11.3 Oxygenation Equipment
Open Resources for Nursing (Open RN)
There are several types of equipment a nurse may use when providing oxygen therapy to a patient. Each device is described in detail below.
Pulse Oximeter
A pulse oximeter is a commonly used portable device used to obtain a patient’s oxygen saturation level at the bedside or in a clinic. See Figure 11.6[1] for an image of a portable pulse oximeter. The pulse oximeter, commonly referred to as a “Pulse Ox,” is an electronic device that measures the oxygen saturation of hemoglobin in a patient’s red blood cells, referred to as SpO2. The normal range for SpO2 for an adult without an underlying respiratory condition is above 92%. The pulse oximeter analyzes light produced by the probe as it passes through the finger to determine the saturation level of the hemoglobin molecule. Pulse oximeter probes can be attached to a patient’s finger, forehead, nose, foot, ear, or toe. However, pulse oximetry readings can be inaccurate if the patient is wearing nail polish, has reduced perfusion of the extremities due to a cardiovascular condition, or has other molecules attached to hemoglobin such as in the case of carbon monoxide poisoning.[2]

Oxygen Flow Meter
In inpatient settings, rooms are equipped with wall-mounted oxygen supply outlets that are nationally standardized in a green color, whereas air outlets are standardized with a yellow color. Oxygen flow meters are attached to the green oxygen outlets, and then the oxygenation device is attached to the flow meter. See Figure 11.7[3] for an image of an oxygen flow meter. An oxygen flow meter consists of a glass cylinder containing a steel ball with an opening through which oxygen from the supply source is injected through an adapter. This adapter is commonly referred to as a “tree” because of its appearance. Oxygen is turned on, and the flow rate of oxygen is controlled by turning the green valve on the side of the glass cylinder. The flow rate is set according to the location of a steel ball inside the cylinder and the numbered lines on the glass cylinder. For example, in Figure 11.7, the flow rate is currently set at 2 liter per minute (L/min). It is essential to implement safety precautions whenever oxygen is used. Read more about “Safety with Oxygen Therapy” later in this section.

Portable Oxygen Supply Devices
Portable oxygen tanks are commonly used when transporting a patient to procedures within the hospital or to other agencies. See Figure 11.8[4] for an image of a portable oxygen tank. Oxygenation devices are connected to the tank in a similar manner as the wall-mounted oxygen flow meter. It is crucial for nurses and transporters to ensure the tank has an adequate amount of oxygen for use during transport, is turned on, and the appropriate flow rate is set.

Instead of oxygen tanks, oxygen concentrators are commonly used by patients in their home environment. See Figure 11.9[5] for an image of a home oxygen concentrator. Oxygen concentrators are also produced in portable sizes that are lightweight and easy for patient use while travelling and mobile in the community. See Figure 11.10[6] for an image of a portable oxygen concentrator. Oxygen concentrators work by taking the 21% concentration of oxygen in the air, running it through a molecular sleeve to remove the nitrogen and concentrating the oxygen to a 96% level, thus producing between 1 and 6 liters per minute of oxygen. Oxygen concentrators may provide pulse flow or continuous flow. Pulse flow only occurs on inhalation, whereas continuous flow delivers oxygen throughout the entire breath cycle. Pulse versions are the most lightweight because oxygen is provided only as needed by the patient.[7]


Nasal Cannula
A nasal cannula is the simplest oxygenation device and consists of oxygen tubing connected to two short prongs that are inserted into the patient’s nares. See Figure 11.11[8] for an image of a nasal cannula. The tubing is connected to the flow meter of the oxygen supply source. To prevent drying out the patient’s mucus membranes, humidification may be added for hospitalized patients receiving oxygen flow rates greater than 4 L/minute or for those receiving oxygen therapy for longer periods of time.[9]
Nasal cannulas are the most common type of oxygen equipment. They are used for short- and long-term therapy (i.e., COPD patients) and are best used with stable patients who require low amounts of oxygen.
Flow rate: Nasal cannulas can have a flow rate ranging from 1 to 5 liters per minute (L/min), with a 4% increase in FiO2 for every liter of oxygen, resulting in range of fraction of inspired oxygen (FiO2) levels of 24-44%.
Advantages: Nasal cannulas are easy to use, inexpensive, and disposable. They are convenient because the patient can talk and eat while receiving oxygen.
Limitations: The nasal prongs of nasal cannula are easily dislodged, especially when the patient is sleeping. The tubing placed on the face can cause skin breakdown in the nose and above the ears, so the nurse must vigilantly monitor these areas. Based on agency policy, the nurse should add padding to the oxygen tubing as needed to avoid skin breakdown and may apply a water-based lubricant to prevent drying. However, petroleum-based lubricant should not be used due to the risk of flammability. Nasal cannulas are not as effective if the patient is a mouth breather or has blocked nostrils, a deviated septum, or nasal polyps.[10]

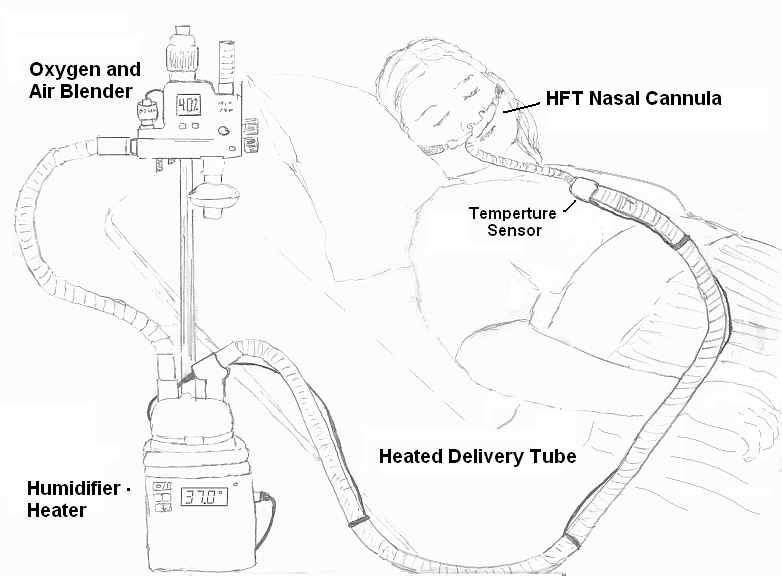
High-Flow Nasal Cannula
High-flow nasal cannula therapy is an oxygen supply system capable of delivering up to 100% humidified and heated oxygen at a flow rate of up to 60 liters per minute.[11] Patients with high-flow nasal cannulas are generally in critical condition and require advanced monitoring. See Figure 11.12[12] for an illustration of a high-flow nasal cannula system that is initially set up by a respiratory therapist and then maintained by a nurse.
Simple Mask
A simple mask fits over the mouth and nose of the patient and contains exhalation ports (i.e., holes on the side of the mask) through which the patient exhales carbon dioxide. These holes should always remain open. The mask is held in place by an elastic band placed around the back of the head. It also has a metal piece near the top that can be pinched and shaped over the patient’s nose to create a better fit. Humidified air may be attached if the oxygen concentrations are drying for the patient. See Figure 11.13[13] for an image of a simple face mask.
Flow Rate: Simple masks should be set to a flow rate of 6 to 10 L/min, resulting in oxygen concentration (FiO2) levels of 35%-50%. The flow rate should never be set below 6 L/min because this can result in the patient rebreathing their exhaled carbon dioxide.
Advantages: Face masks are used to provide moderate oxygen concentrations. Their efficiency in oxygen delivery depends on how well the mask fits and the patient’s respiratory demands.
Disadvantages: Face masks must be removed when eating, and they may feel confining for some patients who feel claustrophobic with the mask on.[14]

Non-Rebreather Mask
A non-rebreather mask consists of a mask attached to a reservoir bag that is attached with tubing to a flow meter. See Figure 11.14[15] for an image of a non-rebreather mask. It has a series of one-way valves between the mask and the bag and also on the covers on the exhalation ports. The reservoir bag should never totally deflate; if the bag deflates, there is a problem and immediate intervention is required. The one-way valves function so that on inspiration, the patient only breathes in from the reservoir bag; on exhalation, carbon dioxide is directed out through the exhalation ports. Non-rebreather masks are used for patients who can breathe on their own but require higher concentrations of oxygen to maintain satisfactory blood oxygenation levels.
Flow rate: The flow rate for a non-rebreather mask should be set to deliver a minimum of 10 to 15 L/minute. The reservoir bag should be inflated prior to placing the mask on the patient. With a good fit, the non-rebreather mask can deliver between 60% and 80% FiO2.
Advantages: Non-rebreather masks deliver high levels of oxygen noninvasively to patients who can otherwise breathe unassisted.
Disadvantages: Due to the one-way valves in non-rebreather masks, there is a high risk of suffocation if the gas flow is interrupted. The mask requires a tight seal and may feel hot and confining to the patient. It will interfere with talking, and the patient cannot eat with the mask on.

Partial Rebreather Mask
The partial rebreather mask looks very similar to the non-rebreather mask. The difference between the masks is a partial rebreather mask does not contain one-way valves, so the patient’s exhaled air mixes with their inhaled air. A partial rebreather mask requires 10-15 L/min of oxygen, but only delivers 35-50% FiO2.
Venturi Mask
Venturi masks are indicated for patients who require a specific amount of supplemental oxygen to avoid complications, such as those with chronic obstructive pulmonary disease (COPD). Different types of adaptors are attached to a face mask that set the flow rate to achieve a specific FiO2 ranging from 24% to 60%. Venturi adapters are typically set up by a respiratory therapist, but in some facilities they may be set up by a nurse according to agency policy.
Flow rate: The flow rate depends on the adaptor and does not correspond to the flow meter. Consult with a respiratory therapist before changing the flow rate.
Advantages: A specific amount of FiO2 is delivered to patients whose breathing status may be affected by high levels of oxygen.
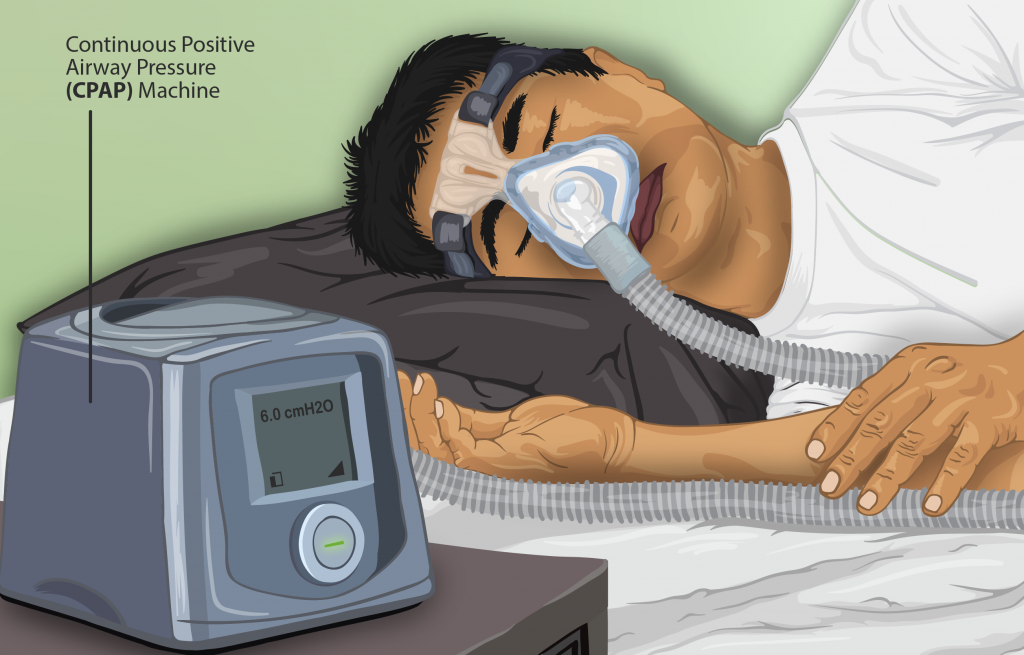
Continuous Positive Airway Pressure (CPAP)
A continuous positive airway pressure (CPAP) device is used for people who are able to breathe spontaneously on their own but need help in keeping their airway unobstructed, such as those with obstructive sleep apnea. (See Table 11.2c in the “Basic Concepts of Oxygenation” section for more information about obstructive sleep apnea.) The CPAP device consists of a special mask that covers the patient’s nose, or nose and mouth, and is attached to a machine that continuously applies mild air pressure to keep the patient’s airways from collapsing.
A prescription is required for a CPAP device in the hospital or patient’s home environment. In the hospital, the FiO2 is set up with the CPAP mask by the respiratory therapist. In a home setting, an adapter is added so that oxygen is attached using a flowmeter with preprogrammed settings so the patient and/or nurse are only required to turn the machine on before sleeping and off upon awakening. It is important to keep the mask and tubing clean to prevent infection, so be sure to follow agency policy for cleaning the equipment regularly. If a humidifier is attached, distilled water or sterile water should be used to fill it, but never tap water. See Figure 11.15[16] for an illustration of a patient wearing a CPAP device while sleeping.
Video Review of FDA Recommendations on How to Use a CPAP Mask[17]
BiPAP
A Bilevel Positive Airway Pressure (BiPAP) device is similar to a CPAP device in that it is used to prevent airways from collapsing, but BiPAP devices have two pressure settings. One setting occurs during inhalation and a lower pressure setting is used during exhalation. Patients using BiPAP devices in their home environment for obstructive sleep apnea often find these two pressures more tolerable because they don’t have to exhale against continuous pressure. In acute-care settings, BiPAP devices are also used for patients in acute respiratory distress as a noninvasive alternative to intubation and mechanical ventilation and are managed by respiratory therapists. BiPAP devices in home settings are set up in a similar manner as CPAP machines for ease of use. See Figure 11.16[18] for an image of a simulated patient wearing a BiPAP mask in a hospital setting with continuous pulse oximetry monitoring.

Bag Valve Mask (Ambu Bag)
A bag valve mask, commonly known as an “Ambu bag,” is a handheld device used in emergency situations for patients who are not breathing (respiratory arrest) or who are not breathing adequately (respiratory failure). In this manner, this device is different from the other devices because it assists with ventilation, the movement of air into and out of the lungs, as well as oxygenation. See Figure 11.17[19] for an image of a bag valve mask. Bag valve masks are produced in different sizes for infants, children, and adults to prevent lung injury, so it is important to use the correct size for the patient.
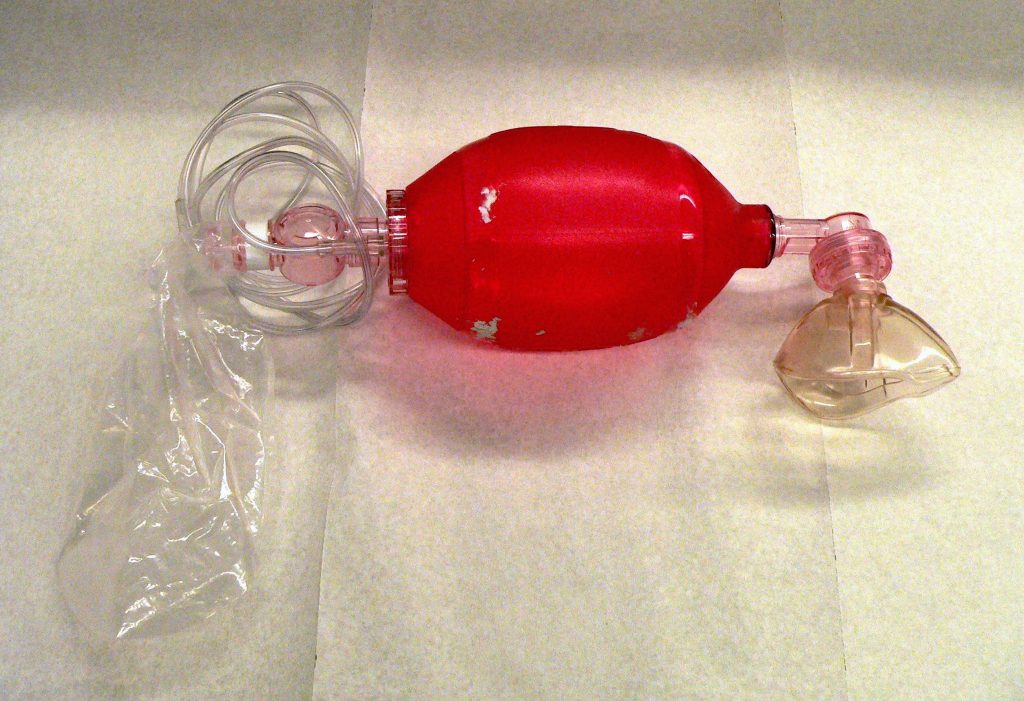
When using a bag mask valve, the rescuer manually compresses the bag to force air into the lungs. Squeezing the bag once every 5 to 6 seconds for an adult or once every 3 seconds for an infant or child provides an adequate respiratory rate. In inpatient settings, the bag mask valve is attached to an oxygen supply to increase the concentration of oxygenation provided with each breath. See Figure 11.18[20] for an illustration of operating a bag valve mask.
It is vital to obtain a tight seal of the mask to the patient’s face, but this is difficult for a single rescuer to achieve. Therefore, two rescuers are recommended; one rescuer performs a jaw thrust maneuver, secures the mask to the patient’s face with both hands, and focuses on maintaining a leak-proof mask seal, while the other rescuer squeezes the bag and focuses on the amount and the timing.
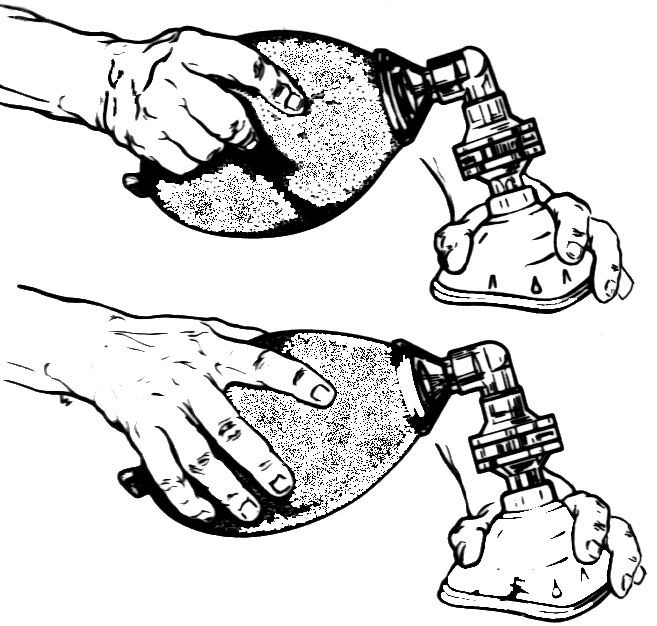
Flow rate: The flow rate for a bag valve mask attached to an oxygen source should be set to 15 L/minute, resulting in FiO2 of 100%.
Advantages: A bag valve mask is portable and provides immediate assistance to patients in respiratory failure or respiratory arrest. It also can be used to hyperoxygenate patients before procedures that can cause hypoxia, such as tracheal suctioning.
Disadvantages: The rate and depth of compression of the bag must be closely monitored to prevent injury to the patient. In the event of respiratory failure when the patient is still breathing, the bag compressions must be coordinated with the patient’s inhalations to ensure that oxygen is delivered and asynchrony of breaths is prevented. Complications may also result from overinflating or overpressurizing the patient. Complications include lung injury or the inflation of the stomach that can lead to aspiration of stomach contents. Additionally, rescuers may tire after a few minutes of manually compressing the bag, resulting in less than optimal ventilation. Alternatively, an endotracheal tube (ET) can be inserted by an advanced practitioner to substitute for the mask portion of this device. See more information about endotracheal tubes below.
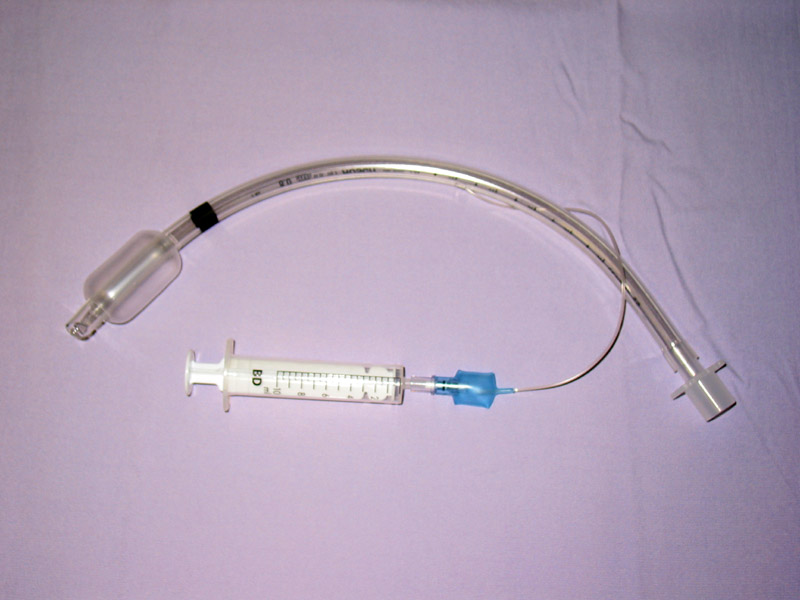
Endotracheal Intubation
When a patient is receiving general anesthesia prior to a procedure or surgery or is experiencing respiratory failure or respiratory arrest, an endotracheal tube (ET) is inserted by an advanced practitioner, such as a respiratory therapist, paramedic, or anesthesiologist, to maintain a secure airway. The ET tube is sealed within the trachea with an inflatable cuff, and oxygen is supplied via a bag valve mask or via mechanical ventilation. See Figure 11.19[21] for an image of a cuffed endotracheal tube.
Mechanical Ventilator
A mechanical ventilator is a machine attached to an endotracheal tube to assist or replace spontaneous breathing. Mechanical ventilation is termed invasive because it requires placement of a device inside the trachea through the mouth, such as an endotracheal tube. Mechanical ventilators are managed by respiratory therapists via protocol or provider order. FiO2 can be set from 21-100%. Nurses collaborate with respiratory therapists and the health care providers regarding the overall care of the patient on a mechanical ventilator. See Figure 11.20[22] for an image of a simulated patient who is intubated with an endotracheal tube and attached to a mechanical ventilator.

Tracheostomy
A tracheostomy is a surgically-made hole called a stoma that goes from the front of the patient’s neck into the trachea. A tracheostomy tube is placed through the stoma and directly into the trachea to maintain an open (patent) airway and to administer oxygen. A tracheostomy may be performed emergently or as a planned procedure. Read more about tracheostomies in the “Tracheostomy Care and Suctioning” chapter.
Flow Rates and Oxygen Percentages
When administering oxygen to a patient, it is important to ensure that oxygen flow rates are appropriately set according to the type of administration device. Review Table 11.3a to review appropriate settings for various types of oxygenation devices.
Table 11.3a Settings of Oxygenation Devices
| Device | Flow Rates and Oxygen Percentage |
|---|---|
| Nasal Cannula | Flow rate: 1-6 L/min
FiO2: 24% to 44% |
| High-Flow Nasal Cannula | Flow rate: up to 60 L/min
FiO2: Up to 100% |
| Simple Mask | Flow rate: 6-10 L/min
FiO2: 28% to 50% |
| Non-Rebreather Mask | Flow rate: 10 to 15 L/min
FiO2: 60-80% Safety Note: The reservoir bag should always be partially inflated. |
| CPAP, BiPAP, Venturi Mask, Mechanical Ventilator | Use the settings provided by the respiratory therapist and/or provider order.
|
| Bag Valve Mask | Flow rate: 15 L/min
FiO2: 100% Squeeze the bag once every 5 to 6 seconds for an adult or once every 3 seconds for an infant or child. |
Safety with Oxygen Therapy
Oxygen therapy supports life, but it also supports fire. While there are many benefits to oxygen therapy, there are also many hazards. Oxygen must be administered cautiously and according to the safety guidelines in Table 11.3b.[23]
Table 11.3b Oxygen Therapy Safety Guidelines
| Guideline | Additional Information |
|---|---|
| Remember that oxygen is a medication. | Oxygen is a medication and should not be adjusted without consultation with a physician or respiratory therapist. |
| Store oxygen cylinders correctly. | When using oxygen cylinders, store them upright, chained, or in appropriate holders so that they will not fall. Full oxygen tanks should be stored separately from partially-full or empty oxygen tanks. |
| Use tank holders appropriately. | When transporting a patient, proper tank holders must be used per Joint Commission guidelines. Tanks should never be placed on the patient’s bed. |
| Do not allow smoking near the oxygen devices. | Oxygen supports combustion. No smoking is permitted around any oxygen delivery devices in the hospital or home environment. |
| Keep oxygen cylinders away from heat sources. | Keep oxygen delivery systems at least 5 feet from any heat source. |
| Check for electrical hazards in the home or hospital prior to use. | Determine that electrical equipment in the room or home is in safe working condition. A small electrical spark in the presence of oxygen will result in a serious fire. The use of a gas stove, kerosene space heater, or smoker is unsafe in the presence of oxygen. Avoid items that may create a spark (e.g., electrical razor, hair dryer, synthetic fabrics that cause static electricity, or mechanical toys) with nasal cannula in use. Petroleum-based lubricants should not be used on the lips or around the nasal cannula. |
| Check levels of oxygen in portable tanks. | Check oxygen levels of portable tanks before transporting a patient to ensure that there is enough oxygen in the tank. |
- “OxyWatch_C20_Pulse_Oximeter.png” by Thinkpaul is licensed under CC BY-SA 3.0 ↵
- American Lung Association. (2020, May 27). Pulse oximetry. https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/pulse-oximetry ↵
- “Oxygen Regulator3I3A1063.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “RECALLED_–_Portable_oxygen_cylinder_units_(8294127015).jpg” by The U.S. Food and Drug Administration is in the Public Domain ↵
- “Invacare Perfecto 2 Oxygen Concentrator.JPG” by BrokenSphere / Wikimedia Commons is licensed under CC BY-SA 3.0 ↵
- “Portable Oxygen Concentrator by Inogen.jpg” by Oxystore is licensed under CC BY-SA 4.0 ↵
- Gibson, C. M. (Ed.). Portable oxygen concentrator. WikiDoc. https://www.wikidoc.org/index.php/Portable_oxygen_concentrator ↵
- “Image00011.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/5-5-oxygen-therapy-systems/ ↵
- Duck, A. (2009, December 14). Does oxygen need humidification? https://www.nursingtimes.net/clinical-archive/respiratory-clinical-archive/does-oxygen-need-humidification-14-12-2009/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Sharma, Danckers, Sanghavi, and Chakraborty and is licensed under CC BY 4.0 ↵
- “HFT diagram.png” by Strangecow is in the Public Domain ↵
- “DSC_2086.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/5-5-oxygen-therapy-systems/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology is licensed under CC BY 4.0 ↵
- “DSC_2083.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/5-5-oxygen-therapy-systems/ ↵
- “Depiction of a sleep apnea patient using a CPAP machine” by https://www.myupchar.com/en is licensed under CC BY 4.0 ↵
- U.S. Food and Drug Administration. (2012, December 12). CPAP tips from FDA. [Video]. YouTube. https://youtu.be/B10ABypyGOo ↵
- “Simulated patient wearing a BiPAP mask” by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Ballon ventilation 1.jpg” by Rama is licensed under CC BY-SA 2.0 FR ↵
- “Resuscitator 3 - Operation (PSF).png” by Pearson Scott Foresman is in the Public Domain ↵
- “Sondeintubation.jpg” by bigomar2 is licensed under CC BY-SA 3.0 ↵
- “Simulated intubated patient on a mechanical ventilator” by ARISE project is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
The mechanical movement of air into and out of the lungs.

