17.2 Basic Concepts of Enteral Tubes
Open Resources for Nursing (Open RN)
Gastrointestinal Function
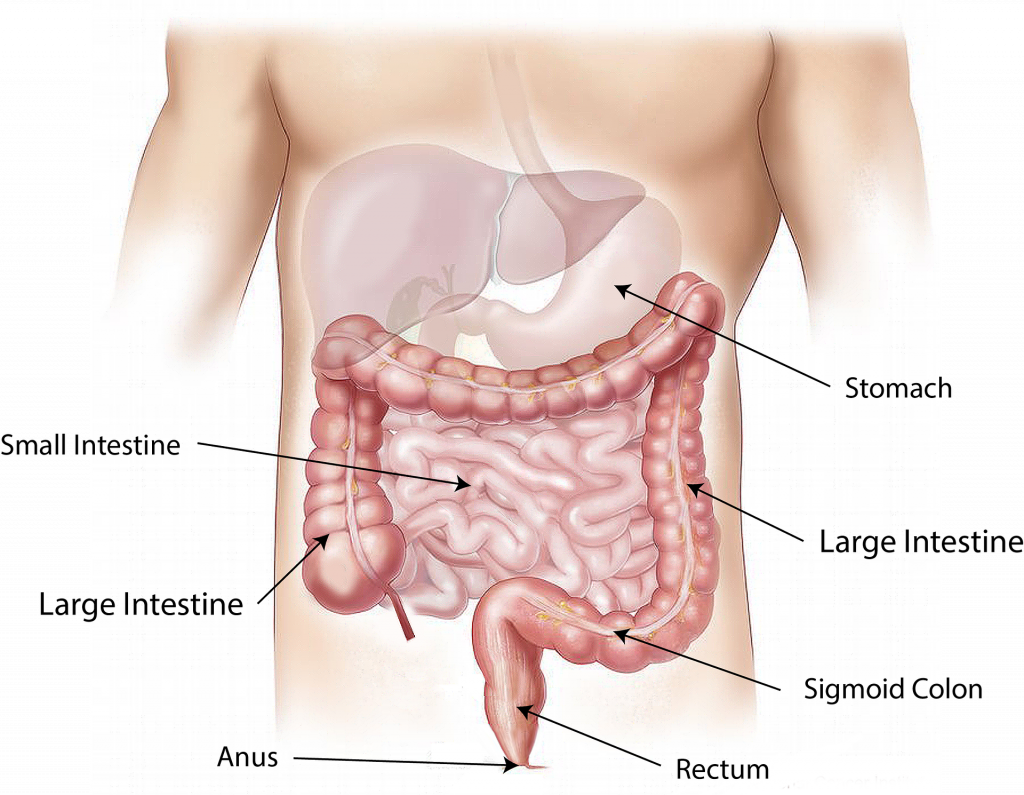
It is important to understand the anatomy and functioning of the gastrointestinal system before administering feedings or medications through an enteral tube. See Figure 17.1[1] for an illustration of the anatomy of the gastrointestinal system.
Enteral Nutrition
Enteral nutrition is indicated for patients who need nutritional supplementation and have a functioning gastrointestinal tract, but cannot swallow food safely. Feedings can be administered via enteral tubes placed into the stomach or into the small intestine (usually the jejunum). For example, enteral feeding is commonly used for patients with the following conditions:
- Impaired swallowing (such as from a stroke or Parkinson’s disease)
- Decreased level of consciousness
- Respiratory distress requiring mechanical ventilation
- Oropharyngeal or esophageal obstruction (such as in head or neck cancer)
- Hypercatabolic states (such as in severe burns)[2]
For short-term feeding, NG tubes are used. If the duration of feeding is longer than four weeks or if access through the nose is contraindicated, a surgery is performed to place the tube directly through the gastrointestinal wall (for example, PEG or PEJ tubes).
Patients who are not candidates for enteral nutrition are prescribed parenteral nutrition. Parenteral nutrition is a concentrated intravenous solution containing glucose, amino acids, minerals, electrolytes, and vitamins. A lipid solution is typically administered as a separate infusion. This combination of solutions is called total parenteral nutrition because it supplies complete nutritional support. Parenteral nutrition is administered via a large central intravenous line, typically the subclavian or internal jugular vein, because it is irritating to the blood vessels.
Types of Enteral Tubes
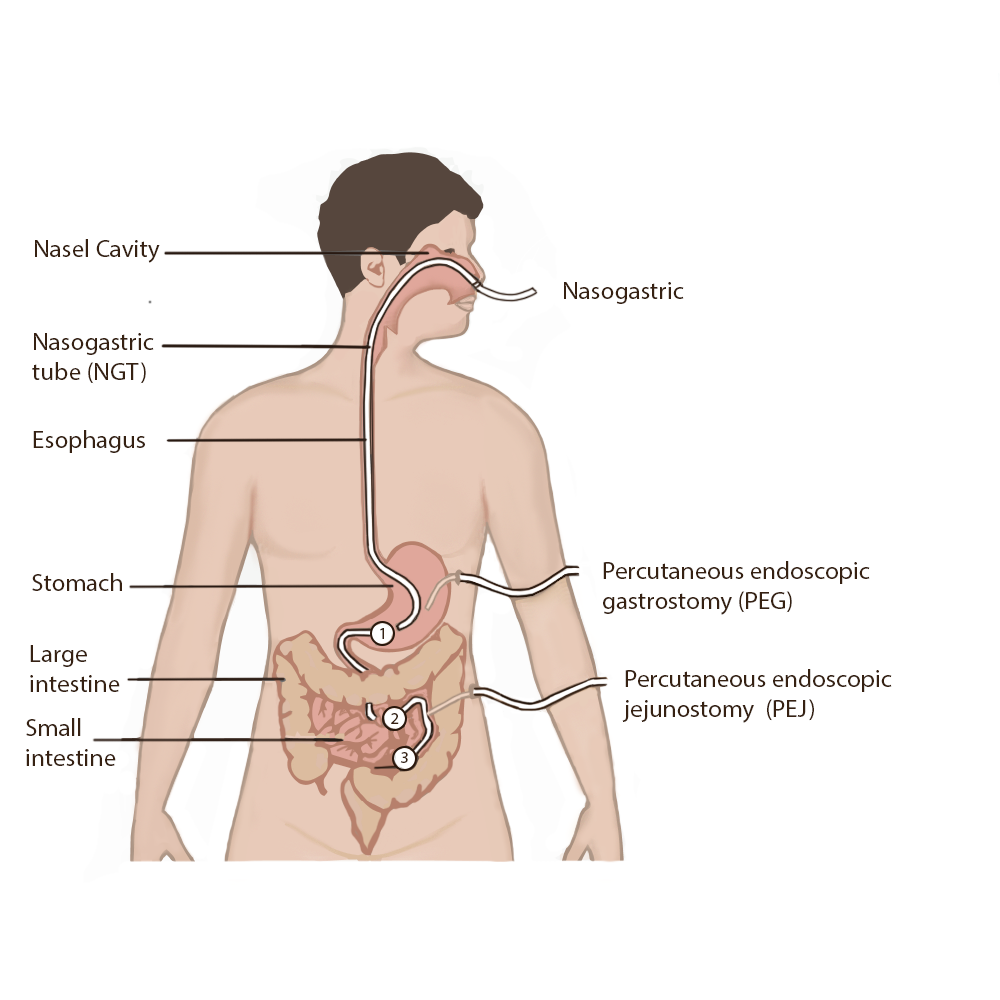
There are several different types of enteral tubes based on their location in the gastrointestinal system, as well as their function. Three commonly used enteral tubes are the nasogastric tube, the percutaneous endoscopic gastrostomy (PEG) tube, and the percutaneous endoscopic jejunostomy (PEJ) tube. See Figure 17.2[3] for an illustration of common enteral tubes. NG tubes are typically used for a short period of time (less than four weeks), whereas PEG and PEJ tubes are inserted for long-term enteral nutrition. Some institutions also place nasoduodenal (ND) tubes to provide long-term enteral nutrition. [4]
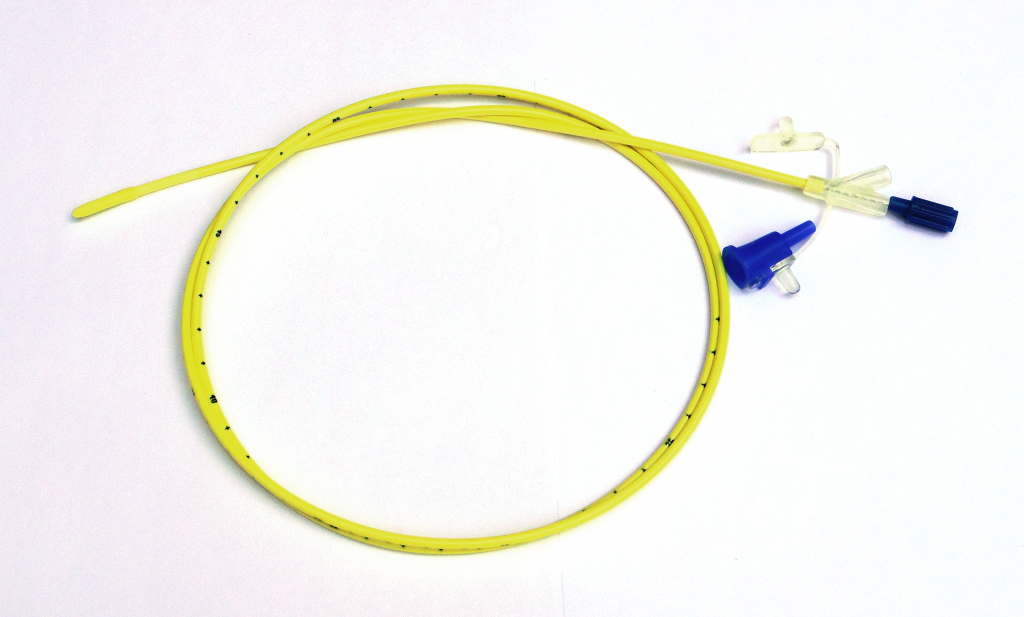
A nasogastric (NG) tube is a single- or double-lumen tube that is inserted into the nasopharynx through the esophagus and into the stomach. NG tubes can be used for feeding, medication administration, and suctioning. NG tubes used for feeding and medication administration are small and flexible, whereas NG tubes used for suctioning are larger and more rigid. NG tubes are secured externally on the patient’s nose or cheek by adhesive tape or a fixation device, so this area should be assessed daily for signs of pressure damage. See Figure 17.3[5] for an image of a small bore feeding tube.
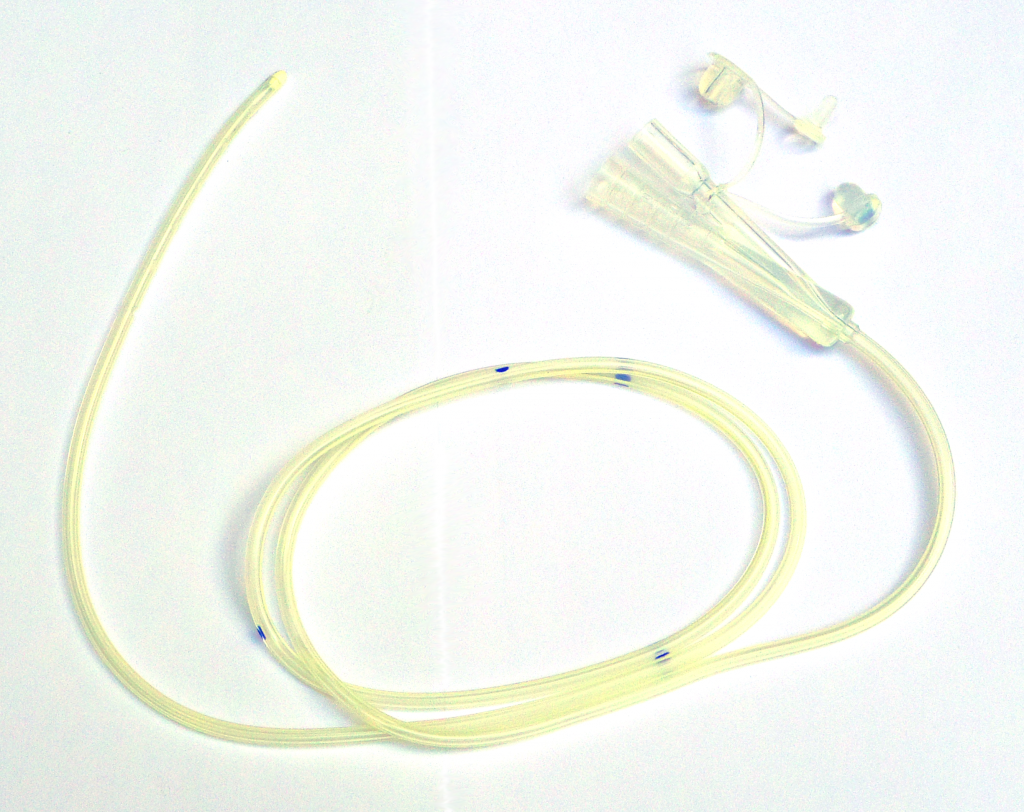
An example of a large bore nasogastric tube is the Salem Sump. Large bore nasogastric tubes, such as the Salem Sump, are used for gastric decompression. The Salem Sump has a double lumen that includes a venting system. One lumen is used to empty the stomach, and the other lumen is used to provide a continuous flow of air. The continuous flow of air reduces negative pressure and prevents gastric mucosa from being drawn into the catheter, which causes mucosal damage. This terminal end also has an anti-reflux valve to prevent gastric secretions from traveling through the wrong lumen. See Figure 17.4[6] for an example of a double-lumen enteral tube.
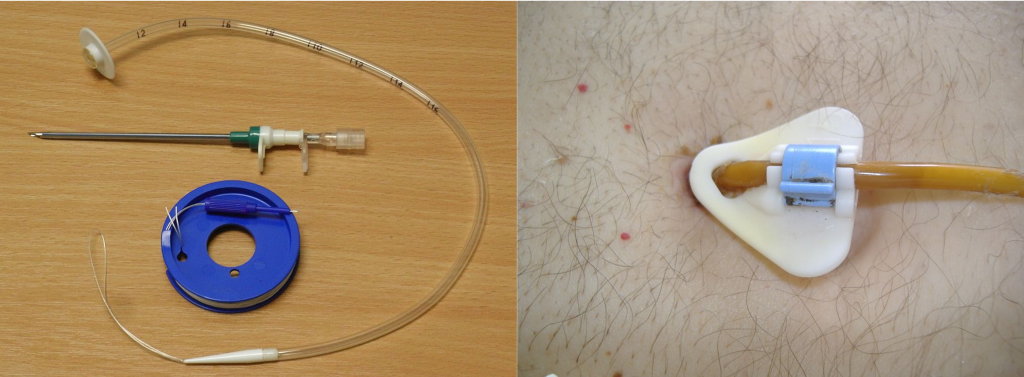
Other types of tubes are placed through the patient’s abdominal wall and are used for long-term enteral feeding. A percutaneous endoscopic gastrostomy (PEG) tube is placed via an endoscopic procedure into the stomach. Alternatively, a percutaneous endoscopic jejunostomy (PEJ) tube is placed in the jejunum of the small intestine for patients who cannot tolerate the administration of enteral formula or medications into the stomach due to medical conditions such as delayed gastric emptying. See Figure 17.5[7] for an image of a PEG tube insertion kit and the appearance of an enteral tube as it exits from a patient’s abdomen.
Assessing Tube Placement
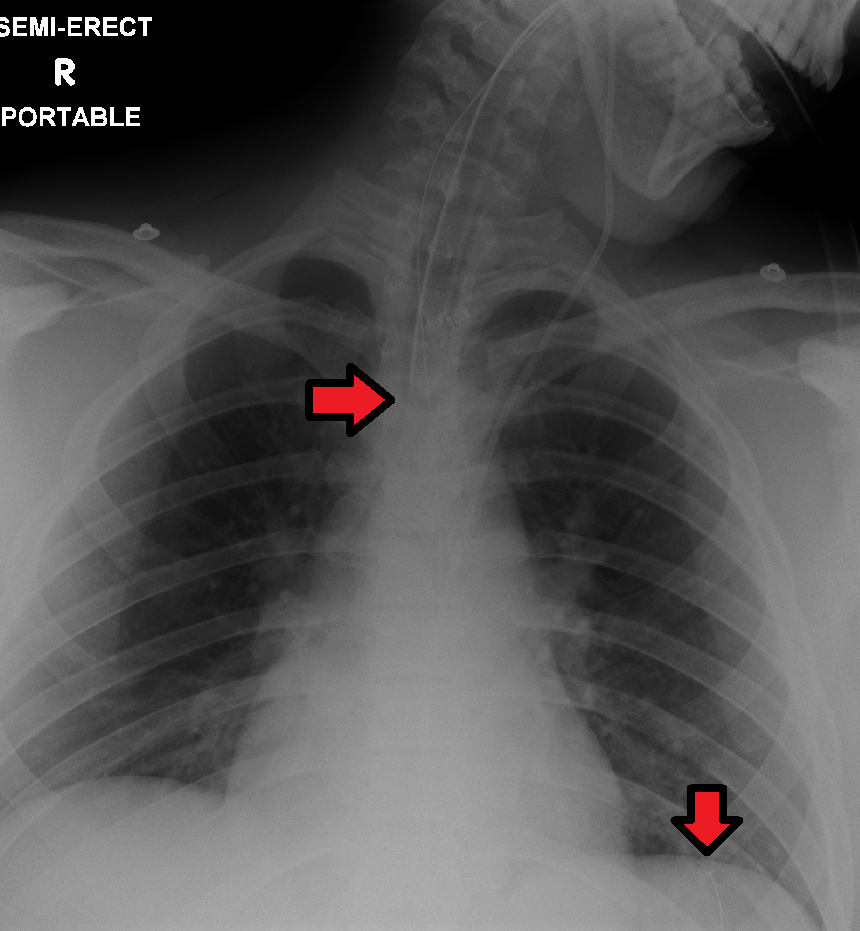
Feedings or medications administered into an incorrectly placed enteral tube result in life-threatening aspiration pneumonia. The placement of an enteral tube is immediately verified after insertion by an X-ray to ensure it has not been inadvertently placed into the trachea and down into the bronchi. See Figure 17.6[8] for an image of an X-ray demonstrating correct placement of an enteral tube in the stomach as indicated by the lower red arrow. (This X-ray also demonstrates an endotracheal tube correctly placed in the trachea as indicated by the top arrow.) After X-ray verification, the tube should be marked with adhesive tape and/or a permanent marker to indicate the point on the tube where the feeding tube enters the nares or penetrates the abdominal wall. This number on the tube at the entry point should be documented in the medical record and communicated during handoff reports. At the start of every shift, nurses evaluate if the incremental marking or external tube length has changed. If a change is observed, bedside tests such as visualization or pH testing of tube aspirate can help determine if the tube has become dislocated. If in doubt, a radiograph should be obtained to determine tube location. [9]
After the initial verification of tube placement by X-ray, it is possible for the tube to migrate out of position due to the patient coughing, vomiting, and moving. For this reason, the nurse must routinely check tube placement before every use. The American Association of Critical‐Care Nursing recommends that the position of a feeding tube should be checked and documented every four hours and prior to the administration of enteral feedings and medications by measuring the visible tube length and comparing it to the length documented during X-ray verification.[10],[11],[12]
Older methods of checking tube placement included observing aspirated GI contents or the administration of air with a syringe while auscultating (commonly referred to as the “whoosh test”). However, research has determined these methods are unreliable and should no longer be used to verify placement.[13],[14]
Checking the pH of aspirated gastric contents is an alternative method to verify placement that may be used in some agencies. Gastric aspirate should have a pH of less than or equal to 5.5 using pH indicator paper that is marked for use with human aspirate. However, caution should be used with this method because enteral formula and some medications alter the gastric pH.[15]
Follow agency policy for assessing and documenting tube placement. Additionally, if the patient develops respiratory symptoms that indicate potential aspiration, immediately notify the provider and withhold enteral feedings and medications until the placement is verified.
Assessing and Cleaning the Tube Insertion Site
The area of tube insertion should be assessed daily for signs of pressure damage. For NG tubes, the adhesive used to secure the tube can be irritating and cause skin breakdown. PEG and PEJ tubes may have fluid seepage around the insertion point that can cause skin breakdown if not cleaned regularly. Follow agency policy for cleansing the external insertion site for PEG and PEJ tubes. Cleansing is typically performed using gauze moistened with water or saline and then allowed to air dry before the fixation plate is repositioned. Because skin surrounding the insertion site is prone to breakdown, barrier cream or dressings may be prescribed to prevent breakdown.[16],[17]
Tube Feeding
Enteral Nutrition (EN) refers to nutrition provided directly into the gastrointestinal (GI) tract through an enteral tube that bypasses the oral cavity. Each year in the United States, over 250,000 hospitalized patients from infants to older adults receive EN. It is also used widely in rehabilitation, long‐term care, and home settings. EN requires a multidisciplinary team approach, including a registered dietician, health care provider, pharmacist, and bedside nurses. The registered dietician performs a nutrition assessment and determines what type of enteral nutrition is appropriate to promote improved patient outcomes. The health care provider writes the order for the enteral nutrition. Prescriptions for enteral nutrition should be reviewed by the nurse for the following components: type of enteral nutrition formula, amount and frequency of free water flushes, route of administration, administration method, and rate. Any concerns about the components of the prescription should be verified with the provider before tube feeding is administered.[18]
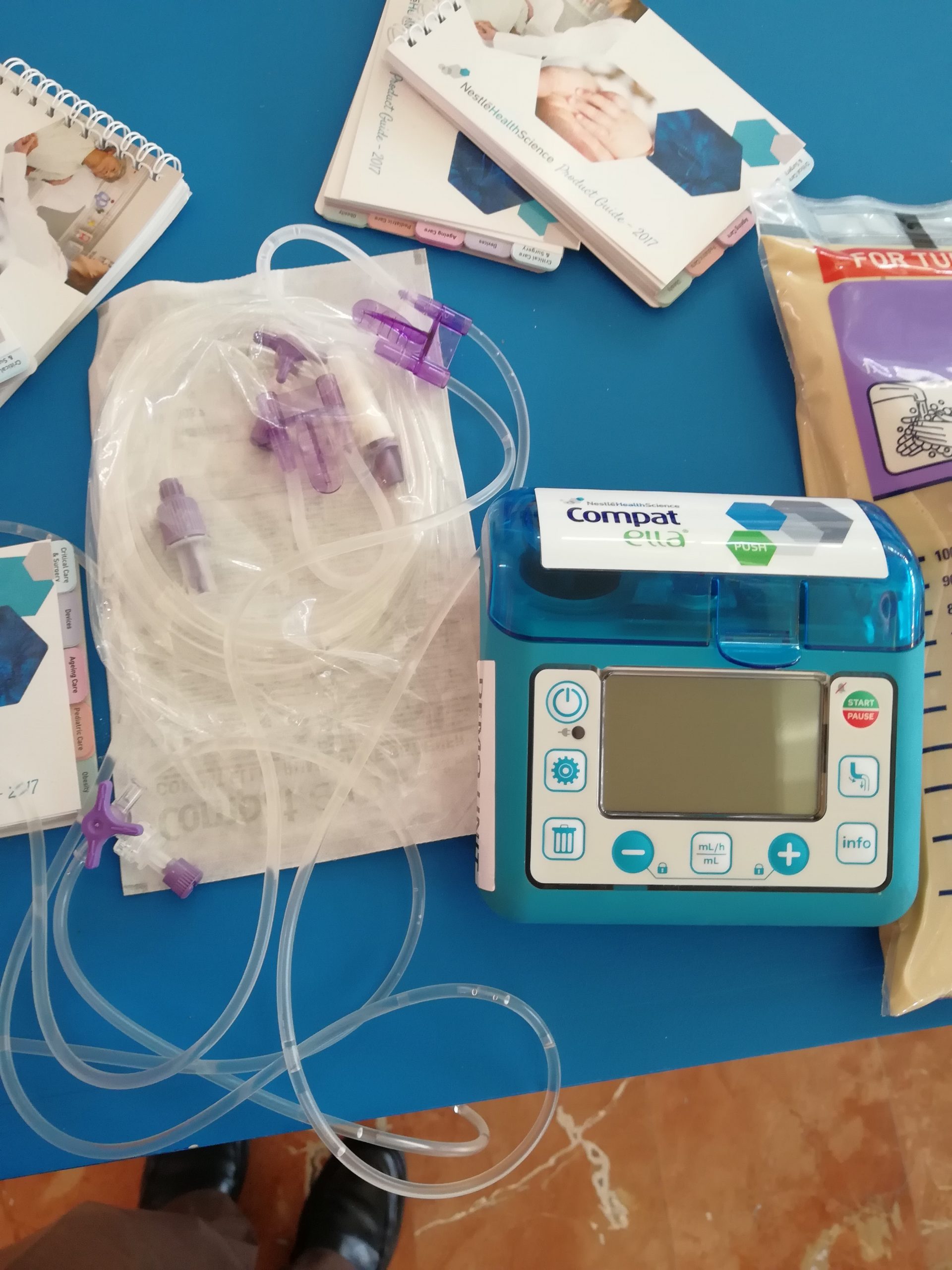
Tube feeding can be administered using gravity to provide a bolus feeding or via a pump to provide continuous or intermittent feeding. Feedings via a pump are set up in mL/hr, with the rate prescribed by the health care provider. See Figure 17.7[19] for an image of an enteral tube feeding pump and the associated tubing. Note that tubing used for enteral feeding is indicated by specific colors (such as purple in Figure 17.7). A global safety initiative, referred to as “EnFit,” is in progress to ensure all devices used with enteral feeding, such as extension sets, syringes, PEG tubes, and NG tubes have specific EnFit ends that can only be used with tube feeding sets. This new safety design will avoid inadvertent administration of enteral feeding into intravenous tubing that can cause life-threatening adverse effects.
Review the “Checklist for NG Tube Enteral Feeding by Gravity with Irrigation” section for additional information regarding administering bolus feedings by gravity.
Life Span Considerations
Enteral feeding is administered to infants and children via a syringe, gravity feeding set, or feeding pump. The method selected is dependent on the nature of the feeding and clinical status of the child.[20]
Complications of Enteral Feeding
The most serious complication of enteral feeding is inadvertent respiratory aspiration of gastric contents, causing life-threatening aspiration pneumonia. Other complications include tube clogging, tubing misconnections, and patient intolerance of enteral feeding.[21]
Reducing Risk of Aspiration
In addition to verifying tube placement as discussed in an earlier section, nurses perform additional interventions to prevent aspiration. The American Association of Critical‐Care Nurses recommends the following guidelines to reduce the risk for aspiration:
- Maintain the head of the bed at 30°-45° unless contraindicated
- Use sedatives as sparingly as possible
- Assess feeding tube placement at four‐hour intervals
- Observe for change in the amount of external length of the tube
- Assess for gastrointestinal intolerance at four‐hour intervals[22]
Measurement of gastric residual volume (GRV) is performed by using a 60-mL syringe to aspirate stomach contents through the tube. It has traditionally been used to assess aspiration risk with associated interventions such as slowing or stopping the enteral feeding. GRVs in the range of 200–500 mL cause interventions such as slowing or stopping the feeding to reduce risk of aspiration. However, according to recent research, it is not appropriate to stop enteral nutrition for GRVs less than 500 mL in the absence of other signs of intolerance because of the impact on the patient’s overall nutritional status. Additionally, the aspiration of gastric residual volumes can contribute to tube clogging.[23] Follow agency policy regarding measuring gastric residual volume and implementing interventions to prevent aspiration.
Managing Tube Clogging
Feeding tubes are prone to clogging for a variety of reasons. The risk of clogging may result from tube properties (such as narrow tube diameter), the tube tip location (stomach vs. small intestine), insufficient water flushes, aspiration for gastric residual volume (GRV), contaminated formula, and incorrect medication preparation and administration. A clogged feeding tube can result in decreased nutrient delivery or delayed administration of medication, and, if not corrected, the patient may require additional surgical intervention to replace the tube.[24]
Research supports using water as the best choice for initial declogging efforts. Instill warm water into the tube using a 60‐mL syringe, and apply a gentle back‐and‐forth motion with the plunger of the syringe. Research shows that the use of cranberry juice and carbonated beverages to flush the tube can worsen tube occlusions because the acidic pH of these fluids can cause proteins in the enteral formula to precipitate within the tube. If water does not work, a pancreatic enzyme solution, an enzymatic declogging kit, or mechanical devices for clearing feeding tubes are the best second‐line options.[25]
To prevent enteral tubes from clogging, it is important to follow these guidelines:
- Flush feeding tubes at a minimum of once a shift.
- Flush feeding tubes immediately before and after intermittent feedings. During continuous feedings, flush at standardized, scheduled intervals.
- Flush feeding tubes before and after medication administration and follow appropriate medication administration practices.
- Limit gastric residual volume checks because the acidic gastric contents may cause protein in enteral formulas to precipitate within the lumen of the tube.[26]
Preventing Tubing Misconnections
In April 2006, The Joint Commission issued a Sentinel Event Alert on tubing misconnections due to enteral feedings being inadvertently infused into intravenous lines with life-threatening results. A color-coded enteral tubing connection design was developed to visually communicate the difference between enteral tubing and intravenous tubing. In addition to tubing design, follow these guidelines to prevent tubing misconnection errors:
- Make tubing connections under proper lighting.
- Do not modify or adapt IV or feeding devices because doing so may compromise the safety features incorporated into their design.
- When making a reconnection, routinely trace lines back to their origins and then ensure that they are secure.
- As part of a hand‐off process, recheck connections and trace all tubes back to their origins.[27]
Managing Intolerances and Imbalances
Patients should be monitored daily for signs of tube feeding intolerance, such as abdominal bloating, nausea, vomiting, diarrhea, cramping, and constipation. If cramping occurs during bolus feedings, it can be helpful to administer the enteral nutritional formula at room temperature to prevent symptoms.[28] Notify the provider of signs of intolerance with anticipated changes in the prescription regarding the type of formula or the rate of administration. Electrolytes and blood glucose levels should also be monitored, as ordered, for signs of imbalances.[29],[30]
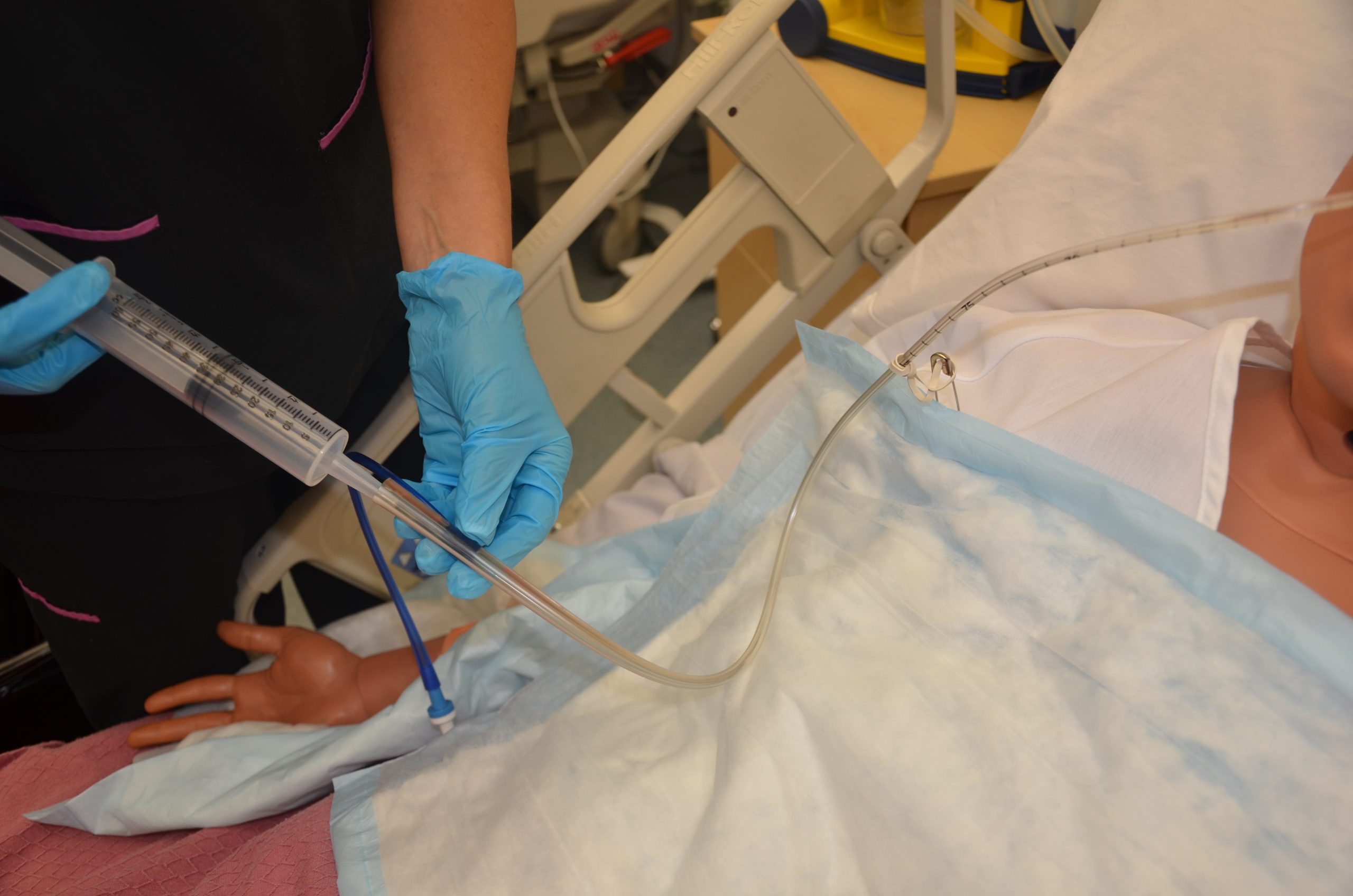
Tube Irrigation
Enteral tubes are routinely flushed to maintain patency. Follow agency policy when flushing a tube. Typically, tap water and a 60-mL syringe are used to flush enteral tubes.[31] See Figure 17.8[32] for an image of a nurse irrigating an NG tube.
The steps for irrigating enteral tubes are typically the following:
- Draw the required amount of water into the 60-mL syringe and dispel excess air.
- If the tube has a clamp, close it.
- Open the distal end of the tube and connect the syringe.
- Open the clamp.
- Administer the water.
- Close the clamp.
- Remove the syringe and refill it with water if indicated.
- Repeat as needed to obtain the desired flushing volume.
- Once completed, remove the syringe, close the tube cap, and reopen the clamp.[33]
Tube Suctioning
NG tubes may be used to remove gastric content, referred to as gastric decompression. In these situations, the stomach is drained by gravity or by connection to a suction pump to prevent nausea, vomiting, gastric distension, or to wash the stomach of toxins. This procedure is commonly used for post-operative patients who have not yet regained peristalsis or for patients with a small bowel obstruction to remove the accumulation of stomach bile. It is also used in the emergency department for patients with some types of poisonings or overdoses and is commonly referred to as “pumping out the stomach.”
For patients receiving suctioning via enteral tubes, the drainage amount and color should be documented every shift.
- “abdomen-intestine-large-small-1698565” by bodymybody is licenced under CCO ↵
- Wireko, B. M., & Bowling, T. (2010). Enteral tube feeding. Clinical Medicine, 10(6), 616–619. https://doi.org/10.7861/clinmedicine.10-6-616 ↵
- “Types and Placement of Enteral Tubes.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Best, C. (2019). Selection and management of commonly used enteral feeding tubes. Nursing Times, 15(3), 43-47. https://www.nursingtimes.net/clinical-archive/nutrition/selection-and-management-of-commonly-used-enteral-feeding-tubes-18-02-2019/ ↵
- “Enteral_feeding_tube_stylet_retracted.png” by Tenbergen is licensed under CC BY-SA 4.0 ↵
- “Silicone_dual_lumen_stomach_tube_with_plug_removed.png” by Tenbergen is licensed under CC BY-SA 4.0 ↵
- “PEG_tube_kit.jpg” by Gilo1969 and “Percutaneous_endoscopic_gastrostomy-tube.jpg” by Pflegewiki-User HoRaMi are licensed under CC BY-SA 3.0 ↵
- "ETTubeandNGtubeMarked.png" by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Lemyze, M. (2010). The placement of nasogastric tubes. CMAJ : Canadian Medical Association Journal , 182(8), 802. https://doi.org/10.1503/cmaj.091099 ↵
- Simons, S. R., & Abdallah, L. M. (2012). Bedside assessment of enteral tube placement: Aligning practice with evidence. American Journal of Nursing, 112(2), 40-46. https://doi.org/10.1097/01.naj.0000411178.07179.68 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Simons, S. R., & Abdallah, L. M. (2012). Bedside assessment of enteral tube placement: Aligning practice with evidence. American Journal of Nursing, 112(2), 40-46. https://doi.org/10.1097/01.naj.0000411178.07179.68 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Best, C. (2019). Selection and management of commonly used enteral feeding tubes. Nursing Times, 15(3), 43-47. https://www.nursingtimes.net/clinical-archive/nutrition/selection-and-management-of-commonly-used-enteral-feeding-tubes-18-02-2019/ ↵
- Blumenstein, I., Shastri, Y. M., & Stein, J. (2014). Gastroenteric tube feeding: Techniques, problems and solutions. World Journal of Gastroenterology, 20(26), 8505–8524. https://doi.org/10.3748/wjg.v20.i26.8505 ↵
- Best, C.(2019). Selection and management of commonly used enteral feeding tubes. Nursing Times, 15(3), 43-47. https://www.nursingtimes.net/clinical-archive/nutrition/selection-and-management-of-commonly-used-enteral-feeding-tubes-18-02-2019/ ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- “Open_system_enteral_feeding.jpg” by Ashashyou is licensed under CC BY-SA 3.0 ↵
- The Royal Children’s Hospital Melbourne. (2017, December). Enteral feeding and medication administration. https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Enteral_feeding_and_medication_administration/ ↵
- Blumenstein, I., Shastri, Y. M., & Stein, J. (2014). Gastroenteric tube feeding: Techniques, problems and solutions. World Journal of Gastroenterology, 20(26), 8505–8524. https://doi.org/10.3748/wjg.v20.i26.8505 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- The Royal Children’s Hospital Melbourne. (2017, December). Enteral feeding and medication administration. https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Enteral_feeding_and_medication_administration/ ↵
- Blumenstein, I., Shastri, Y. M., & Stein, J. (2014). Gastroenteric tube feeding: Techniques, problems and solutions. World Journal of Gastroenterology, 20(26), 8505–8524. https://doi.org/10.3748/wjg.v20.i26.8505 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053. ↵
- Best, C. (2019). Selection and management of commonly used enteral feeding tubes. Nursing Times, 15(3), 43-47. https://www.nursingtimes.net/clinical-archive/nutrition/selection-and-management-of-commonly-used-enteral-feeding-tubes-18-02-2019/ ↵
- “DSC_1667.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/10-2-nasogastric-tubes ↵
- Best, C. (2019). Selection and management of commonly used enteral feeding tubes. Nursing Times, 15(3), 43-47. https://www.nursingtimes.net/clinical-archive/nutrition/selection-and-management-of-commonly-used-enteral-feeding-tubes-18-02-2019/ ↵
Nutrition provided directly into the gastrointestinal (GI) tract through an enteral tube that bypasses the oral cavity.
Stomach contents aspirated with a 60-mL syringe, typically performed for patients receiving enteral feeding to assess aspiration risk with associated interventions such as slowing or stopping tube feeding.

