6.8 Assessing Cerebellar Function
Open Resources for Nursing (Open RN)
The neurological aspect of motor function is based on the activities of the cerebellum. The cerebellum is responsible for equilibrium, coordination, and the smoothness of movement. Specific tests used to evaluate cerebellar function include assessment of gait and balance, pronator drift, the finger-to-nose test, rapid alternating action, and the heel-to-shin test.
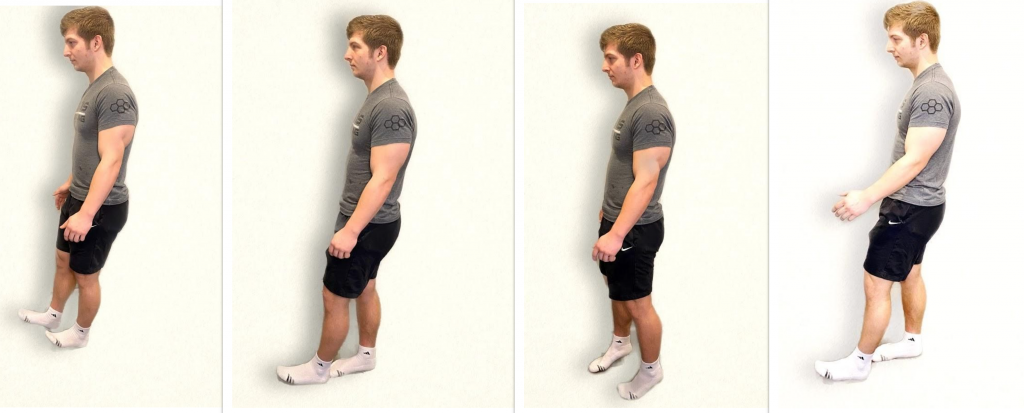
Gait and Balance
When assessing gait and balance, ask the patient to perform the following actions, using an assistive device if needed:
- Walk 10 feet, pivot, and walk back
- Look straight ahead and walk heel to toe
- Walk on tiptoes
- Walk on heels
Steps should be equal with a regular pace while arms are swinging and coordinated with walking. Balance should be maintained. A change in gait, weakness, shuffling, jerky movements, loss of balance, or incoordination of arm swing can indicate a neurological dysfunction. See Figure 6.32[1] for an image of assessing gait and balance.
Pronator Drift
Assessing for pronator drift helps to detect mild upper limb weakness. Ask the patient to close their eyes and extend both arms at 90 degrees at shoulder level with the palms facing upwards. The patient should try to maintain this position for 20 to 30 seconds. Closing the eyes accentuates the effect because the brain is deprived of visual information about the position of the body and must rely on proprioception. Proprioception is the awareness of body position and movement. The expected finding is both arms will maintain this position equally. If the patient is unable to maintain the position, the result is referred to as a positive pronator drift test. Patients with weakness in one arm will not be able to keep the affected arm raised, and ultimately the palm may begin to pronate (palm facing down). In some patients, the arm may remain supinated but will drop lower than the unaffected arm.
Finger-to-Nose Test
The finger-to-nose test assesses equilibrium and coordination. Place the patient in a seated or standing position and ask them to close their eyes. Instruct the patient to extend their arms outward from the sides of the body, and then touch the tip of the nose with the right index finger and return the arm to extended position. Repeat with the left side and continue to repeat touching the nose with alternating movements by both arms.
The expected finding is the patient will smoothly touch the nose with alternating left and right index fingers and return their arms to an extended position repeatedly. An abnormal result occurs when the patient is unable to alternate fingers or demonstrates the inability to touch the nose. For example, the patient may touch the cheek or other part of the face, or movement may be clumsy with stops and restarts. See Figure 6.33[2] for an image of a finger-to-nose test.

Rapid Alternating Action
To perform a rapid alternating action test, place the patient in a seated position with palms down on thighs. Ask the patient to turn their hands so their palms face upwards and then quickly return them to a downward position and repeat. Instruct the patient to alternate this movement at a fast pace. The expected finding is the rhythm, rate, and movement are smooth and coordinated as pace increases. An abnormal finding is when the patient is unable to alternate movements or can only do so at a slow pace. See Figure 6.34[3] for an example of the rapid alternating action test.
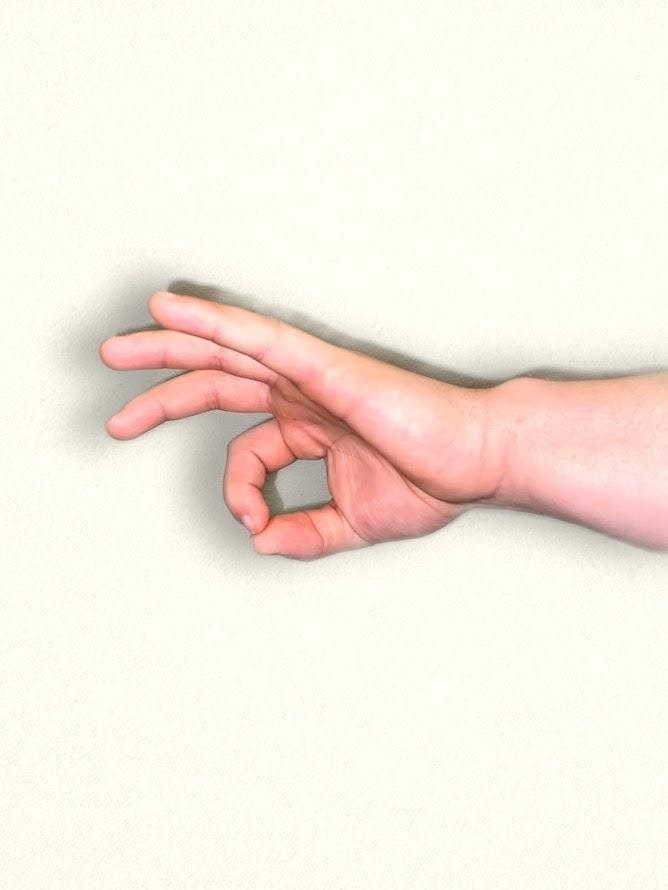
An alternative test is to have the patient touch the thumb to each finger on their hand in sequence and gradually increase the pace. Repeat this test on the other hand. See Figure 6.35[4] for an alternative finger touch test.

Heel-to-Shin Test
To perform a heel-to-shin test, place the patient in a supine position. Ask the patient to place the heel of the right foot just below their left kneecap, and then slide the right heel in a straight line down the shin bone to the ankle. Ask them to repeat this procedure on the left leg. The expected action is a smooth and straight movement of both legs. An abnormal finding is if the heel falls off the lower leg or the patient is not able to complete the movement smoothly in a straight motion. See Figure 6.36[5] for an image of the heel-to-shin test.

Visit Stanford Medicine 25’s “Cerebellum Exam” video on YouTube for a review of cerebellar exam.[6]
- "Neuro Exam image 14.png," "Neuro Exam Image 19.png," "Neuro Exam image 40.png," and "Neuro Exam Image 34.png" by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- "Neuro Exam Image 7.png" by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- "Neuro Exam Image 20.jpg" by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- "Neuro Exam Image 15.png" by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- "Neuro Exam Image 1.png" and "Neuro Exam Image 2.png" by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- Stanford medicine 25. (2014, March 18). Cerebellum exam (Stanford medicine 25). [Video]. YouTube. All rights reserved. https://youtu.be/Imu1kk_gOKA ↵
A person’s sense of their body position.

