract and lift the thoracic wall, increasing lung volume.
- During forced expiration, accessory muscles of the abdomen contract, forcing abdominal organs upward against the diaphragm. This helps to push the diaphragm further into the thorax, pushing more air out. In addition, accessory muscles help to compress the rib cage, which also reduces the volume of the thoracic cavity.
- During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract.
Concept Check
- Breathing normally, place your hand on your stomach and take in one full respiratory cycle.
- What type of breathing are you doing?
- Keeping your hand on your stomach, take in one large breath and exhale.
- What type of breathing are you doing?
- Complete 10 jumping jacks. Once completed, place your hand on your stomach and take in one full respiratory cycle.
- What type of breathing are you doing?
Respiratory Rate and Control of Ventilation
Breathing usually occurs without thought, although at times you can consciously control it, such as when you swim under water, sing a song, or blow bubbles. The respiratory rate is the total number of breaths that occur each minute. Respiratory rate can be an important indicator of disease, as the rate may increase or decrease during an illness or in a disease condition. The respiratory rate is controlled by the respiratory center located within the medulla oblongata in the brain, which responds primarily to changes in carbon dioxide, oxygen, and pH levels in the blood.
The normal respiratory rate of a child decreases from birth to adolescence:
- A child under 1 year of age has a normal respiratory rate between 30 and 60 breaths per minute.
- By the time a child is about 10 years old, the normal rate is closer to 18 to 30.
- By adolescence, the normal respiratory rate is similar to that of adults, 12 to 18 breaths per minute.
Did you know?
Respiratory rate is the total number of breaths that occur each minute.
Watch this video:
Media 12.1. Respiratory System, Part 2: Crash Course A&P #32 [Online video]. Copyright 2015 by CrashCourse.
Practice Terms Related to the Respiratory System
Common Abbreviations for the Respiratory System
Many terms and phrases related to the respiratory system are abbreviated. Learn these common abbreviations by expanding the list below.
Diseases and Disorders of the Respiratory System
A variety of diseases can affect the respiratory system, such as asthma, emphysema, chronic obstructive pulmonary disorder (COPD), and lung cancer. All of these conditions affect the gas exchange process and result in labored breathing and other difficulties.
The Effects of Second-Hand Tobacco Smoke
- It is estimated that the risk of developing lung cancer is increased by up to 30% in nonsmokers who live with an individual who smokes in the house, as compared to nonsmokers who are not regularly exposed to second-hand smoke.
- Children who live with an individual who smokes inside the home have a larger number of lower respiratory infections, which are associated with hospitalizations, and higher risk of sudden infant death syndrome (SIDS). Second-hand smoke in the home has also been linked to a greater number of ear infections in children, as well as worsening symptoms of asthma.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a term used to represent a number of respiratory diseases, including chronic bronchitis and emphysema. COPD is a chronic condition with most symptoms appearing in middle-aged or older adults. Signs and symptoms include shortness of breath, cough, and sputum production. There is no cure for COPD. Shortness of breath may be controlled with bronchodilators. The best plan is to avoid triggers and getting sick. Clients with COPD are advised to avoid people who are sick, get vaccinated against influenza and pneumococcal pneumonia, and reduce their exposure to pollution and cigarette smoke. While there are several risk factors, as many as 75% of cases are associated with cigarette smoking (National Heart, Lung, and Blood Institute, n.d.). To learn more about COPD, visit the National Heart, Lung, and Blood Institute’s web page.
Asthma
Asthma is a chronic disease characterized by inflammation, edema of the airway, and bronchospasms which can inhibit air from entering the lungs. Bronchospasms can lead to an “asthma attack.” An attack may be triggered by environmental factors such as dust, pollen, pet hair, or dander, changes in the weather, mold, tobacco smoke, and respiratory infections, or by exercise and stress.
Signs and symptoms of an asthma attack involve coughing, shortness of breath, wheezing, and tightness of the chest. Symptoms of a severe asthma attack require immediate medical attention and may include dyspnea that results in cyanotic lips or face, confusion, drowsiness, a rapid pulse, sweating, and severe anxiety. The severity of the condition, frequency of attacks, and identified triggers influence the type of medication that an individual may require. Longer-term treatments are used for those with more severe asthma. Short-term, fast-acting drugs that are used to treat an asthma attack are typically administered via an inhaler. For young children or individuals who have difficulty using an inhaler, asthma medications can be administered via a nebulizer.
Lung Cancer
Lung cancer is a leading cause of cancer death among men and women. Smoking is the most significant risk factor for lung cancer, with 90% of cases in men and 80% of cases in women attributed to tobacco smoking. Signs and symptoms may include shortness of breath, wheezing, blood in the mucus, hoarseness, and trouble swallowing (MedlinePlus, n.d.).
There are two types of lung cancer, small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). Both cancers occur when malignant cells form in the tissues of the lung. If metastasis occurs, lung cancer cells spread to other parts of the body. Treatment will depend on the type of lung cancer and the stage at diagnosis. Treatments may include surgery, chemotherapy, targeted therapy, immunotherapy, and radiation therapy (National Cancer Institute, 2021a, 2021b).
Sleep Apnea
Sleep apnea is a chronic disorder that occurs in children and adults. It is characterized by the cessation of breathing during sleep. These episodes may last for several seconds or several minutes, and may differ in the frequency with which they are experienced. Sleep apnea leads to poor sleep. Signs and symptoms include fatigue, evening napping, irritability, memory problems, morning headaches, and excessive snoring. A diagnosis of sleep apnea is usually done during a sleep study, where the patient is monitored in a sleep laboratory for several nights. Treatment of sleep apnea commonly includes the use of a device called a continuous positive airway pressure (CPAP) machine during sleep. The CPAP machine has a mask that covers the nose, or the nose and mouth, and forces air into the airway at regular intervals. This pressurized air can help to gently force the airway to remain open, allowing more normal ventilation to occur.
Medical Terms in Context
Medical Specialties and Procedures Related to the Respiratory System
Respiratory Therapists (RTs)
Respiratory therapists (RTs) are healthcare professionals that monitor, assess, and treat people who are having problems breathing. RTs must have at least a two-year degree. RTs measure lung capacity, test oxygen and carbon dioxide levels, perform chest physiotherapy to remove mucus from patients’ lungs, and operate ventilator equipment (Bureau of Labor Statistics, 2021). For more information, visit the American Association for Respiratory Care web page.
Thoracic Surgeon
A thoracic surgeon refers to a surgeon who has specialized in either thoracic (chest) surgery or cardiothoracic (heart and chest) surgery (National Cancer Institute, n.d.). To learn about the career path, read this PDF from The Society of Thoracic Surgeons.
Spirometry Testing
Spirometry testing is used to find out how well lungs are working by measuring air volume.
- Respiratory volume describes the amount of air in a given space within the lungs, or which can be moved by the lung, and is dependent on a variety of factors.
- Tidal volume refers to the amount of air that enters the lungs during quiet breathing, whereas inspiratory reserve volume is the amount of air that enters the lungs when a person inhales past the tidal volume.
- Expiratory reserve volume is the extra amount of air that can leave with forceful expiration, following tidal expiration.
- Residual volume is the amount of air that is left in the lungs after expelling the expiratory reserve volume.
- Respiratory capacity is the combination of two or more volumes.
- Anatomical dead space refers to the air within the respiratory structures that never participates in gas exchange, because it does not reach functional alveoli.
- Respiratory rate is the number of breaths taken per minute, which may change during certain diseases or conditions.
Both respiratory rate and depth are controlled by the respiratory centers of the brain, which are stimulated by factors such as chemical and pH changes in the blood. These changes are sensed by central chemoreceptors, which are located in the brain, and peripheral chemoreceptors, which are located in the aortic arch and carotid arteries. A rise in carbon dioxide or a decline in oxygen levels in the blood stimulates an increase in respiratory rate and depth.
Watch this video:
Media 12.3. Peak Flow and Spirometry – Lung Function Tests [Online video]. Copyright 2012 by Oxford Medical Education.
Respiratory System Vocabulary
Adenoidectomy
Excision of the adenoids.
Alveolar duct
Small tube that leads from the terminal bronchiole to the respiratory bronchiole and is the point of attachment for alveoli.
Alveolitis
Inflammation of the alveoli.
Aphonia
Condition of the absence of one’s voice.
Apnea
A temporary absence of respiration.
Asphyxia
Condition caused by a lack of oxygen that leads to impending or actual death.
Aspirate
To withdraw fluid, tissue, or other substances from a body cavity, cyst, or tumor.
Atelectasis
Failure of the lung to expand (inflate) completely.
Autonomic
Involuntary or unconscious.
Benign
Non-cancerous.
Bronchiectasis
Dilation of the bronchi.
Bronchitis
Inflammation of the bronchus.
Bronchodilators
A type of drug that causes small airways in the lungs to open up.
Bronchogenic carcinoma
Cancer that begins in the tissue that lines or covers the airways of the lungs, including small cell and non-small cell lung cancer.
Bronchopneumonia
Inflammation of the lung, particularly the bronchioles and alveoli, that is associated with bronchitis.
Bronchoscope
A thin, tube-like instrument used to examine the inside of the trachea, bronchi, and lungs.
Bronchoscopy
A procedure involving a bronchoscope to examine the inside of the trachea, bronchi, and lungs.
Bronchospasm
Spasmodic contraction of the smooth muscle of the bronchi.
Carcinogen
Any substance that causes cancer.
Cardiac notch
An indentation on the surface of the left lung.
Carina
A ridge at the base of the trachea (windpipe) that separates the openings of the right and left main bronchi (the large air passages that lead from the trachea to the lungs).
Chronic
A condition that lasts a long time with periods of remission and exacerbation.
Computerized tomography (CT)
A noninvasive imaging technique that uses computers to analyze several cross-sectional X-rays in order to reveal minute details about structures in the body.
Conducting zone
The major functions of the conducting zone are to provide a route for incoming and outgoing air, remove debris and pathogens from the incoming air, and warm and humidify the incoming air.
Cyanotic
Pertaining to abnormal color of blue (bluish color, lips and nail beds) caused by deoxygenation.
Defensins
The lysozyme enzyme and proteins which have antibacterial properties.
Diaphragm
A sheet of skeletal muscle separating the thoracic and abdominal cavities that has to contract and relax for you to breathe.
Dysphonia
Condition of difficult speaking, including hoarseness and change in pitch or quality of the voice.
Dyspnea
Difficulty breathing.
Epiglottitis
Inflammation of the epiglottis.
Endoscope
A thin, tube-like instrument used to look at tissues inside the body.
Endoscopy
A procedure that uses an endoscope to examine the inside of the body.
Epiglottis
Leaf-shaped piece of elastic cartilage that is a portion of the larynx that swings to close the trachea during swallowing.
Epistaxis
Nosebleed.
Erythrocytes
Red blood cells.
Eupnea
A mode of breathing that occurs at rest and does not require the cognitive thought of the individual; also known as quiet breathing.
Expiration
Exhalation, or the process of causing air to leave the lungs.
External nose
The surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions.
Fauces
The opening of the oral cavity into the pharynx.
Fibroelastic membrane
A flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages.
Glottis
Composed of the vestibular folds, the true vocal cords, and the space between these folds.
Hard palate
Located at the anterior region of the nasal cavity and is composed of bone.
Hemothorax
Hemorrhage within the pleural cavity.
Hematologist
A doctor who has special training in diagnosing and treating blood disorders.
Hematology
The study of blood and blood-forming issues.
Hilum of the lung
A concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs.
Hypercapnia
Abnormally elevated blood levels of CO2 (carbon dioxide).
Hyperpnea
Forced breathing or breathing that is excessive.
Hypocapnia
Abnormally low blood levels of CO2 (carbon dioxide).
Hypoxemia
Below-normal level of oxygen saturation of blood (typically <95 percent).
Hypoxia
Lack of oxygen supply to the tissues.
Inferior
A position below or lower than another part of the body proper.
Influenza (flu)
An acute viral infection involving the respiratory tract.
Inspiration
Inhalation, or process of breathing air into the lungs.
Laryngeal
Pertaining to the larynx.
Laryngitis
Inflammation of the larynx.
Laryngopharynx
One of the three regions of the pharynx; inferior to the oropharynx and posterior to the larynx.
Laryngoplasty
Surgical repair of the larynx.
Laryngoscope
A thin, tube-like instrument used to examine the larynx.
Laryngoscopy
Examination of the larynx with a mirror or laryngoscope.
Larynx
A cartilaginous structure inferior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs; also known as the voice box.
Lobectomy
Excision of the lobe(s) of an organ.
Lymphocytes
The second most common type of leukocyte and are essential for the immune response.
Malignant
Cancerous.
Mucus
A thick, slippery fluid made by the membranes that line certain organs of the body.
Nasopharyngitis
Inflammation of the nose and pharynx.
Nasopharynx
The upper part of the throat behind the nose. An opening on each side of the nasopharynx leads into the ear.
Nebulizer
A device used to turn liquid into a fine spray.
Nosocomial infection
Infection acquired in hospital.
Oropharynx
A passageway for both air and food; borders the nasopharynx and the oral cavity.
Oximeter
Instrument used to measure the oxygenation of tissues.
Pharyngeal tonsil
The tonsil located at the back of the throat; also known as the adenoid when swollen.
Pharyngitis
Inflammation of the pharynx.
Pharynx
A tube formed by skeletal muscle and lined by mucous membrane that is continuous with that of the nasal cavities; also known as the throat.
Pleural effusion
An abnormal collection of fluid between the thin layers of tissue (pleura) lining the lung and the wall of the chest cavity.
Pleurisy
Inflammation of the pleura.
Pneumoconiosis
A condition caused by the inhalation of dust.
Pneumonectomy
Excision of the lung.
Pneumonia
A severe inflammation of the lungs in which the alveoli (tiny air sacs) are filled with fluid.
Pneumothorax
An abnormal collection of air in the space between the thin layer of tissue that covers the lungs and the chest cavity that can cause all or part of the lung to collapse.
Polysomnography (PSG)
Simultaneous and continuous monitoring of several parameters during sleep to study normal and abnormal sleep.
Posterior
Describes the back or direction toward the back of the body.
Pulmonary artery
Artery that arises from the pulmonary trunk.
Pulmonary edema
Fluid accumulation in alveoli and bronchioles (related to heart failure).
Pulmonary embolism
A blood clot within the lung.
Radiologist
A doctor who has special training in creating and interpreting pictures of areas inside the body.
Radiography
A procedure that uses x-rays to take pictures of areas inside the body.
Radiology
The use of radiation or other imaging technologies to diagnose or treat disease.
Respiratory zone
The respiratory zone includes structures that are directly involved in gas exchange.
Rhinitis
Inflammation of the mucous membranes of the nose.
Rhinoplasty
A plastic surgical operation on the nose, either reconstructive, restorative, or cosmetic.
Rhinorrhea
Excess nasal drainage; also called a “runny nose.”
Septal cartilage
The flexible hyaline cartilage connected to the nasal bone.
Sinusitis
Inflammation of the sinuses.
Soft palate
Located at the posterior portion of the nasal cavity and consists of muscle tissue.
Sonogram
A computer picture of areas inside the body created by high-energy sound waves.
Spirometry
The measurement of volume of air inhaled or exhaled by the lung.
Sputum
Mucus and other matter brought up from the lungs by coughing.
Stethoscope
An instrument is used to hear sounds produced by the heart, lungs, or other parts of the body.
Sympathetic nervous system (SNS)
The division of the nervous system involved in our fight-or-flight responses. It continuously monitors body temperature and initiates appropriate motor responses.
Tachypnea
Rapid breathing.
Thoracalgia
Pain in the chest.
Thoracentesis
Removal of fluid from the pleural cavity through a needle inserted between the ribs.
Thoracic
Pertaining to the chest.
Thoracoscope
A thin tube-like instrument used to examine the inside of the chest.
Thoracoscopy
Examination of the inside of the chest, using a thoracoscope.
Thoracotomy
An operation to open the chest.
Tonsillectomy
Excision of the tonsils.
Tonsillitis
Inflammation of the tonsils.
Tracheitis
Inflammation of the trachea.
Tracheostomy
Surgery to create an opening into the trachea.
Tracheotomy
Surgical incision of the trachea.
Trachea
The windpipe.
Upper respiratory infection
Infection of the nasal cavity, pharynx and larynx cause by a virus.
Uvula
A small bulbous, teardrop-shaped structure located at the apex of the soft palate.
Ventilator
A machine used to help a patient breathe.
Test Yourself
References
Bureau of Labor Statistics. (2021). Respiratory therapists. In Occupational outlook handbook. U.S. Department of Labor. https://www.bls.gov/ooh/healthcare/respiratory-therapists.htm
CrashCourse. (2015, August 24). Respiratory system, part 1: crash course A&P #31 [Video]. YouTube. https://youtu.be/bHZsvBdUC2I
CrashCourse. (2015, August 31). Respiratory system, part 2: crash course A&P #32 [Video]. YouTube. https://youtu.be/Cqt4LjHnMEA
National Cancer Institute. (n.d.). Thoracic surgeon definition. National Institutes of Health, U.S. Department of Health. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/thoracic-surgeon
National Cancer Institute. (2021a). Non-small cell lung cancer treatment (PDQ®)-Patient version. National Institutes of Health, U.S. Department of Health. https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq
National Cancer Institute. (2021b). Small cell cancer treatment (PDQ®)-Patient version. National Institutes of Health, U.S. Department of Health. https://www.cancer.gov/types/lung/patient/small-cell-lung-treatment-pdq
National Heart, Lung, and Blood Institute. (n.d.). COPD. National Institutes of Health, U.S. Department of Health. https://www.nhlbi.nih.gov/health-topics/copd
Oxford Medical Education. (2012, May 13). Peak flow and spirometry – Lung function tests [Video]. YouTube. https://www.youtube.com/watch?v=M4C8EInOMOI
Image Descriptions
Figure 12.1 image description: This figure shows the upper half of the human body. The major organs in the respiratory system are labeled. [Return to Figure 12.1].
Figure 12.2 image description: This figure shows a cross section view of the nose and throat. The major parts are labeled. [Return to Figure 12.2].
Figure 12.3 image description: This figure shows a micrograph of pseudostratified epithelium. [Return to Figure 12.3].
Figure 12.4 image description: This figure shows the side view of the face. The different parts of the pharynx are color-coded and labeled (from the top): nasal cavity, hard palate, soft palate, tongue, epiglottis, larynx, esophagus, trachea. [Return to Figure 12.4].
Figure 12.5 image description: The top panel of this figure shows the anterior view of the larynx, and the bottom panel shows the right lateral view of the larynx. [Return to Figure 12.5].
Figure 12.6 image description: This diagram shows the cross-section of the larynx. The different types of cartilages are labeled (clockwise from top): pyriform fossa, true vocal cord, epiglottis, tongue, glottis, vestibular fold, trachea, esophagus. [Return to Figure 12.6].
Figure 12.7 image description: The top panel of this figure shows the trachea and its organs. The major parts including the larynx, trachea, bronchi, and lungs are labeled. [Return to Figure 12.7].
Figure 12.8 image description: This image shows the bronchioles and alveolar sacs in the lungs and depicts the exchange of oxygenated and deoxygenated blood in the pulmonary blood vessels. [Return to Figure 12.8].
Figure 12.9 image description: This figure shows the detailed structure of the alveolus. The top panel shows the alveolar sacs and the bronchioles. The middle panel shows a magnified view of the alveolus, and the bottom panel shows a micrograph of the cross section of a bronchiole. [Return to Figure 12.9].
Figure 12.10 image description: Diagram of the lungs with the major parts labelled (from top, clockwise): trachea, superior lobe, main bronchus, lobar bronchus, segmental bronchus, inferior lobe, inferior lobe, middle lobe, superior lobe of the left lung. [Return to Figure 12.10].
Figure 12.11 image description: This figure shows the lungs and the chest wall, which protects the lungs, in the left panel. In the right panel, a magnified image shows the pleural cavity and a pleural sac. [Return to Figure 12.11].
Figure 12.12 image description: The left panel of this image shows a person inhaling air and the location of the chest muscles. The right panel shows the person exhaling air and the contraction of the thoracic cavity. [Return to Figure 12.12].

